Abstract
Background
Methods
Results
Figures and Tables
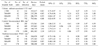
Table 1
Characteristics of hospitals and intensive care units participated in KONIS from July 2015 through June 2016

Table 2
Pooled means of nosocomial infection rates, by number of hospital beds, July 2015 through June 2016

Table 3
Pooled means and percentiles of the decive-associated infection rates, by number of hospital beds, July 2015 through June 2016
*(No. of urinary catheter-associated UTIs/No. of urinary catheter-days)×1,000; †(No. of central line-associated BSIs/No. of central line-days)×1,000; ‡(No. of ventilator-associated PNEUs/No. of ventilator-days)×1,000.
Abbreviations: UTI, urinary tract infection; BSI, bloodstream infection; PNEU, pneumonia; CI, confidence interval.
Table 4
Pooled means and percentiles of the distribution of device-utilization ratios, by number of hospital beds, July 2015 through June 2016
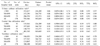
Table 5
Pooled means and percentiles of the distribution of device-associated infection rates, by type of ICU, July 2015 through June 2016

*(No. of urinary catheter-associated UTIs/No. of urinary catheter-days)×1,000; †(No. of central line-associated BSIs/No. of central line-days)×1,000; ‡(No. of ventilator-associated PNEUs/No. of ventilator-days)×1,000.
Abbreviations: ICU, intensive care unit; MICU, medical ICU; MCICU, medical combined ICU; SCICU, surgical combined ICU; SICU, surgical ICU; NSICU, neurosurgical ICU; UTI, urinary tract infection; BSI, bloodstream infection; PNEU, pneumonia; CI, confidence interval.
Table 6
Pooled means and percentiles of the distribution of device-utilization ratios, by type of ICU, July 2015 through June 2016

*(No. of urinary catheter-days/No. of patient-days); †(No. of central line-days/No. of patient-days); ‡(No. of ventilator-days/No. of patient-days).
Abbreviations: ICU, intensive care unit; MICU, medical ICU; MCICU, medical combined ICU; SCICU, surgical combined ICU; SICU, surgical ICU; NSICU, neurosurgical ICU; UTI, urinary tract infection; BSI, bloodstream infection; PNEU, pneumonia; CI, confidence interval.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download