Abstract
Patients who have a lower facial asymmetry with compensatory head posture (developmental facial asymmetry) may have minor temporomandibular (T-M) joint problems and tend to mask their asymmetry by tilting the head for camouflage of their chin deviation. However, this compensatory head posture can give the impression of orbital dystopia and c spine deviation. When these patients undergo bimaxillary orthognathic surgery, orbital canting and head tilting improves gradually without the need for camouflage, and bleary eyes become clearer. We evaluated 13 patients who underwent LeFort I osteotomy combined with bilateral sagittal split osteotomy of the mandible for developmental facial asymmetry to quantitatively observe whole facial postural changes after surgery. Pre-operative and post-operative 1:1 full-face photographs of the patients were analyzed to compare the degrees of head tilting and orbital canting and the sizes of the eye opening. After bimaxillary orthognathic surgery, eye canting decreased from 2.6° to 1.5°, eye and lip lines came closer to parallel, and the degree of head tilting decreased from 3.4° to 1.3°. The eyes also appeared to open wider. Correction of lower facial skeletal asymmetry through bimaxillary orthognathic surgery improved head tilting and orbital canting gradually by eliminating the need of compensatory head posture. Facial expressions also changed as the size of the eyes increased due to the reduction of facial muscle tension caused by T-M joint dysfunction.
Most people have minor to moderate facial asymmetry that has no aesthetic or functional significance. Lower face asymmetry is more easily perceived than asymmetry of the upper face.1 It is reported that occlusal and lip cants are the most noticeable features of facial asymmetry. Although there are no standard criteria for categorizing the severity of asymmetry, Padwa, et al.2 reported that 90% of the general population will notice an occlusal cant that exceeds 4°.
Congenital disorders, such as hemifacial microsomia, and acquired disorders, such as fibrous dysplasia, can cause facial asymmetry. Facial asymmetry with no clear cause is classified as developmental facial asymmetry. Individuals with developmental facial asymmetry have a normal appearance at birth, with the asymmetry gradually becoming apparent as they grow. These individuals tend to mask the asymmetry by adopting a compensatory head posture, such as tilting the head to move the chin point to the midline; however, this tilting may give the false impression of orbital dystopia (Fig. 1). Also individuals with distinct facial asymmetry may have accompanying temporomandibular (T-M) joint dysfunction or minor T-M joint deformities, which can cause headaches, clicking sounds, discomfort with jaw movements, and strain on adjacent musculature. Tension in the orbicularis oris muscle contributes to the appearance of small tired eyes in individuals with facial asymmetry.
Bimaxillary orthognathic surgery is commonly used to correct a canted occlusal plane with rolling movement of the maxilla. After rotation of the maxilla around an anteroposterior axis (rolling) after bimaxillary orthognathic surgery, orbital canting and head tilting become more horizontal, and the tired appearance of the eyes appears to improve. Head posture has been studied in profile photographs, with Capurso, et al.3 showing that forward head and neck posture is the most common alteration. However, patient satisfaction after surgery is more related to the frontal view than the lateral view. Therefore, in this study, we quantitatively analyzed postoperative changes in the frontal view, and evaluated the effect of jaw surgery on other parts of the face, including head posture and eye opening. We hypothesized that surgical correction of lower face asymmetry would eliminate the need for compensatory head posture and resolve pain from T-M joint dysfunction and tension on adjacent musculature, thereby changing facial expressions.
We reviewed the records of 13 patients. Eight female and five male patients who underwent LeFort I osteotomy and coronal rotation, combined with bilateral sagittal split osteotomy of the mandible, for developmental facial asymmetry. This study received Institutional Review Board approval from Yonsei University Medical Center (No. 4-2018-0297). Verbal and written informed consent was obtained from each patient preoperatively. All operations were performed by a single surgeon at Severance Hospital. Average patient age was 22.4 years (range 19–34 years), and average follow-up period was 14.8 months (range 6–31 months). Preoperative and postoperative full-face photographs (1:1 magnification) were taken of the natural head position, with the patients looking straight at the camera with a horizontal visual axis. All photographs were taken at a professional studio at Yonsei Medical Center under the same conditions. We measured the degree of orbital canting, degree of head tilting, and opening of the eyes. All patients had consultations with the dentist and underwent orthodontic treatment prior to the surgery.
All surgical procedures are performed under general nasotracheal anesthesia. Epinephrine (1:100000) mixed with a local anesthetic agent was infiltrated into the surgical field. The mandibular incision was made approximately 10 mm from the lateral aspect of the molars and extended from the mid-ramus to the region of the second molar. A maxillary incision was made 5 mm above the mucogingival junction between the first molars. After completing the subperiosteal elevation, mandibular bony cuts were made. Sagittal split osteotomy was performed with a reciprocating saw above the level of the mandibular foramen, continuing anteriorly along the oblique line and mandibular body, after which the maxillary osteotomy was performed. A transverse osteotomy was done from the pyriform aperture laterally until the cut descended just posterior to the last maxillary molar, dropping through the maxillary tuberosity. The pterygoid osteotomy was performed with a curved osteotome, and the septum was divided with a septal osteotome. Then, the maxilla was downfractured in a slow steady fashion with digital pressure alone or using Rowe disimpaction forceps. The maxilla was placed into its new position using an intermediate splint.
After rotation of the maxillomandibular complex, the maxilla was plated into the correct position, and the intermediate splint was removed. Mandibular splitting was performed with serial osteotomies until the distal segment was placed into the desired occlusion plane using the final splint. The forwardly displaced lateral portion of the ramus was resected with a reciprocating saw, and the condylar head was manually pushed in a clockwise direction (upward and anterior). The lateral portion was fixed with three lag screws. Gingivobuccal incisions were repaired with Vicryl sutures.
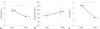
On regular follow-up after surgery, postoperative photographs were taken in the same manner as the preoperative photographs. Preoperative and postoperative orbital canting, head tilting, and opening of the eyes were compared, and the results were expressed as percent change. Orbital canting was evaluated as the angle between true horizontal and the line connecting the centers of the pupils (interpupillary line). Head tilting was evaluated as the angle between true vertical and the line perpendicular to the interpupillary line. The eye was outlined on the full-face photographs, and the opening of the eye was evaluated using the ImageJ program (National Institutes of Health, Bethesda, MD, USA) (Fig. 2).
Photographs taken before surgery and a year after surgery showed marked differences in the patients' overall appearance. Before surgery, average orbital canting was 2.6±1.8° from true horizontal. After surgery, average orbital canting was 1.5±0.6° from true horizontal, which was a 42.8% decrease. Opening of the eye increased from 157±4.8 mm2 to 159.1±8.1 mm2 wide, although this increase was not significant. Before surgery, average head tilt was 3.4±1.9° from true vertical. After surgery, the average head tilt was 1.3±0.7° from true vertical, which was a 60.6% decrease (Fig. 3). As a result, the interpupillary line and the line connecting bilateral oral commissure came closer to parallel and to true horizontal. Interestingly, these changes did not appear immediately after surgery. Instead, the patients' appearances changed gradually over the 12-month postoperative period (Fig. 4).
Symmetry is an important factor in determining facial attractiveness; however, no human face is perfectly symmetrical. Facial asymmetry is a relative distortion of multiple anatomical parts including the eyes, nose, lips, and mandible,4 and the degree of asymmetry determines whether it is perceptible. Song, et al.5 reported that the mouth is the most asymmetrical facial structure, followed by the ears, and the orbits exhibit the lowest degree and incidence of asymmetry. Lee and Yu6 reported that asymmetry of the lower third of the face tends to be perceived more than asymmetry of the upper or middle third of the face. Although position of the mandibular body, gonial angle, and lip canting are all involved in asymmetry of the lower third of the face, chin deviation exerts the greatest influence.
Although there are no standard criteria for the quantitative assessment of facial asymmetry, some studies have reported quantitative data. An occlusal cant of 0° to 3° is observed in normal, healthy individuals.6 Padwa, et al.2 reported that more than half of both untrained and trained observers can notice an asymmetry of 3°, and if the cant is greater than 4°, 90% of untrained observers and 98% of trained observers can detect the asymmetry. Keulen, et al.4 reported that most observers were able to identify a chin deviation of 4 mm or greater.
Most individuals with facial asymmetry experience T-M joint problems. Some may have clinical signs and symptoms related to the masticatory system, such as muscle contraction headache, malocclusion, or bruxism, which can be diagnostic.7 Previous studies have reported abnormal forward head posture in patients with T-M disorders,8910 and Munhoz, et al.11 reported that individuals with more severe T-M joint disorder tend to exhibit cervical spine hyperlordosis. These adaptations in lateral position are thought to be the result of compensatory head posture. According to Bjork12 and Marcotte,13 in individuals with prognathic profiles, the protrusive mandible tends to be masked by forward positioning of the forehead.
Conversely, a convex facial profile is masked somewhat by upward positioning of the chin. In the anteroposterior view, individuals with distinct facial asymmetry often tilt the head to bring the chin point to midline. This head posture leads to the false impression of orbital dystopia due to rotating an untilted orbital plane. In addition, most of these individuals have tired appearing eyes.
Patients with facial asymmetry may desire surgery for aesthetic reasons, even without functional problems with mastication or occlusal position. Facial asymmetry can involve not only the skeleton, but may also have dental and soft tissue components, requiring a combination of orthodontic treatment and orthognathic surgery. Surgical management of facial asymmetry generally requires bimaxillary surgery involving a LeFort I osteotomy and bilateral sagittal split osteotomy. In this study, we found that bimaxillary orthognathic surgery to correct skeletal asymmetry in the lower face can improve head tilting and orbital canting. These changes are presumed to be the result of head posture correction. After surgery, postural compensation by head tilting is unnecessary, and the impression of orbital dystopia disappears. Changes in head and neck posture are presumed to reflect the gradual readjustment of head and neck muscles, such as the sternocleidomastoid muscle.
Results of electromyographic evaluations reveal neuromuscular imbalance in candidates for orthognathic surgery, reflecting asymmetrical development of the temporalis and masseter muscles.14 Goto, et al.15 reported differences in bilateral masseter muscle size in patients with facial asymmetry, and Kiliaridis and Katsaros16 reported that children with untreated unilateral cross bite have a thinner masseter muscle on the affected side. The masticatory muscles are innervated by the trigeminal nerve, which commingles with the nerves of the neck. Therefore, masticatory system dysfunction often leads to problems within cervical structures and vice versa. When the auriculotemporal nerve is constantly stimulated, possibly by internal derangement of the T-M joint, the aberrant signal may cause the head and neck to turn to the ipsilateral side of the stimulation.17 Forward head and neck posture in patients with facial asymmetry can be explained by this neuromuscular relationship. Muscle orientation becomes symmetrical as skeletal components achieve symmetry, and the neural stimulation is relieved by surgery.617 Kiliaridis and Katsaros16 also reported that bilateral differences in muscle size in patients with unilateral cross bite were eliminated after treatment of the malocclusion. A number of studies have reported that orthognathic surgery, in combination with orthodontic treatment, corrects the dentofacial deformity and improves occlusal contacts, masticatory efficiency, bite force, and electromyography activity. The gradual redistribution of jaw muscle activity alters facial alignment and head posture.
Head and neck posture are also connected to the extraocular muscles. Monaco, et al.18 reported that ocular convergence defects are more common in patients with functional mandibular deviation. In this study, we observed that surgical correction of lower face asymmetry improves the appearance of tired eyes, which is presumed to be due to muscle readaptation and pain relief. These changes occur gradually because muscle stress is not relieved immediately, and time is necessary to allow the head and neck muscles to readjust. Patients may feel discomfort early after surgery as this realignment takes place.19
Although not evaluated in this study, changes in lip cant after bimaxillary surgery have been reported. Lip cant is caused by differences in height of the bilateral oral commissures, determined by the upward pull of the zygomaticus major and levator anguli oris muscles and the downward pull of the depressor anguli oris muscle.20 During orthognathic surgery, the depressor anguli oris muscle attachment is displaced to correct lip cant.
One limitation of this study is the lack of precise method to measure head and cervical posture. A device to help patients maintain stillness during the full-face photographs is needed for reproducibility. In addition, magnetic resonance imaging or computed tomography scans could provide more precise estimates of hard and soft tissue changes.
Figures and Tables
Fig. 1
Schematic illustrations. (A) Natural head position. In the natural head position with a horizontal visual axis, a difference in height of the oral commissures is apparent. (B) Compensatory head posture. Tilting the head camouflages the lower face asymmetry, but results in canting of the orbital plane.
Fig. 2
In the compensatory head position, orbital canting was evaluated as the angle between true horizontal (left, dotted blue line) and the line connecting the centers of the pupils (left, linear blue line). The opening of the eye was calculated using the ImageJ program (National Institute of Health) by tracing the margin along the upper and lower eyelid (right, green area). Head tilting was evaluated as the angle between true vertical (left, dotted yellow line) and the line perpendicular to the interpupillary line (left, linear yellow line).

ACKNOWLEDGEMENTS
The authors thank Mr. Dong-Su Jang, Research Assistant, Department of Anatomy, Yonsei University College of Medicine, Seoul, Korea, for his help with the figures.
References
1. Kim YH, Jeon J, Rhee JT, Hong J. Change of lip cant after bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 2010; 68:1106–1111.

2. Padwa BL, Kaiser MO, Kaban LB. Occlusal cant in the frontal plane as a reflection of facial asymmetry. J Oral Maxillofac Surg. 1997; 55:811–816.

3. Capurso U, Garino GB, Rotolo L, Verna C. [Radiographic screening of asymmetry and postural changes in orthodontic patients]. Mondo Ortod. 1990; 15:313–320.
4. van Keulen C, Martens G, Dermaut L. Unilateral posterior crossbite and chin deviation: is there a correlation? Eur J Orthod. 2004; 26:283–288.

5. Song WC, Koh KS, Kim SH, Hu KS, Kim HJ, Park JC, et al. Horizontal angular asymmetry of the face in korean young adults with reference to the eye and mouth. J Oral Maxillofac Surg. 2007; 65:2164–2168.

6. Lee DH, Yu HS. Masseter muscle changes following orthognathic surgery: a long-term three-dimensional computed tomography follow-up. Angle Orthod. 2012; 82:792–798.
7. Isacsson G, Linde C, Isberg A. Subjective symptoms in patients with temporomandibular joint disk displacement versus patients with myogenic craniomandibular disorders. J Prosthet Dent. 1989; 61:70–77.

8. D'Attilio M, Epifania E, Ciuffolo F, Salini V, Filippi MR, Dolci M, et al. Cervical lordosis angle measured on lateral cephalograms; findings in skeletal class II female subjects with and without TMD: a cross sectional study. Cranio. 2004; 22:27–44.
9. Gremillion HA. The prevalence and etiology of temporomandibular disorders and orofacial pain. Tex Dent J. 2000; 117:30–39.
10. Lee WY, Okeson JP, Lindroth J. The relationship between forward head posture and temporomandibular disorders. J Orofac Pain. 1995; 9:161–167.
11. Munhoz WC, Marques AP, Siqueira JT. Radiographic evaluation of cervical spine of subjects with temporomandibular joint internal disorder. Braz Oral Res. 2004; 18:283–289.

12. Bjork A. Some biological aspects of prognathism and occlusion of the teeth. Acta Odontol Scand. 1950; 9:1–40.

13. Marcotte MR. Head posture and dentofacial proportions. Angle Orthod. 1981; 51:208–213.
14. Di Palma E, Gasparini G, Pelo S, Tartaglia GM, Sforza C. Activities of masticatory muscles in patients before orthognathic surgery. J Craniofac Surg. 2010; 21:724–726.

15. Goto TK, Nishida S, Yahagi M, Langenbach GE, Nakamura Y, Tokumori K, et al. Size and orientation of masticatory muscles in patients with mandibular laterognathism. J Dent Res. 2006; 85:552–556.

16. Kiliaridis S, Katsaros C. The effects of myotonic dystrophy and Duchenne muscular dystrophy on the orofacial muscles and dentofacial morphology. Acta Odontol Scand. 1998; 56:369–374.

17. Sims AB, Stack BC, Demerjian GG. Spasmodic torticollis: the dental connection. Cranio. 2012; 30:188–193.

18. Monaco A, Streni O, Marci MC, Sabetti L, Marzo G, Giannoni M. Relationship between mandibular deviation and ocular convergence. J Clin Pediatr Dent. 2004; 28:135–138.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download