Abstract
The purpose of this study is to develop the treatment planning system (TPS) based on Monte-Carlo simulation for BNCT. In this paper, we will propose a method for dose estimation by Monte-Carlo simulation using the CT image, and will evaluate the accuracy of dose estimation of this TPS. The complicated geometry like a human body allows defining using the lattice function in MCNPX. The results of simulation such as flux or energy deposition averaged over a cell, can be obtained using the features of the tally provided by MCNPX. To assess the dose distribution and therapeutic effect, dose distribution was displayed on the CT image, and dose volume histogram (DVH) was employed in our developed system. The therapeutic effect can be efficiently evaluated by these evaluation tool. Our developed TPS could be effectively performed creating the voxel model from CT image, the estimation of each dose component, and evaluation of the BNCT plan.
The general concept of Neutron Capture Therapy (NCT) was first proposed by Locher in 1936, and NCT which is used boron as the neutron capture element is called Boron Neutron Capture Therapy (BNCT).12) The principle of BNCT is based on the neutron capture reaction, i.e. 10B(n, α)7Li, which is occurred between the neutron and boron incorporated into cancer cells. The alpha particles and recoiling lithium-7 ions are classified in high Linear Energy Transfer (high-LET). The path lengths of these are approximately 10 µm, which is almost equivalent to the mean cell diameter. They can be selectively damage to cancer cells while sparing adjacent normal cells.34)
The dose estimation in BNCT is much more complicated than that in photon and electron radiation therapy, because neutrons produce many different nuclear reactions, each with a different physical and biological dose. Although biological dose in BNCT is necessary to consider strictly divided into each component on the basis of the origin of neutron reactions, the dosimetry could not be applied to it. Therefore, Monte-Carlo simulation that allows to take into account by separating each component is used as a solution of this problem. In order to perform the Monte-Carlo simulation, information of the geometry and structure materials is required. Patient's computed tomography (CT) image is suitable to define them, and is required to accurately predict the dose to the individual patient. The purpose of this study is to develop the treatment planning system (TPS) based on Monte-Carlo simulation for BNCT. In this paper, we will propose a method for dose estimation by Monte-Carlo simulation using the CT image, and will evaluate the accuracy of dose estimation of this TPS.
This study was performed using only mcnpx simulation without any specific dose calculation algorithm. The conventional TPS regarding the neutron beam is based on neutron dose calculation algorithm. However, we used the result of mcnpx simulation for calculating dose distribution originally, the mcnpx simulation tool is optimized to caluculated reaction between the neutron and the material (particle). For our developed TPS for BNCT, Monte Carlo n-particle extended (MCNPX™: Los Alamos National Laboratory, New Mexico, USA)5) version 2.6.0 was used as a dose calculation engine. MCNPX is a general purpose Monte Carlo radiation transport code that tracks nearly all particles at nearly all energies. Most of the TPS which has been developed for BNCT were also used it for dose calculation: the NCTPlan6) is developed at MIT (Massachussets Institute of Technology), the JAERI computational dosimetry system (JCDS)7) is developed at JAEA (Japan Atomic Energy Agency), and the THORplan8) is developed at Tsing Hua University. However, MCNPX has many library regarding particle physics characteristic and mechanism between particles. Therefore, we use the MCNPX for this simulation. MCNPX has the following features:
The complicated geometry like a human body allows defining using the lattice function in MCNPX. In this study, the process for reconstructing the voxel models from patient's CT images is described in the following section. The results of simulation such as flux or energy deposition averaged over a cell, can be obtained using the features of the tally provided by MCNPX. The MCNPX uses pointwise continuous-energy neutron and photon cross sections based on the ENDF/B-VII data library.
In this study, we assumed the treatment for malignant brain tumors. The process for reconstructing the voxel models from patient's CT images consists mainly three parts. Firstly, patient's head CT images with 512×512 pixels is converted into these of 150×150 pixels in this study, because if the miniaturization of the voxel cell size uses for Monte-Carlo simulation, calculation time is increased extremely. The focus of this study is to evaluate the accuracy of calculated doses in our developed TPS, the CT image size is not necessary to maintain the original image size. Secondary, CT images were divided using lattice function in MCNPX into 1×1×1 mm3 voxel cells. Finally, to define the tissue material compositions (i.e., bone, normal tissue, and air) in each voxel, each voxel is classified according to the Hounsfield unit (HU) of them which depends on the primary tissue types. These compositions were defined according to the ICRU report 469) values for the adult patient. These processes are performed automatically. In addition, the tumor region is assumed the sphere with a diameter of 2 cm, which is located from the head surface to a depth of 3 cm in the cerebellum. The 10B concentrations of 25 ppm in brain and 87.5 ppm in tumor were used, so as tumor-normal ratio is 3.5:1. The relative biological effect (RBE)10) for neutrons and photons were determined 3.0 and 1.0, respectively. The compound biological effectiveness (CBE) for tumor is 3.8, and for normal tissue is 1.35.
Monodirectional neutron source of 40 mm length with monoenergetic epithermal neutron 5 keV was located on the right side of the head, and source-to-surface distance is 10 cm with its central axis intercepting the tumor, as shown in Fig. 1. The simulation comprised 800 million independent histories. The nitrogen dose and boron dose were calculated using the track length estimate tally F4 and the kerma factor for each dose components. The photon dose was calculated using the track length estimate of energy deposition tally F6 in unit MeV g−1. Moreover, biological dose is also calculated using the previously mentioned RBE and CBE values.
The voxel model was created from the patients' CT image for dose calculation. Fig. 2 shows (a) original patients' CT image and (b) the reconstructed voxel model. In order to perform the Monte-Carlo simulation in MCNPX, the reconstructed voxel model is automatically converted into text file (i.e., input file).
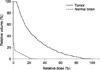
Fig. 3 shows the depth dose profiles for each dose component along the beam centerline. The neutron capture reaction is occurred between the neutron and boron incorporated into cancer cells. In addition, Alpha particles have high-LET and short path length, which can selectively damage cancer cells. The BNCT treatment is mainly affect by the boron dose. Since the composition of each structure is different, the absorbed dose delivered to these greatly differs in BNCT treatment. We found that they could be considered using the MCNPX and patients' CT image.
To assess the dose distribution and therapeutic effect, dose distribution was displayed on the CT image (Fig. 4), and dose volume histogram (DVH) was employed in our developed system (Fig. 5). The therapeutic effect can be efficiently evaluated by these evaluation tool.
The absorbed dose can be estimated by our developed TPS in BNCT treatment. However, we assumed that 10B concentrations are uniformly distributed in the tumor and brain, although they are non-uniformity distributed in practice. Cerullo et al. introduced the data on the in vivo boron distribution, acquired by a positron emission tomography (PET) scan after labeling the BPA (borono-phenylalanine) with the positron emitter 18F.11) To incorporate the data of PET in our TPS would be needed to perform more accurate dose calculation in the near future. Although this study showed the possibility about BNCT treatment dose calculation using MCNPX, the CT pixel size is too high to apply clinical environment. Then, to apply clinical environment, it is essential to simulate dose distribution and dose calculation using clinical CT image.
Figures and Tables
References
1. Sweet WH, Javid M. The possible use of neutron capture isotopes such as boron-10 in the treatment of neoplasms I. Intracranial tumors. J Neurosurg. 1952; 9:200–209.
2. Farr L, Sweet W, Robertson J, et al. Neutron capture therapy with boron in the treatment of glioblastoma multiforme. Am J Roentgenol Radium Ther Nucl Med. 1954; 71:279–291.
3. Raju MR, Eisen Y, Carpenter S, et al. Radiobiology of a particles III. Cell inactivation by α-particle traversals of the cell nucleus. Radiat Res. 1991; 128:204–209.
4. Zhou H, Suzuki M, Randers-Pehrson G, et al. Radiation risk to low fluences of particles may be greater than we thought. Proc Natl Acad Sci. 2001; 98:14410–14415.
5. Pelowitz DB, editor. MCNPX User's Manual Version 2.5.0, LA-CP-05-0369. Los Alamos National Laboratory;2005.
6. Zamenhof R, Redmond E 2nd, Solares G, et al. Monte Carlo-based treatment planning for boron neutron capture therapy using custom designed models automatically generated from CT data. Int J Radiat Oncol Biol Phys. 1996; 35:383–397.

7. Kumada H, Yamamoto K, Matsumura A, et al. Verification of the computational dosimetry system in JAERI (JCDS) for boron neutron capture therapy. Phys Med Biol. 2004; 49:3353–3365.

8. Lin TY, Liu YW. Liu: Development and verification of THORplan.a BNCT treatment planning system for THOR. Appl Radiat Isot. 2011; 69:1878–1881.
9. ICRU. Photon, electron, proton, and neutron interaction data for body tissues, ICRU Report 46. Bethesda, MD: International Commission on Radiation Units and Measurements;1992.
10. Coderre JA, Morris GM. Morris: The radiation biology of boron neutron capture therapy. Radiat Res. 1999; 151:1–18.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download