This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To evaluate the initial maternal and perinatal outcomes of fetoscopic laser photocoagulation for the treatment of twin-to-twin transfusion syndrome (TTTS) in a referral center in Brazil.
Methods
This prospective observational study analyzed 24 fetoscopic laser photocoagulation procedures at 18–26 weeks of gestation. TTTS severity was determined using the Quintero classification. Blood vessels that crossed the interamniotic membrane were nonselectively photocoagulated. The χ2 test and Mann-Whitney U test were used for the statistical analysis.
Results
The mean (±standard deviation) age of pregnant women, gestational age at surgery, surgical time, gestational age at birth, and newborn weight were 32.2±4.1 years, 20.7±2.9 weeks, 51.8±16.7 minutes, 30.5±4.1 weeks, and 1,531.0±773.1 g, respectively. Using the Quintero classification, there was a higher percentage of cases in stage III (54.2%), followed by stages IV (20.8%), II (16.7%), and I (8.3%). Ten (41.7%) donor fetuses died and 14 (58.3%) donor fetuses survived until the end of gestation. Placental insertion location (anterior vs. posterior) did not affect the incidence of iatrogenic septostomy, surface bleeding, and premature rupture of membranes until the end of gestation. The death rate of donor and recipient fetuses before 24th gestational week increased with severity of TTTS.
Conclusion
The maternal and perinatal outcomes resulting from the implementation of a new minimally invasive surgical technique are in line with those obtained in major centers worldwide, considering the learning curves and infrastructures.
Keywords: Twin-to-twin transfusion syndrome, Fetoscopy, Lasers, Perinatal mortalities
Introduction
Twin-to-twin transfusion syndrome (TTTS) is a complication that occurs in 10% monochorionic twin pregnancies and has poor prognosis in 80% untreated cases. This progressive disease has a rapid evolution and can lead to the sudden death of one of the fetuses [
1]. In addition, 30% surviving fetuses present with neurodevelopmental retardation because of a combination of factors, including prematurity and perinatal adverse events (AEs) [
2]. In the placenta, there is an unequal blood flow distribution between the fetuses via unidirectional arteriovenous vascular anastomoses that are not compensated by other anastomoses. This causes blood to be transferred from one twin (donor) to the other (recipient). Moreover, the type, location, and number of anastomoses are important factors in the development of these complications [
3].
TTTS treatment has been conducted in the past decades by repeated amniocentesis or interamniotic septostomy; however, the rate of fetal survival is low and the rate of complications is high. The introduction of laser coagulation of chorionic plate anastomoses may improve perinatal outcome and appears to be the best strategy in selected severe cases of TTTS [
4].
The objective of this study was to evaluate the maternal and perinatal outcomes of laser fetoscopy for TTTS treatment in the context of the initial experience of a tertiary referral medical center in Brazil.
Materials and methods
Between November 2012 and November 2016, this prospective observational study analyzed 24 monochorionic and diamniotic twin pregnancies with diagnosis of TTTS at 18–26 weeks of gestation. The patients were selected at the Outpatient Clinic of the Fetal Medicine Service of the Department of Obstetrics of the Paulista School of Medicine, Federal University of São Paulo (EPM-UNIFESP) and at the Santa Joana/Pro-Matre Hospital Complex. The study was approved by the Research Ethics Committee of UNIFESP and all participants signed a consent form (approval number: 1770/11).
The inclusion criterion was monochorionic diamniotic twin pregnancy with a diagnosis of TTTS in stages I (symptomatic), II, III, or IV, using the Quintero classification. The exclusion criteria were the presence of increased risk for preterm birth (cervical length measurement <25 mm by transvaginal ultrasonography), presence of obstetric complications at the time of admission, major fetal malformations diagnosed on ultrasonography or in the postnatal period, and fetal aneuploidy. Gestational age was determined considering the date of the last menstrual period (LMP) in women with regular cycles. For cases of uncertain LMP, gestational age was determined by ultrasonography using crown-rump length (CRL) measurement up to 13th gestational week.
The epidemiological parameters were analyzed in gestations with TTTS and included perinatal characteristics, surgical characteristics, and placental insertion location (anterior vs. posterior). The location of the placenta was subdivided into 2 groups, and the following variables were analyzed in each group: surgical time, laser photocoagulation duration, chorioamniotic membrane separation, the need for iatrogenic septostomy, rate of bleeding at the location of trocar insertion, incidence of placental bleeding, premature rupture of membranes within the first 24 hours after surgery, and premature rupture of membranes until the end of gestation. Moreover, TTTS severity was categorized using the Quintero classification and these subgroups were descriptively analyzed with regard to perinatal characteristics.
All ultrasonography examinations were performed by a single investigator (MMB). The device used in all evaluations was a Voluson 730 Expert (GE Medical System, Milwaukee, WI, USA) equipped with a volumetric convex transducer (RAB 4-8L).
Approximately 1 hour before surgery, prophylactic antibiotic therapy and 100 mg of indomethacin as a tocolytic were administered. Fetoscopy was performed under intradural anesthesia. A 2.0-mm incision was made in the skin for the insertion of the trocar using the Seldinger technique under ultrasonography guidance. A semiflexible endoscope with a diameter of 1.2 mm, a 0° direction of view, and an opening angle of 70–80° was inserted. The sheath was carefully positioned at 20–35° for proper curvature in the anterior placentas. A laser diode with 600- or 800-µm fiber diameter and 40-W power was the preferred choice.
The 2-mm trocar was introduced in the amniotic cavity of the polyhydramnios and directed to the longitudinal axis of the donor fetus by following an imaginary line between the 2 umbilical cord insertions. The insertion of the fetoscope allowed a good visualization of the vascular anastomoses crossing the interamniotic membrane at the chorionic plate.
Nonselective coagulation of the vessels crossing the interamniotic membrane was performed in the following order. First the arteriovenous anastomoses that were deep in the placenta were identified and those with a flow directed toward the recipient fetus were coagulated. This was followed by the coagulation of other arteriovenous anastomoses, and finally that of all the vessels that crossed the interamniotic membrane. Subsequently, a line corresponding to the equator of the placenta joining all previously coagulated vessels was also coagulated. Coagulation was performed at 1.0 cm from the chosen vessel, at a 90° angle, with shots of 3–4 s and a 40-W power output. After the coagulation step, amniocentesis was performed until the fluid volume was normal and then the trocar was removed under ultrasonography guidance.
Ultrasonography follow-up was performed for 24–48 hours after the fetoscopic procedure to identify possible complications, including premature rupture of membranes, preterm placental abruption, and intra-amniotic infection. The patients were maintained at rest in the first 24 hours using analgesics, cefazolin, and tocolytic agents (20-mg nifedipine orally every 8 hours). Corticosteroids (2 doses of 12-mg betamethasone every 24 hours) were used in cases of imminent preterm delivery before of 34 weeks of gestation.
The data were transferred to an Excel spreadsheet (Microsoft Corp., Redmond, WA, USA) and analyzed using the Statistical Package for Social Sciences (SPSS) software, version 15.0 (SPSS Inc., Chicago, IL, USA). The maternal and perinatal variables were expressed as means (±standard deviations) and percentages. The chi-square test was used to assess differences in the distribution of a characteristic categorized as a function of another categorized characteristic and to determine the degree of relationship between the 2 characteristics in independent samples. The nonparametric Mann-Whitney U test was used to compare 2 groups of numerical data and independent samples, and no assumptions were made about the distribution of the analyzed samples.
Results
The mean±standard deviation (range) of maternal age, gestational age at surgery, surgical time, laser photocoagulation duration, gestational age at birth, and newborn weight was 32.2±4.1 years (24–41 years), 20.7±2.9 weeks (17–26 weeks), 51.8±16.7 minutes (30–98 minutes), 36.0±12.6 minutes (15–60 minutes), 30.5±4.1 weeks (22–37 weeks), and 1,531.0±773.0 g (405–2,770 g), respectively.
The analysis of TTTS severity at the time of surgery using the Quintero classification indicated a higher rate of stage III (54.2%), followed by stages IV (20.8%), II (16.7%), and I (8.3%). Fetoscopy was performed in 11 (45.8%) women with anterior placenta and in 13 (54.2%) women with posterior placenta.
Iatrogenic septostomy occurred in 6 fetoscopic procedures (25%), and the amniotic membrane between the fetuses remained intact in 18 procedures (75%). After fetoscopy, the membranes were not separated in 20 (83.3%) pregnancies. Upon introduction of the trocar, bleeding occurred only in 1 (4.2%) case, and trocar introduction was uneventful in 23 (95.8%) cases. During fetoscopy, placental bleeding occurred in 4 (16.7%) cases but did not occur in 20 (83.3%) cases. There was no case of premature rupture of membranes in the first 24 hours after fetoscopy. However, premature rupture of membranes after these first 24 hours occurred in 7 (29.2%) cases whereas the membrane remained intact until the end of gestation in 17 (70.8%) cases. There were no cases of intrauterine infection after fetoscopy. Ten (41.7%) donor fetuses died whereas 14 (58.3%) donor fetuses survived to full term. Eighteen (75%) recipient fetuses survived and 6 (25%) recipient fetuses died. Eight (33.6%) fetuses died before gestational week 24 whereas 3 (12.5%) fetuses died in the neonatal period. In 21 pregnancies (87.5%), at least one of the twins was alive at birth and in 11 (45.8%) pregnancies the 2 fetuses survived. Four (16.7%) cases had TTTS recurrence after fetoscopy whereas twin anemia polycythemia sequence (TAPS) occurred in one (4.2%) case.
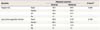
There was no statistically significant effect of placental insertion location (anterior vs. posterior) on surgical time and laser photocoagulation duration, however the surgical time was shorten in cases with placental posterior insertion (
Table 1).
Table 1
Comparative analysis of placental insertion location (anterior vs. posterior), surgical time and laser photocoagulation duration
|
Variables |
Placental insertion |
P-valuea)
|
|
Anterior |
Posterior |
|
Surgical time |
Mean |
54.3 |
49.6 |
0.494 |
|
Median |
50.0 |
45.0 |
|
SD |
18.1 |
15.7 |
|
No. |
11 |
13 |
|
Laser photocoagulation duration |
Mean |
40.9 |
31.9 |
0.106 |
|
Median |
40.0 |
30.0 |
|
SD |
11.3 |
12.5 |
|
No. |
11 |
13 |

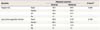
There was no statistically significant effect of placental insertion location (anterior vs. posterior) on the following variables: iatrogenic septostomy, diagnosis of membrane separation, bleeding at the site of trocar insertion, placental bleeding during surgery, diagnosis of premature rupture of membranes in the first 24 hours after fetoscopy, diagnosis of premature rupture of membranes until the end of gestation (
Table 2).
Table 2
Correlation of placental insertion location (anterior vs. posterior) and categorical variables

|
Variables |
Placental insertion |
Total |
P-valuea)
|
|
Anterior |
Posterior |
|
Iatrogenic septostomy |
No |
8 (72.7) |
10 (76.9) |
18 (75.0) |
|
|
Yes |
3 (27.3) |
3 (23.1) |
6 (25.0) |
1.000 |
|
Separation of membranes |
No |
8 (72.7) |
12 (92.3) |
20 (83.3) |
|
|
Yes |
3 (27.3) |
1 (7.7) |
4 (16.7) |
0.464 |
|
Bleeding at the site of trocar insertion |
No |
10 (90.9) |
13 (100) |
23 (95.8) |
|
|
Yes |
1 (9.1) |
0 (0.0) |
1 (4.2) |
0.932 |
|
Placental bleeding |
No |
9 (81.8) |
11 (84.6) |
20 (83.3) |
|
|
Yes |
2 (18.2) |
2 (15.4) |
4 (16.7) |
1.000 |
|
Premature rupture of membranes |
No |
8 (72.7) |
9 (69.2) |
17 (70.8) |
|
|
Yes |
3 (27.3) |
4 (30.8) |
7 (29.2) |
1.000 |
|
Premature rupture of membranes <24 hr |
No |
11 (100) |
13 (100) |
24 (100) |
Not applicable |
|
Total |
11 (100) |
13 (100) |
24 (100) |
|

The rate of death of donor and recipient fetuses before 24th gestational week increased with TTTS severity. The advanced stages of the disease were associated with lower weight because of premature birth (
Table 3).
Table 3
Weight and gestational age at birth at each disease stage using the Quintero classification

|
Quintero classification |
Total |
|
I |
II |
III |
IV |
|
Birth weight (g) |
<1,000 |
0 (0.0) |
0 (0.0) |
4 (30.8) |
4 (80.0) |
8 (33.3) |
|
1,000–1,499 |
0 (0.0) |
1 (25.0) |
2 (15.4) |
1 (20.0) |
4 (16.7) |
|
1,500–1,999 |
0 (0.0) |
2 (50.0) |
0 (0.0) |
0 (0.0) |
2 (8.3) |
|
2,000–2,499 |
1 (50.0) |
1 (25.0) |
6 (46.2) |
0 (0.0) |
8 (33.3) |
|
≥2,500 |
1 (50.0) |
0 (0.0) |
1 (7.7) |
0 (0.0) |
2 (8.3) |
|
<30 |
0 (0.0) |
0 (0.0) |
6 (46.2) |
4 (80.0) |
10 (41.7) |
|
Gestational age at birth (wk) |
30–33.6 |
1 (50.0) |
3 (75.0) |
2 (15.4) |
1 (20.0) |
7 (29.2) |
|
34–36.6 |
0 (0.0) |
1 (25.0) |
3 (23.1) |
0 (0.0) |
4 (16.7) |
|
≥37 |
1 (50.0) |
0 (0.0) |
2 (15.4) |
0 (0.0) |
3 (12.5) |
|
Total |
2 (100) |
4 (100) |
13 (100) |
5 (100) |
24 (100) |

Discussion
Twin monochorionic pregnancies present several complications. The pathophysiology of these complications is usually associated with the vascular architecture of monochorionic placentas, which involves several vascular connections in the blood circulation of both fetuses [
4]. The unequal blood flow distribution causes TTTS and TAPS. However, the selective restriction of fetal growth is associated with the unequal placental sharing.
The unequal blood flow distribution between the fetuses may therefore lead to serious pathologies, the most severe and well-known being TTTS, which affects approximately 10% monochorionic twin pregnancies [
5]. The diagnosis of TTTS is based on the presence of the oligohydramnios-polyhydramnios sequence detected by ultrasonography and is usually made in the second trimester. Oligohydramnios is defined as a larger vertical pocket of ≤2.0 cm in the amniotic cavity of the donor fetus whereas polyhydramnios is defined as a larger vertical pocket of >8.0 or >10 cm after 20 weeks of gestation in the recipient fetus [
1]. According to several studies, the Quintero classification indicates disease severity and is one of the determinants of fetal prognosis. Progression to more advanced stages is associated with worse prognosis, which reinforces the importance of an early diagnosis for a better prognosis [
67].
Since the first fetoscopic laser surgery performed 25 years ago, only a few centers have specialized in minimally invasive fetal surgery. There is a consensus that the best treatment strategy in cases of TTTS is fetoscopic laser photocoagulation. Therefore, an increase in the number of centers specializing in fetoscopy is necessary. Although TTTS is rare, the following factors are essential for achieving the best perinatal results: surgical procedure choice, case selection, the correct timing for the procedure, and adequate postoperative follow-up. In addition, the development of specialized centers in tertiary hospitals is necessary to optimize the treatment of this condition [
8].
In our series case, we used indomethacin as uterine relaxation agent. Usually, indomethacin is the first option for the uterine relaxation before fetoscopic laser surgery for TTTS as described Chang et al. [
9] in a tertiary reference center in Taiwan. In the case of anaphylaxis to indomethacin, nifedipine is the second option [
9]. We did not any case of anaphylaxis to indomethacin in our series case.
Fetoscopic laser photocoagulation is an effective treatment for TTTS but is associated with numerous complications that can occur in the first week after surgery (miscarriage and premature rupture of membranes) or immediately after the intervention (e.g., premature placental detachment and intrauterine death of the fetuses). Late complications include premature rupture of membranes before 32th gestational week, fetal death, recurrence of TTTS and TAPS, and neonatal death [
101112]. In our series, there were no cases of premature rupture of membranes in the first 24 hours after surgery. However, this complication occurred in 29.2% cases after these first 24 hours. This result is similar to that of another study that used the same technique (42%) [
10].
The mean gestational age at birth was 30.5 weeks in our study and 32.4 weeks in the study that used the “Solomon” technique; these results demonstrate the high rate of prematurity associated with this pathology [
10]. The low mean weight of the newborns (1,531.0 g) also indicates the early gestational age at birth. Iatrogenic septostomy occurred in 6 fetoscopy procedures (25% vs. 12% cases in the “Solomon” study). Separation of amniotic membranes occurred in 16.7% cases in our sample and in 5% cases in the “Solomon” study. Placental bleeding during surgery occurred in 16.7% cases in this study vs. 6% cases in the “Solomon” study [
10]. All intraoperative complications increased the risk of AEs. Inadvertent septostomy during surgery results in an iatrogenic monoamniotic pregnancy, which requires the anticipation of delivery to 32–34 weeks of gestation.
There were no cases of infection because of fetoscopy. However, there was a higher number of intrauterine deaths of donor fetuses compared to recipient fetuses, corresponding to 41.7% and 25%, respectively at least one of the fetuses was alive in 87.5% cases and the 2 fetuses were alive at the end of gestation in 45.8% cases. These rates, in particular the likelihood of survival of at least one of the fetuses, are in line with the rates reported in other studies [
131415]. In our study, the survival of both fetuses was lower than that obtained in other studies but was similar to that obtained in the study that described the photocoagulation technique for the first time in 2004 [
7].
Therefore, the diagnosis and treatment of TTTS need to be improved to increase the survival rate of fetuses affected by this condition. The “Solomon” technique appears to contribute to the increase in the survival rate of both fetuses [
1617]. However, the greatest contribution of this technique is the decrease in the recurrence rate of TTTS and the rate of TAPS. In our sample, the recurrence rate of TTTS was 16.7%, compared to only 1% in the Solomon study. The rates of TAPS in our study and in the Solomon study were 4.2% and 3%, respectively. Our results were closer to those of the study that did not use the Solomon technique, in which the recurrence rate of TTTS and the rate of TAPS were 7% and 16%, respectively. However, we reiterate that our study consisted in the initial experience of introducing the surgical technique for the treatment of TTTS.
There were no significant differences between pregnancies with anterior and posterior placenta in relation to the evaluated surgical parameters. These results suggest that the presence of anterior placenta, which was expected to cause greater technical difficulty, was not a causal factor for major complications.
The death rate of donor and recipient fetuses increased with disease severity, i.e., the death rate was higher in stages III and IV, according to the Quintero classification. The survival rate of both fetuses and of at least one fetus because of TTTS was inversely related to disease severity, i.e., the lower the severity using the Quintero classification, the higher the survival rate of the fetuses. In addition, preterm births and low newborn weight increased with increasing disease severity. Therefore, surgical intervention for TTTS treatment should be performed soon after diagnosis to prevent worsening of the clinical status and poor surgical outcomes. However, the correlation between surgical outcomes and the Quintero classification does not indicate a decrease in the number of surviving fetuses with the progression of the disease stages [
18].
A learning curve is unavoidable in the implementation of a minimally invasive fetal surgery programs, and the best perinatal results are observed in the institutions that perform a high number of procedures. In addition, constant exposure to cases and the development of the technique by a small number of surgeons in each institution improve these results [
19]. Therefore, the number of surgeries performed by a surgeon and the hospital infrastructures, including the presence of obstetrics and neonatology teams in the follow-up and discussion of TTTS cases, are vital for the improvement of results.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download