Abstract
Purpose
The aim of this study was to describe our treatment experiences with patients who had acute abdomen (AA) with common bile duct (CBD) dilatation.
Methods
The treatment outcomes in children with AA and CBD dilatation were retrospectively reviewed. According to the shape of the intrahepatic bile ducts on ultrasonography (US), the origin of the pain was estimated as choledochal cyst (CC) complication or choledocholithiasis in normal CBD. Patients with complicated CC underwent surgery, and patients with choledocholithiasis in a normal appearing CBD underwent symptomatic treatment initially.
Results
Of the 34 patients, 30 (88.2%) were female. The mean age of the patients was 6.4±4.9 (range, 0.8–17) years. Seventeen (50.0%) patients had CBD stones and 17 (50.0%) did not. Surgical treatment was performed in 20 (58.8%) patients, 2 of whom underwent preoperative stone removal with endoscopic retrograde cholangiopancreatography and an operation. Conservative treatment was applied in 12 (35.3%) patients (8 with and 4 without stones), 1 of whom developed symptom relapse and underwent an operation. Among the 8 patients with CBD stones, 4 (4/17, 23.5%) had complete resolution of the stones and recovery of the CBD diameter after conservative treatment. US findings of patients with stone showed a fusiform or cylindrical shape of the CBD in 14 (82.4%) patients.
Patients who come to the hospital with acute abdominal pain will be subjected to abdominal ultrasonography (US) with a screening test to find the cause of abdominal pain. Biliary dilatation is not uncommonly seen in patients with acute abdomen during abdominal US. When common bile duct (CBD) dilatation was found in the examination, two factors that can cause CBD dilatation can be considered. First, CBD dilatation was present from birth and secondary complications occurred, leading to abdominal pain. Second, passive dilatation was caused by choledocholithiasis in normal CBD and abdominal pain occurred. Because the cause and treatment direction of CBD dilatation are different, it is important to distinguish between these two factors.
It is a priority to accurately determine the presence or absence of CBD dilation by US. The clinical approach therefore requires definition of the normal limits of the bile duct size and imaging examination to define the level and etiology of the obstruction. Reliance on the CBD diameter as a surrogate for choledocholithiasis is associated with a sensitivity ranging from 50% to 90% with a CBD diameter of <6 mm using transabdominal US (TUS) [12]. It is also important to make sure that there is a stone in the distal CBD during abdominal US. Accurate prediction of CBD stones in patient with CBD dilatation avoids the time delay to surgery, operative complications, morbidity, and increased cost associated with additional imaging studies beyond US.
CBD dilatation seems to have no symptomatic pathologic condition at all times. Son et al. [3] reported that incidentally discovered biliary dilatation without any symptoms or abnormalities in laboratory and ultrasound tests in children could be defined as primary ductal dilatation and considered a non-pathologic condition. They suggested that such condition was associated with a relatively benign clinical course and did not require medical intervention. Lee et al. [4] demonstrated that among 162 patients, 131 cases had anomalous biliary tract dilatations and 31 cases had non-anomalous biliary dilatations consisting of normal variants or resulting from secondary causes. Therefore it is necessary to investigate that CBD dilatation is a direct cause of abdominal pain.
Choledochal cysts must be considered when investigating the cause of CBD dilatation and considered as a differential diagnosis of unclear upper abdominal pain, jaundice, and pancreatitis in children. However, 29% to 62% of pediatric patients with choledochal cyst reportedly have choledocholithiasis [56], which may complicate the differentiation between a choledochal cyst and choledocholithiasis alone. Choledocholithiasis can also lead to CBD dilatation, which can be misdiagnosed as a choledochal cyst [7].
In patients with acute abdominal pain accompanied by CBD dilatation, clinicians must differentiate whether the pain is caused by complications of a choledochal cyst or by choledocholithiasis of the normal bile duct. However, there is no guideline or recommendation for management of acute abdominal pain with CBD dilatation, mainly depending on subjective judgment and experience of one's own. There has been little research in this area to provide sound guidelines. Therefore, the aim of this study was to describe our treatment experiences with patients who had abdominal pain with CBD dilatation.
Thirty-four patients aged <18 years who were admitted Pusan National University Children's Hospital due to acute abdomen accompanying dilatation of the CBD on US examination were included in this study. Clinical data such as sex, age, accompanying symptoms, complications, comorbid diseases, treatments, and outcomes were retrospectively collected by reviewing the medical records of the patients from January 2008 to July 2011. This study was approved by the Institutional Review Board of Pusan National University Yangsan Hospital (No. 05-2018-028).
The initial US examination was performed within the first 2 days of presentation of symptoms in all patients. The examinations were conducted by one pediatric gastroenterologist and ultrasound specialist. The CBD diameter was examined by real-time US using a Sequoia 512 US system (Acuson, Mountain View, CA, USA) with a high frequency probe (10-MHz linear transducer) and graded compression. When the diameter of the CBD on sonography exceeded 6 mm, the patient was suspected to have an abnormal CBD.
If the CBD was dilated with or without choledocholithiasis and with abrupt tapering of the intrahepatic bile ducts and/or evidence of acute pancreatitis, we suspected that the abdominal pain had originated from complications of choledochal cyst. If the CBD was dilated with choledocholithiasis and smooth tapering of the intrahepatic bile ducts, the origin of pain was suspected to be CBD obstruction with choledocholithiasis. In patients with choledochal cysts, further investigations such as computed tomography and magnetic resonance cholangiopancreatography were performed to detect combined anomalies in the biliary tree and pancreas.
The patients with complications of choledochal cyst regardless of choledocholithiasis were managed supportively for several days first, and then treated surgically. In contrast, the patients with choledocholithiasis in normal looking CBD were treated symptomatically for several days with a close observation and underwent a follow-up US repeatedly. Depending on the presence or absence of disappearance of stone, we decided to do surgery or to discontinue treatment.
A t-test was used to compare differences in continuous variables between groups. The p-values <0.05 were considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics for Windows ver. 21.0 (IBM Co., Armonk, NY, USA).
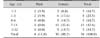
In total, 34 patients were included in this study. Of the 34 patients, 30 (88.2%) were female and 4 (11.8%) were male. The female:male ratio was 7.5:1.0 (p>0.05). The mean age of the patients was 6.4±4.9 (range, 0.8–17) years (Table 1).
Symptoms accompanying abdominal pain were vomiting in 19 (55.9%) patients, fever in 5 (14.7%) and jaundice in 4 (11.8%). Comorbid diseases included acute pancreatitis in 25 (73.5%) patients, CBD stones in 17 (50.0%), cholecystitis in 9 (26.5%), gallbladder stones in 7 (20.6%), anomalous union of the pancreaticobiliary duct (APBDU) in 4 (11.8%), and choledochal cyst rupture in 2 (5.9%) (Table 2).
Half of patients in this study had CBD stones, and half did not. Surgical treatment (choledochojejunostomy) was performed in 20 (58.8%) patients, 2 of whom underwent preoperative stone removal with endoscopic retrograde cholangiopancreatography (ERCP) and an operation. Among the patients with choledocholithiasis, 5 (29.4%) underwent surgical treatment. Conservative treatment was performed in 12 (35.3%) patients (8 with and 4 without stones), 1 of whom developed symptom relapse and underwent an operation. Among the 8 patients with CBD dilatation accompanied by stones, 4 (4/17, 23.5%) had complete resolution of the stones and recovery of the CBD diameter after conservative treatment. The remaining patients had choledochal cysts. Two patients were not followed up (Table 3).
The TUS findings of CBD dilatation with stones (17 patients) showed a fusiform or cylindrical shape of the CBD in 14 (82.4%) patients (p<0.05) (Table 4).
In order to differentiate the cause of CBD dilatation whether it is resulted from choledochal cyst or passive dilatation of normal bile duct by choledocholithiasis, the authors preferentially judged according to the shape of the intrahepatic bile duct in the ultrasound examination. Namely, if the CBD was dilated with abrupt tapering of the intrahepatic bile ducts, we suspected that the abdominal pain had originated from complications of choledochal cyst. If the CBD was dilated with choledocholithiasis and smooth tapering of the intrahepatic bile ducts, the origin of pain was suspected to be CBD obstruction with choledocholithiasis. This judgment seemed to be appropriate for most patients.
The majority of patients with acute abdomen accompanying CBD dilatation were diagnosed with choledochal cysts in the present study, these patients presented with symptoms related to complications of choledochal cysts such as acute pancreatitis, cholecystitis, cyst rupture, and choledocholithiasis. One-third of patients with CBD dilatation and choledocholithiasis underwent surgical treatment in the early days of hospital admission because the presenting symptoms were caused by complicated choledochal cysts. Patients with an indistinguishable cause of CBD dilation, whether the dilation was caused by a secondary change of the normal duct or a congenital anomaly, initially received conservative treatment. Half of these patients had complete resolution of stones and recovery of the CBD diameter after treatment, suggesting that the CBD dilatation was caused by stone impaction in the normal CBD. They could therefore avoid an unnecessary operation. The remaining of patients had choledochal cysts and required surgical treatment.
Oh et al. [6] reported that several cholangiographic features may be helpful for assessing CBD dilatation. Specifically, the severity index of CBD dilatation (calculated by dividing the measured CBD diameter by the age-corrected maximal diameter of a normal CBD) was helpful for discriminating congenital CBD dilatation from obstructive CBD dilatation. Comorbid APBDU was also an important factor for differential diagnosis. However, the presence of choledocholithiasis was not useful for the differential diagnosis of the two CBD types because choledocholithiasis occurred in 76.6% of patients with obstructive CBD dilatation and in 61.8% of patients with congenital CBD dilatation. The use of ERCP has declined because of low detection rates, even in patients considered likely to have CBD stones [8]. Pediatric gastroenterologists have also been reluctant to use ERCP in children because of the risk of complications [9]. Therefore, ERCP should be reserved for patients likely to require therapeutic intervention [10]. In the present study, ultrasound examination was a very useful test to determine the initial treatment policy in patients with acute abdomen accompanying CBD dilatation.
In the present study, most of the CBD dilatations (82.4%) in patients with CBD stones were fusiform or cylindrical in shape. Oh et al. [6] also demonstrated that patients with obstructive CBD dilatation tended to have a CBD with cylindrical-fusiform features more frequently than patients with congenital CBD dilatation (93.3% vs. 78.2%, respectively) and that patients with congenital CBD dilatation tended to have cystic features more frequently than patients with obstructive CBD (21.8% vs. 6.7%, respectively). In a study by Matsumoto et al. [11], 88 (87.1%) of the 101 patients with congenital cystic dilatation of the CBD had adult-type cysts. An adult-type cyst is a fusiform or cylindrical cyst that appears to be closely related to the formation of primary bile duct stones.
Although choledocholithiasis is rare in children, we must consider the possibility of CBD dilatation caused by CBD stones. The underlying pathophysiology of choledocholithiasis in children is unclear and has been commonly related to hemolytic conditions, prematurity, gastrointestinal surgery, Crohn's disease, parenteral nutrition, cystic fibrosis, and diuretic or antibiotic therapy [12]. None of our patients had any of these risk factors.
The approach to management of choledocholithiasis has shifted almost entirely to ERCP-a two-stage approach [13]. Although open CBD exploration is the most effective for clearance of CBD stones, it is associated with higher morbidity and a longer hospital stay than laparoscopic CBD clearance [14]. One-stage laparoscopic CBD stone clearance is currently as effective as both preoperative and postoperative two-stage ERCP CBD clearance with similar morbidity and mortality outcomes [15]. However, there are many reports that CBD stones in children can pass spontaneously without any significant complications [812]. In the present study, 2 patients underwent preoperative stone removal with ERCP and an operation. Among the patients with CBD dilatation accompanied by stones, 24% had complete resolution of the stones and recovery of the CBD diameter after conservative treatment.
In conclusion, when diagnostically approaching patients with acute abdomen accompanying CBD dilatation, complications of choledochal cysts such as acute pancreatitis, cholecystitis and choledochal cyst rupture, must be considered. It is necessary to check the presence of a distal CBD stone, the shape of the CBD and the shape of intrahepatic bile duct on ultrasound, in order to differentiate whether the patient's pain is caused by complications of a choledochal cyst or by choledocholithiasis of the normal bile duct. Surgical treatment should be considered in patients with complicated choledochal cysts. In contrast, symptomatic treatment rather than surgery should be considered in patients with choledocholithiasis in normal appearing CBD.
This study has several limitations associated with its retrospective, single-center design and small patient number. A collaborative and prospective study with a large number of patients is needed to identify the clinical factors differentiating complicated choledochal cysts from choledocholithiasis in patients with a normal CBD.
Figures and Tables
References
1. Liu TH, Consorti ET, Kawashima A, Tamm EP, Kwong KL, Gill BS, et al. Patient evaluation and management with selective use of magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy. Ann Surg. 2001; 234:33–40.

2. Boys JA, Doorly MG, Zehetner J, Dhanireddy KK, Senagore AJ. Can ultrasound common bile duct diameter predict common bile duct stones in the setting of acute cholecystitis? Am J Surg. 2014; 207:432–435.

3. Son YJ, Lee MJ, Koh H, Kim S. Asymptomatic bile duct dilatation in children: is it a disease? Pediatr Gastroenterol Hepatol Nutr. 2015; 18:180–186.

4. Lee HC, Yeung CY, Chang PY, Sheu JC, Wang NL. Dilatation of the biliary tree in children: sonographic diagnosis and its clinical significance. J Ultrasound Med. 2000; 19:177–182.

5. Huang CS, Huang CC, Chen DF. Choledochal cysts: differences between pediatric and adult patients. J Gastrointest Surg. 2010; 14:1105–1110.

6. Oh SH, Chang SH, Kim HJ, Cho JM, Hwang JH, Namgoong JM, et al. Cholangiographic characteristics of common bile duct dilatation in children. World J Gastroenterol. 2015; 21:6229–6235.

7. Youn HS, Seo JH, Park CH, Cho JM, Park JJ. An infantile case of cholelithiasis initially misdiagnosed as choledochal cyst. Pediatr Int. 2012; 54:168–169.

8. Mah D, Wales P, Njere I, Kortan P, Masiakos P, Kim PC. Management of suspected common bile duct stones in children: role of selective intraoperative cholangiogram and endoscopic retrograde cholangiopancreatography. J Pediatr Surg. 2004; 39:808–812.

9. Prasil P, Laberge JM, Barkun A, Flageole H. Endoscopic retrograde cholangiopancreatography in children: a surgeon's perspective. J Pediatr Surg. 2001; 36:733–735.

10. Holm AN, Gerke H. What should be done with a dilated bile duct? Curr Gastroenterol Rep. 2010; 12:150–156.

11. Matsumoto Y, Uchida K, Nakase A, Honjo I. Congenital cystic dilatation of the common bile duct as a cause of primary bile duct stone. Am J Surg. 1977; 134:346–352.

12. Nordin N, Alex G, Clarnette T, Stephens N, Oliver M. Common bile duct stones in infancy: a medical approach. J Paediatr Child Health. 2012; 48:705–709.

13. Abboud PA, Malet PF, Berlin JA, Staroscik R, Cabana MD, Clarke JR, et al. Predictors of common bile duct stones prior to cholecystectomy: a meta-analysis. Gastrointest Endosc. 1996; 44:450–455.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download