Abstract
Purpose
Treatment of chronic constipation and fecal impaction is usually outpatient and requires high or frequent doses of laxatives. However, there are children who fail outpatient treatments, sometimes repeatedly, and are ultimately hospitalized. We sought to compare the characteristics of the children who failed outpatient treatment and needed inpatient treatment vs those who achieved success with outpatient treatment, in an effort to identify attributes that might be associated with a higher likelihood towards hospitalization.
Methods
In this retrospective cohort study, we reviewed the medical records of all patients aged 0 to 21 years, with chronic functional constipation and fecal impaction seen in the pediatric gastroenterology clinic over a period of 2 years.
Results
Total of 188 patients met inclusion criteria. While 69.2% were successfully treated outpatient (referred to as the outpatient group), 30.9% failed outpatient treatment and were hospitalized (referred to as the inpatient group). The characteristics of the inpatient group including age at onset of 3.6±3.6 years (p=0.02); black ethnicity (odds ratio [OR] 4.31, 95% confidence interval [95% CI] 2.04–9.09); p<0.001); prematurity (OR 2.39, 95% CI 1.09–5.26; p=0.02]; developmental delay (OR 2.20, 95% CI 1.12–4.33; p=0.02); overflow incontinence (OR 2.26, 95% CI 1.12–4.53, p=0.02); picky eating habits (OR 2.02, 95% CI 1.00–4.08; p=0.04); number of ROME III criteria met: median 4, interquartile range 3–5 (p=0.04) and 13±13.7 constipation related prior encounters (p=0.001), were significantly different from the outpatient group.
Functional constipation is a common pediatric health problem with a prevalence between 1% and 30% [12]. In a birth cohort study, medical visits for constipation was noted to be the highest among all functional gastrointestinal diseases [3]. Severe constipation can lead to a state of fecal impaction as defined by various professional societies [45]. The North American and European Societies for Pediatric Gastroenterology, Hepatology and Nutrition describe it as a dilated rectum filled with a large amount of stool; a hard mass palpated in the lower abdomen on physical examination; or excessive fecal loading in the distal colon on abdominal radiography. Treatment involves high or frequent doses of laxatives, usually in an outpatient setting. However, some children fail outpatient treatment and are hospitalized [6]. Inpatient treatment usually involves invasive procedures like insertion of a nasogastric tube, intravenous fluids, rectal enema, etc. which are painful for a child. Further, inpatient management of constipation is expensive and, thus, undesirable for patient's family, insurers, and the health system at large [7]. Characteristics of children who fail outpatient treatment and are hospitalized have not been described; there is definite need for such knowledge. We believe that awareness of such characteristics will be helpful for the informed physician to anticipate challenging treatment scenarios, and enable timely institution of the most appropriate intervention(s) as an outpatient to potentially avoid hospitalization. Thus, we sought to study the characteristics of our group of children who failed initial outpatient treatment and were hospitalized for bowel clean outs (the inpatient group). We compared them with those children who were successfully treated as outpatients (the outpatient group).
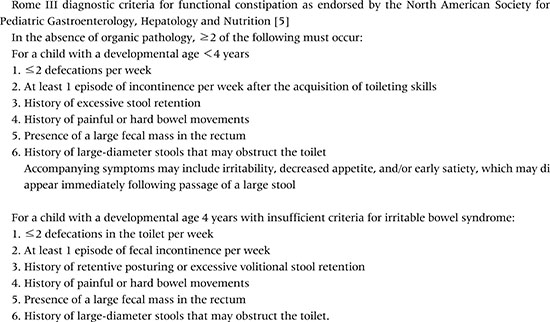
We conducted a retrospective chart review of children and adolescents (0 to 21 years of age) who were treated for chronic constipation and fecal impaction in our Pediatric Gastroenterology Clinic at MetroHealth Medical Center, an academic medical center affiliated with Case Western Reserve University, over a period of 2 consecutive years. We excluded children with constipation due to an organic pathology. Our first line treatment for fecal impaction is outpatient-based laxative therapy. Some of these children who failed outpatient treatment were then hospitalized for inpatient treatment. Thus, we had two groups of children: those who were treated successfully in the outpatient setting, the outpatient group; and the second group who failed outpatient management and required inpatient treatment, the inpatient group (Fig. 1). We collected the following information for both groups: patient demographics; past medical history; symptoms of constipation based on Rome III; other associated symptoms; and number of constipation-related visits in other healthcare settings prior to the pediatric gastroenterology visit, e.g., ambulatory pediatric visits, urgent care and emergency department visits, nurse helpline phone encounters. The institutional review board at MetroHealth Medical Center approved our study (No. 15-00667).
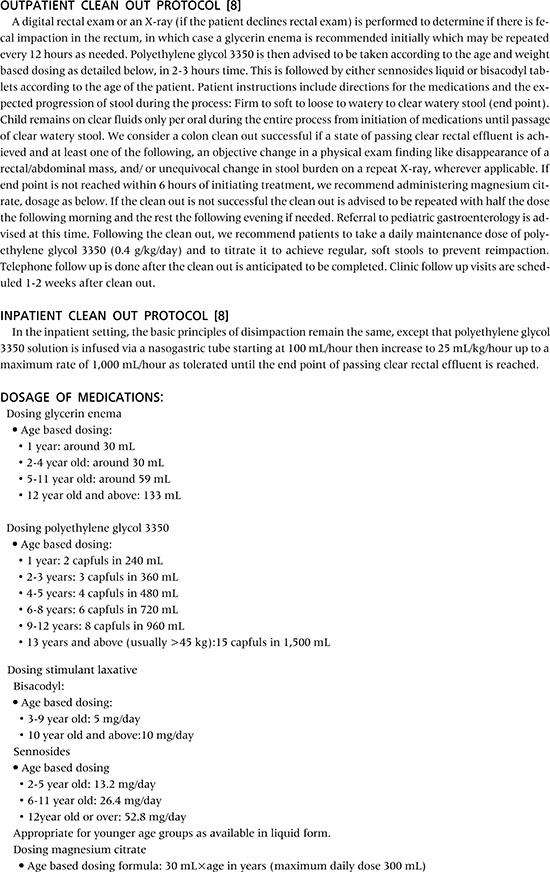
We follow a standard outpatient regimen for disimpaction in our pediatric gastroenterology clinic. Our goal for the patient is to achieve a state of complete colon clean out. The patient drinks a solution of polyethylene glycol 3350 mixed with a clear beverage (e.g., juice, water, etc.) followed by a stimulant laxative like senna or bisacodyl. Additional laxatives like magnesium citrate and enemas are prescribed on an as needed basis. Laxative doses have been extrapolated from a clinical report by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition Endoscopy and Procedures Committee (Appendix 1) [8]. Similar regimens have been shown to be effective in achieving colon clean out in an outpatient setting, thereby, avoiding hospital admissions [9]. For inpatient treatment, we use a polyethylene glycol 3350 and electrolytes solution via nasogastric tube and stimulant laxatives (senna or bisacodyl). If a large/ hard fecal mass is present on digital rectal exam we give an enema to dislodge the rectal mass first. After the colon clean out, the patient is started on daily maintenance treatment with polyethylene glycol 3350 to achieve regular, soft bowel movements.
We expressed the data as means±standard deviations, and as medians with interquartile ranges. Also, we expressed it as percentages and odds ratios with 95% confidence intervals. We analyzed continuous data using t-tests or Mann-Whitney U-tests, as appropriate. We analyzed dichotomous data using chi-square or Fisher exact tests, as appropriate.
Total of 188 patients met our inclusion criteria. The mean age at presentation to the gastroenterology clinic was 8.8±4.2 years, and 52.7% (99/188) were female. All of them received initial outpatient treatment. We noted that 69.2% were treated successfully as outpatients (the outpatient group) and 30.9% (58/188) failed the outpatient treatment and were hospitalized for treatment (the inpatient group).
We found that there was a significantly larger proportion of children of black ethnicity in the inpatient treatment group as compared to the outpatient group. On the other hand, a significantly larger percentage of Hispanic children were successfully treated as outpatients. The proportion of other demographic features like gender, insurance type, and body mass index were not different between the two groups (Table 1).
Our inpatient group was significantly younger at the time of onset of constipation than the outpatient treatment group, with a median age of 3.6 years in the inpatient group versus 5 years in the outpatient group. The number of prior constipation-related visits (before the pediatric gastroenterology visit) were higher in the inpatient group with a mean of 13 visits in the inpatient group versus 6.6 visits in the outpatient group (Table 2).
We found a higher percentage of children with developmental delay and history of prematurity in the inpatient group as compared to the outpatient group. The percentage of children with mental health disorders, behavioral disorders, autism spectrum disorder, cerebral palsy, neuromuscular disorder, spina bifida, thyroid disorder, Hirschsprung disease, and other intestinal anatomical disorders were not significantly different between the two groups (Table 3).
Children in the inpatient group were noted to have a greater number of signs and symptoms corresponding to ROME III criteria. Overflow incontinence and ‘picky eating habits’ were also more common in the inpatient group. The two groups did not differ much in terms of other associated signs and symptoms such as chronic abdominal pain, rectal pain, rectal prolapse, hematochezia, straining, nausea and vomiting (Table 4).
Our study results provide novel insights in to the clinical characteristics of children who failed outpatient treatment and needed hospitalization for severe constipation at our institution.
The presence of a significantly greater number of children of black ethnicity in the inpatient group is noteworthy. Interesting ethnic trends and attitudes towards bowel habits have been reported in this group. In a community-based study of children of primarily African-American ethnicity who presented to pediatric clinics for routine health maintenance visits, it was noted that 19.3% of children had a functional gastrointestinal disorder based on responses to the Questionnaire on Pediatric Gastrointestinal Diseases, that were confirmed by a pediatric gastroenterologist. Functional constipation was identified as the most common functional gastrointestinal disorder. While 16% of the children in this study met symptom-based criteria for functional constipation, the majority had not complained to their pediatrician about it. The author stated that this finding suggests that constipation is underreported or not perceived as a significant problem in this ethnic group [10]. This trend could worsen constipation and explain higher rates of failure of outpatient treatment. On the other hand, Hispanic children were represented in a larger proportion in the outpatient group, this observation needs further investigation.
Our study found that young age at onset of constipation of around 3.6 years was noted in the inpatient group. Since the mean age of presentation to the pediatric gastrointestinal clinic was 8.8±4.2 years, it is possible that a delay in diagnosis or lack of effective treatment may have led to recurrent impactions or a state of chronic fecal impaction in these children. This could also explain the findings of Bongers et al. [11], who found that 25% of patients who developed constipation before the age of 5 years continued to have severe complaints of constipation, infrequent painful defecation, and fecal incontinence beyond puberty. The number of constipation-related visits (prior to visit to the pediatric gastroenterologist) was significantly greater in the inpatient group. Poor response to outpatient therapy, persistent symptoms, and parental frustration may have led to the increased utilization of ambulatory healthcare services.
There were a significantly greater number of children with history of prematurity in the inpatient group. Although, a longitudinal follow-up study of extremely low birth weight babies suggested that a lower gestational age was associated with chronic constipation in childhood [12], there is a paucity of further studies studying causality. Also, our study found a larger number of children with history of developmental delay (motor, speech, not otherwise specified type, etc.) in the inpatient group as compared to the outpatient group. The need for inpatient treatment in this population could be attributed to delay in recognition and treatment of constipation because of communication difficulties, and other overriding health priorities, particularly in children with disabilities. Compliance with treatment may also be challenging for children with developmental delays especially autistic children with their ritualistic behaviors, sensitivities, and behavioral issues [13]. Developmental delay might also predispose them to feeding difficulties, nutritional deficiencies, toileting problems, etc. [14]. Even though the majority of our study children with developmental delay were not frankly disabled, it is reasonable to speculate that some of the above factors may have contributed to our findings.
Children in the inpatient group displayed a greater no. of symptoms based on ROME III (Appendix 2) with a median of 4 criteria (3–5) as compared to 3 criteria (2–4) in the outpatient group. Also, a significantly larger percentage of children in the inpatient group presented with overflow incontinence which could be considered an indicator of the chronicity of disease. This is supported by a study that has reported the persistence of overflow incontinence despite good comprehension and acceptance of treatment modalities such as enemas, toileting schedules, etc. Complete recovery rates, even with good adherence, have been noted to be only 35.7% after 3.5 years [15]. Management of overflow incontinence with its strong behavioral and psychosocial facets is particularly challenging [16]. Another reason could be the large volume of laxative solution needed to achieve intestinal clearance in these patients which may make it difficult for the child to drink as an outpatient. Ingebo and Heyman [6] reported that children with overflow incontinence needed an average of 11.8 L (574 mL/kg) of polyethylene glycol solution given over 22.5 hours, while the other children needed only 4.0 L (128 mL/kg) given over 7.5 hours to clear their intestines as inpatients.
Picky eating habits were noted to be a more common characteristic among the children in the inpatient group. It has been established that eating problems can be both the cause and effect of chronic functional constipation. An association between picky eating habits and hard stools has been noted, possibly mediated by low fiber intake, particularly from vegetables [1718]. This association might trigger a vicious cycle with picky eating habits leading to hard stools and constipation, impairing appetite and further fueling the picky eating habits, gradually worsening the course of the disease. This along with the non-compliance with the outpatient regimen resulting from unwillingness to drink the requisite amounts of oral laxatives might contribute to the need for an inpatient admission.
We acknowledge some limitations of our study. It is a retrospective study from a single center. The information was extracted from medical records and relies on previous documentation. Our results reveal the presence of certain characteristics in each treatment group; they do not establish causality or the risk of needing inpatient treatment. Future prospective studies designed to study this are needed. Our patient population comprised of children referred to a specialist; these children who presumably are on the severe end of the disease spectrum may be prone to referral bias. Lastly, we feel that our sample size could have been larger. For example, contrary to the author's experience and some of the published literature, associated conditions like autistic spectrum disorder, cerebral palsy, and behavioral disorders did not reach significance. We speculate that with a larger sample size, perhaps, some of these factors may have emerged as significant for inpatient treatment.
We would like to highlight the strengths of our study. To the best of our knowledge, our study is the first to study and compare the characteristics of the patients who eventually needed inpatient treatment versus outpatient for severe chronic constipation and fecal impaction. Secondly, a single subspecialty provider treated all patients using uniform and evidence-based regimens, thereby eliminating heterogeneity and minimizing treatment bias. Lastly, our patient population is representative of most urban, inner city hospital systems. Thus, our results may prove very useful to a large number of pediatric hospital systems.
In conclusion, we have described characteristics of children that were eventually hospitalized for inpatient treatment of fecal impaction. Conversely, we may have suggested patient characteristics that portend a potentially higher probability of failure of outpatient treatment. We think these results are important and may prove helpful to providers in anticipating challenging treatment scenarios and in individualizing outpatient treatment decisions for their patients. Some of these include discussing patient's/family's barriers to completing the recommended outpatient treatment; to address the barriers to the greatest extent possible; to recommend a more aggressive treatment regimen if needed; to institute a more stringent follow-up plan like closely scheduled clinic visits, telephone calls and possibly home visits; and the ultimate goal of achieving successful outpatient clean-out. This would be a substantial achievement considering the rising inpatient burden of childhood constipation and the tremendous impact on cost of healthcare [719]. However, if some patients still require inpatient treatment, clinicians should intervene expeditiously to optimize the patient's experience, parental satisfaction, and to reduce unnecessary visits to other costlier health care settings, particularly emergency room visits to relieve fecal impaction.
Figures and Tables
Table 2
Comparison of Age at Onset of Constipation, Duration of Disease, and Health Care Utilization between the Outpatient and Inpatient Groups
ACKNOWLEDGEMENTS
Robert Needlman, MD, Professor of Pediatrics, Developmental and Behavioral Pediatrics, MetroHealth Medical Center affiliated with Case Western Reserve University, critically reviewed the study proposal and served as scientific advisor. Niraj Vora, MD, Resident, MetroHealth Medical Center affiliated with Case Western Reserve University, worked on initial planning of the study and contributed to data collection. Catherine Haskins, Ph.D., affiliated with Birchwood School of Hawken, Cleveland, participated in literary proofreading and editing the final draft of the manuscript.
References
1. van den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006; 101:2401–2409.

2. Wald ER, Di Lorenzo C, Cipriani L, Colborn DK, Burgers R, Wald A. Bowel habits and toilet training in a diverse population of children. J Pediatr Gastroenterol Nutr. 2009; 48:294–298.

3. Chitkara DK, Talley NJ, Weaver AL, Katusic SK, De Schepper H, Rucker MJ, et al. Incidence of presentation of common functional gastrointestinal disorders in children from birth to 5 years: a cohort study. Clin Gastroenterol Hepatol. 2007; 5:186–191.

4. Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014; 58:258–274.

5. Benninga M, Candy DC, Catto-Smith AG, Clayden G, Loening-Baucke V, Di Lorenzo C, et al. The Paris Consensus on Childhood Constipation Terminology (PACCT) Group. J Pediatr Gastroenterol Nutr. 2005; 40:273–275.

6. Ingebo KB, Heyman MB. Polyethylene glycol-electrolyte solution for intestinal clearance in children with refractory encopresis. A safe and effective therapeutic program. Am J Dis Child. 1988; 142:340–342.

7. Sethi S, Mikami S, Leclair J, Park R, Jones M, Wadhwa V, et al. Inpatient burden of constipation in the United States: an analysis of national trends in the United States from 1997 to 2010. Am J Gastroenterol. 2014; 109:250–256.

8. Pall H, Zacur GM, Kramer RE, Lirio RA, Manfredi M, Shah M, et al. Bowel preparation for pediatric colonoscopy: report of the NASPGHAN endoscopy and procedures committee. J Pediatr Gastroenterol Nutr. 2014; 59:409–416.
9. Jordan-Ely J, Hutson JM, Southwell BR. Disimpaction of children with severe constipation in 3–4 days in a suburban clinic using polyethylene glycol with electrolytes and sodium picosulphate. J Paediatr Child Health. 2015; 51:1195–1198.

10. Uc A, Hyman PE, Walker LS. Functional gastrointestinal disorders in African American children in primary care. J Pediatr Gastroenterol Nutr. 2006; 42:270–274.

11. Bongers ME, van Wijk MP, Reitsma JB, Benninga MA. Long-term prognosis for childhood constipation: clinical outcomes in adulthood. Pediatrics. 2010; 126:e156–e162.

12. Cunningham C, Taylor HG, Klein N, Minich NM, Hack M. Constipation is a problem among former <750 gram birthweight (ELBW) children. Pediatr Res. 1998; 43:100.

13. Elawad MA, Sullivan PB. Management of constipation in children with disabilities. Dev Med Child Neurol. 2001; 43:829–832.

14. Malone C, Sharif F, Glennon-Slattery C. Growth and nutritional risk in children with developmental delay. Ir J Med Sci. 2016; 185:839–846.

15. Bernard-Bonnin AC, Haley N, Bélanger S, Nadeau D. Parental and patient perceptions about encopresis and its treatment. J Dev Behav Pediatr. 1993; 14:397–400.

16. Ranasinghe N, Devanarayana NM, Benninga MA, van Dijk M, Rajindrajith S. Psychological maladjustment and quality of life in adolescents with constipation. Arch Dis Child. 2017; 102:268–273.

17. Taylor CM, Northstone K, Wernimont SM, Emmett PM. Picky eating in preschool children: Associations with dietary fibre intakes and stool hardness. Appetite. 2016; 100:263–271.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download