Abstract
Purpose
We investigated fecal calprotectin (FC) levels in preterm infants with and without feeding intolerance (FI), and compared the FC levels according to the type of feeding.
Methods
The medical records of 67 premature infants were reviewed retrospectively. The fully enteral-fed infants were classified into two groups; the FI group (29 infants) and the control group (31 infants). Seven infants with necrotizing enterocolitis, sepsis, and perinatal asphyxia were excluded. If breast milk (BM) or preterm formula (PF) could not be tolerated by infants with FI, amino acid-based formula (AAF) was tried temporarily. Once FI improved, AAF was discontinued, and BM or PF was resumed. We investigated the FC levels according to the type of feeding.
Results
Significant differences were found in gestational age, birth weight, age when full enteral feeding was achieved, and hospital stay between the FI and control group (p<0.05). The FC levels in the FI group were significantly higher than those in the control group (p<0.05). The FC levels in the AAF-fed infants with FI were significantly lower than those in the BM- or PF-fed infants (p<0.05). The growth velocities (g/d) and z scores were not significantly different between the FI and control group (p>0.05).
Enteral feeding advancement in preterm infants is one of the most challenging tasks in postnatal growth [1]. Delayed enteral feeding might be associated with decreased gastrointestinal (GI) hormone secretion and intestinal motility [2]. Owing to delayed enteral nutrition, prolonged use of an indwelling catheter for parenteral nutrition is associated with postnatal infection with an increased risk of mortality, prolonged hospitalization, and adverse neurodevelopmental outcome in preterm infants [34]. However, many clinical situations withhold feeding of preterm infants because of the fear of various detrimental GI complications [5]. Feeding intolerance (FI), defined as the inability to digest enteral feeding associated with increased gastric residuals, abdominal distension, and/or emesis, frequently develops in preterm infants [1]. The known risk factors for FI are a weak esophageal sphincter, delayed gastric emptying time, intestinal hypomotility, and abnormal bacterial colonization [67]. The immaturity of the GI tract plays a predominant role in preterm infants with FI [8]. Functional and biochemical maturation are established gradually over the last trimester of gestation and are influenced by different interacting factors such as age, drug use, diet, and intestinal microflora [9]. This greatly affects the digestive absorptive function of preterm infants. Protein digestion begins with hydrolysis in the acid environment of the stomach and is processed with multiple proteases [10]. However, limited gastric acid secretion in preterm infants results in decreased activity of enterokinases to hydrolyze proteins and activate pancreatic protease digestive cascade [11]. The aforementioned facts suggest that absorption of hydrolyzed protein could be easier in preterm infants. Mihatsch et al. [12] reported that the use of hydrolyzed protein formulas in preterm infants established full enteral feeding more rapidly. Raimondi et al. [13] reported that a short course of amino acid-based formula (AAF) was a safe and effective rescue strategy for very-low-birth-weight (VLBW) infants with FI.
Calprotectin is an antimicrobial protein found in neutrophils, monocytes, macrophages, and some squamous epithelium cells and known to increase especially in GI inflammation [1415]. Its presence in stool indicates neutrophil migration to the GI mucosa and can suggest the severity of mucosal inflammation [1416]. According to a recent systemic review, fecal calprotectin (FC) level was elevated in infants with necrotizing enterocolitis (NEC) and was useful as a noninvasive prognostic marker of NEC [17]. However, high FC levels in healthy infants are related to the physiological response of the gut, such as intestinal permeability, gut microbiota, and response to alimentary allergens [18].
We investigated FC levels in preterm infants with and without FI, and compared the FC levels after changing to AAF.
We retrospectively reviewed the medical records of 67 premature infants born at 29–32 weeks' gestation who were admitted to the neonatal intensive care unit of Keimyung University Dongsan Medical Center between May and September 2016. This study was approved by the Institutional Review Board of Keimyung University Dongsan Medical Center (No. 2017-01-037). Seven infants with perinatal asphyxia (Apgar score at 5 minutes, ≤5), sepsis, and NEC were excluded. FI was defined as the inability to digest enteral feeding, which presents as a gastric residual volume of >50%, abdominal distension, emesis, or disruption of the patient's feeding plan [7]. Full enteral feeding was defined as enteral tolerance of at least 120 mL/(kg·d) of milk [7].
All enrolled infants were fed within 3 hours of life using either with mother's breast milk (BM) or with preterm formula (PF) when BM was not available due to mother's condition. The infants with FI were temporarily fed with AAF (Neocate®; Nutricia, London, UK) instead of BM or PF. Calprotectin was investigated as fecal specimens collected from a fresh diaper which was changed every three hours. Infants without FI were examined for calprotectin in the feces once on the 7th day of life. In infants with FI, fecal specimens were taken before feeding was changed to AAF. Subsequent FC levels were measured at least 3 days after feeding with AAF. Once the babies with FI showed clinical improvement, AAF feeding was discontinued, and the previous diet, either BM or PF, was resumed. FC levels were measured using a commercial quantitative enzyme-linked immunosorbent assay kit on the Alegria system (ORGENTEC Diagnostika, Mainz, Germany). The measurable range of FC was from 0 to 1,000 µg/g.
The following variables were analyzed for the perinatal factors: gestational age (GA), birth weight (BW), sex, delivery mode (vaginal delivery or cesarean section), multiple gestation, small for GA (SGA), oligohydramnios, pregnancy-induced hypertension (PIH), antenatal steroid, premature rupture of membrane, gestational diabetes mellitus (GDM), and Apgar score at 1 and 5 minutes.
The growth velocity and z scores were checked at the time of discharge. The growth velocity was calculated using the following formula: (body weight at discharge [g]−BW [g])/hospital stay[d], g/d). The z score was calculated using the Lambda Mu Sigma method [19]. L determines a nonlinear transformation of BW, M stands for the mean of normal distribution, and S stands for its standard deviation (SD). L, M, and S correspond to the following formulas: Z=[(X/M)L−1]/LS, where X indicates the measured value of BW, and centile=M (1+LSZ)1/L, where Z is the z score that corresponds to a given percentile. The z score is a measure of the distance in SDs of a sample from the mean [19].
Statistical analysis was conducted using SPSS Statistics ver. 17.0 (SPSS Inc., Chicago, IL, USA). Descriptive results were reported as the mean±SD. Statistical analysis between groups were conducted with the Student t-test for independent samples for normally distributed data and with the Mann-Whitney U-test for non-normally distributed data. The chi-square test was performed for categorical variables, and the Pearson correlation test was used to evaluate the relationship between the selected variable and FC values. For the interpretation of results, p-values of <0.05 were considered significant.
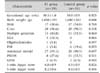
The study population included 60 preterm infants (34 males and 26 females), of whom 29 (48.3%) were grouped as the FI group. The mean age at FI onset was 3.7±1.0 days. AAF was fed for a mean duration of 14.2±8.3 days in the FI group. Table 1 shows the comparison between FI and control group. There was a significant difference in the mean GA (30.3± 1.0 weeks vs. 30.8±0.9 weeks, p<0.05) and BW (1,458± 291 g and 1,600±243 g, p<0.05). However, no significant differences were shown in sex, delivery mode, multiple gestation, SGA, oligohydramnios, PIH, antenatal steroid use, GDM, and Apgar score at 1 and 5 minutes between the two groups (p>0.05).
The FC levels in the FI group were significantly higher than in the control group (855±240 µg/g vs. 401±270 µg/g, p<0.05). As shown in Fig. 1, the FC levels in BM- or PF-fed infants with FI were significantly higher than in AAF-fed infants with FI (898±174 µg/g vs. 273±204 µg/g, p<0.05). At the time of the first FC investigation, there were 3 BM-fed infants (10.3%) and 26 PF-fed infants (89.7%) in the FI group.
Fig. 2 showed the postnatal age-related FC levels in the infants with FI by the type of feeding. There was a negative correlation between FC levels and postnatal age in BM- or PF-fed infants and AAF-fed infants, but not statistically significant (p>0.05).
Postnatal outcomes were assessed with time to full enteral feeding (d), hospital stay (d), body weight at discharge (g), growth velocity (g/d), and z score. We compared the variables between the FI and control groups (Table 2). Time to full enteral feeding (d) was significantly longer in the FI group than in the control group (4.0±0.9 days vs. 3.2±0.8 days, respectively, p<0.05). In addition, hospitalization duration was significantly longer in the FI group than in the control group (34.2±13.2 days vs. 26.4±11.2 days, p<0.05). There was no statistically significant difference between the two groups regarding body weight at discharge, growth velocity, and z scores (p>0.05).
In our preliminary study, the FC levels in FI group were significantly higher than in non-FI group. And the FC levels in AAF-fed infants with FI were significantly lower than BM- or PF-fed infants with FI. No significant differences in postnatal growth parameters were observed between the FI and control groups, which might be associated with the temporary use of AAF.
Previous reports of FC levels in preterm infants indicated a wide range of GA in enrolled infants [1220]. FC levels depend on the gestational and postnatal ages of preterm infants [21]. In the present study, we selectively investigated FC levels in preterm infants born at 29–32 weeks' gestation. A research in preterm infants born at <32 weeks' gestation reported a wide range of FC levels and that FC levels correlated positively with the volume of enteral feeding and the need to interrupt enteral feeding [22]. It is in line with the result of our study that the FI infants showed higher FC levels comparing to the non-FI infants.
The increase in FC level suggests a high level of granulocytes in the gut lumen, which is a hallmark of digestive inflammatory status [20]. Few studies investigated FC levels in preterm infants with FI, and the reference level was investigated a little in term and preterm infants. The studies found higher FC levels in newborns and younger infantsthan in children and adults, which could suggest greater intestinal permeability and different immunological status of the gut in newborns. Mussa et al. [16] studied FC levels in preterm infants with and those without FI, and suggested a cutoff value for FI screening. The result of the study showed that the significantly higher level of FC in the FI group even with various types of feeding, which is in line with the result of our study. Some studies researched about the relationship between the types of feeding and FC levels. Li et al. [20] reported higher FC levels in healthy, exclusively BM-fed infants than in non-BM-fed ones in the first 5 months of life. Savino et al. [23] also reported a similar result of high FC levels in healthy, exclusively BM-fed infants. However, Rougé et al. [22] observed that FC levels were lower in infants with human milk than in infants exclusively or predominantly fed with formula. Campeotto et al. [24] and Yang et al. [25] reported no significant difference in FC levels between the infants fed with BM and those fed with hydrolyzed formula. In the present study, three infants of FI group were fed with BM and twenty-six infants were fed with PM. Due to those differences, there would be a limit to compare the FC levels between the infants fed with BM and those fed with PF. Further prospective studies will be needed to investigate the levels of FC in preterm infants according to the more specific type of feeding. However, no study has been conducted yet about the investigation of FC levels according to the change of feeding regimen in preterm infants with FI, which was shown in the present data. Raimondi et al. [13] compared the infants fed with AAF with the controls fed with PF in terms of time to full enteral feeding, time on parenteral nutrition, time on central venous line, gastric residual volume, and the outcomes on growth at discharge and at 12 months of life. The result and conclusion of the study were that AAF was a safe nutritional alternative for rescuing VLBW infants with intrauterine growth restriction with severe FI. The mean duration of AAF feeding was 15.4±12.3 days in their study and 14.2±8.3 days in our study. The growth outcome in their study was not impaired in the AAF group, which is in line with the result of our study, even though we did not examine long-term results on growth yet.
So far, little is known about the gut response to enteral nutrition during the postnatal period in preterm infants [26]. The immature digestive, absorptive, and immunologic functions in preterm infants can lead to nutrient fermentation, bacterial overgrowth, and mucosal inflammation, which altogether can lead to the intolerance of feeding [26]. In the present study, the lowered level of FC concentration after AAF feeding in infants with FI could suggest that the alleviation of the gut inflammation. AAF is composed of lowered lactose, higher percentage of medium chain triglycerides, and completely hydrolyzed protein with amino acids [27]. The amino acids are essential for the intestinal function with an important role for mucosal blood perfusion, growth, and immunity [28]. The deficiency of the amino acids should result in the impairment of the intestinal function, which can be led to the bacterial overgrowth and mucosal inflammation. According to the previous animal studies, it is known that during the final weeks of gestation, there is a rapid increase in the tissue-specific capacity for glucose uptake, whereas the ability of the mucosa to absorb most amino acids remains low [2629]. And other researches also revealed that the ability to take up and transfer intact proteins from the epithelium into the circulation is a highly specialized function that develops very close to term, which means that the digestive function for protein macromolecules is far more impaired in preterm infants [30]. Those results in premature intestine could advocate the use of partially or totally hydrolyzed milk diets in a situation of delay in introducing or advancement of enteral nutrition in preterm infants.
A question can arise about nutritional adequacy in long-term use of AAF and hydrolyzed protein formula. Rigo et al. [31] and Szajewska et al. [32] reported about the nutritional insufficiency of hydrolyzed protein formula for term and preterm infants. Zuppa et al. [33] also had the same question in their study. In the present study, the patients with FI who switched to AAF for a short termdid not develop any adverse clinical sign or symptom during AAF feeding, and it showed improvement in the symptoms and signs of FI with proper body weight gain. Once the clinical presentation of FI improved, AAF feeding was switched to BM or PF. The growth velocity and z score did not show significant differences when compared with those in the control group at the time of discharge.
In summary, in our preliminary study with a small cohort of preterm infants with FI, the FC levels of the BM- or PF-fed infants were significantly higher than those of the AAF-fed infants. No significant differences in postnatal growth parameters were found between the FI and control groups. As an elemental diet is used for cow's milk protein intolerance or inflammatory bowel disease, we can hypothesize that FI, an inflammatory status of immature GI tract, can be alleviated by temporary use of elemental diet if BM or other formulas are not suitable. The mitigation of gut inflammation through the decrease of FC levels in AAF-fed infants with FI could be presumed.
Figures and Tables
 | Fig. 1Fecal calprotectin levels by type of feeding in preterm infants with feeding intolerance. BM: breast milk, PF: preterm formula, AAF: acid-based formula. |
 | Fig. 2The postnatal age-related fecal calprotectin levels in preterm infants with feeding intolerance by type of feeding. BM: breast milk, PF: preterm formula, AAF: acid-based formula. |
References
1. Moore TA, Wilson ME. Feeding intolerance: a concept analysis. Adv Neonatal Care. 2011; 11:149–154.
2. Berseth CL, Nordyke CK, Valdes MG, Furlow BL, Go VL. Responses of gastrointestinal peptides and motor activity to milk and water feedings in preterm and term infants. Pediatr Res. 1992; 31:587–590.

3. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002; 110:285–291.

4. Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004; 292:2357–2365.

5. Hay WW Jr. Aggressive nutrition of the preterm infant. Curr Pediatr Rep. 2013; 1:DOI: 10.1007/s40124-013-0026-.

6. Mansi Y, Abdelaziz N, Ezzeldin Z, Ibrahim R. Randomized controlled trial of a high dose of oral erythromycin for the treatment of feeding intolerance in preterm infants. Neonatology. 2011; 100:290–294.

7. Indrio F, Riezzo G, Cavallo L, Di Mauro A, Francavilla R. Physiological basis of food intolerance in VLBW. J Matern Fetal Neonatal Med. 2011; 24:Suppl 1. 64–66.

8. Lebenthal E, Lee PC, Heitlinger LA. Impact of development of the gastrointestinal tract on infant feeding. J Pediatr. 1983; 102:1–9.

10. Hyman PE, Clarke DD, Everett SL, Sonne B, Stewart D, Harada T, et al. Gastric acid secretory function in preterm infants. J Pediatr. 1985; 106:467–471.

11. Hyman PE, Feldman EJ, Ament ME, Byrne WJ, Euler AR. Effect of enteral feeding on the maintenance of gastric acid secretory function. Gastroenterology. 1983; 84:341–345.

12. Mihatsch WA, Franz AR, Högel J, Pohlandt F. Hydrolyzed protein accelerates feeding advancement in very low birth weight infants. Pediatrics. 2002; 110:1199–1203.

13. Raimondi F, Spera AM, Sellitto M, Landolfo F, Capasso L. Amino acid-based formula as a rescue strategy in feeding very-low-birth-weight infants with intrauterine growth restriction. J Pediatr Gastroenterol Nutr. 2012; 54:608–612.

14. Fagerhol MK, Dale I, Andersson T. A radioimmunoassay for a granulocyte protein as a marker in studies on the turnover of such cells. Bull Eur Physiopathol Respir. 1980; 16:Suppl. 273–282.

15. Lamb CA, Mansfield JC. Measurement of faecal calprotectin and lactoferrin in inflammatory bowel disease. Frontline Gastroenterol. 2011; 2:13–18.

16. Moussa R, Khashana A, Kamel N, Elsharqawy SE. Fecal calprotectin levels in preterm infants with and without feeding intolerance. J Pediatr (Rio J). 2016; 92:486–492.

17. Pergialiotis V, Konstantopoulos P, Karampetsou N, Koutaki D, Gkioka E, Perrea DN, et al. Calprotectin levels in necrotizing enterocolitis: a systematic review of the literature. Inflamm Res. 2016; 65:847–852.

18. Kapel N, Campeotto F, Kalach N, Baldassare M, Butel MJ, Dupont C. Faecal calprotectin in term and preterm neonates. J Pediatr Gastroenterol Nutr. 2010; 51:542–547.

19. Lim JS, Lim SW, Ahn JH, Song BS, Shim KS, Hwang IT. New Korean reference for birth weight by gestational age and sex: data from the Korean Statistical Information Service (2008–2012). Ann Pediatr Endocrinol Metab. 2014; 19:146–153.

20. Li F, Ma J, Geng S, Wang J, Ren F, Sheng X. Comparison of the different kinds of feeding on the level of fecal calprotectin. Early Hum Dev. 2014; 90:471–475.

21. Zoppelli L, Güttel C, Bittrich HJ, Andrée C, Wirth S, Jenke A. Fecal calprotectin concentrations in premature infants have a lower limit and show postnatal and gestational age dependence. Neonatology. 2012; 102:68–74.

22. Rougé C, Butel MJ, Piloquet H, Ferraris L, Legrand A, Vodovar M, et al. Fecal calprotectin excretion in preterm infants during the neonatal period. PLoS One. 2010; 5:e11083.

23. Savino F, Castagno E, Calabrese R, Viola S, Oggero R, Miniero R. High faecal calprotectin levels in healthy, exclusively breast-fed infants. Neonatology. 2010; 97:299–304.

24. Campeotto F, Kalach N, Lapillonne A, Butel MJ, Dupont C, Kapel N. Time course of faecal calprotectin in preterm newborns during the first month of life. Acta Paediatr. 2007; 96:1531–1533.

25. Yang Q, Smith PB, Goldberg RN, Cotten CM. Dynamic change of fecal calprotectin in very low birth weight infants during the first month of life. Neonatology. 2008; 94:267–271.

26. Sangild PT. Gut responses to enteral nutrition in preterm infants and animals. Exp Biol Med (Maywood). 2006; 231:1695–1711.

27. Kim YJ. Enteral nutrition and its clinical application. Korean J Pediatr Gastroenterol Nutr. 2009; 12:Suppl 1. S27–S36.

28. Wu G, Jaeger LA, Bazer FW, Rhoads JM. Arginine deficiency in preterm infants: biochemical mechanisms and nutritional implications. J Nutr Biochem. 2004; 15:442–451.

29. Buddington RK, Elnif J, Puchal-Gardiner AA, Sangild PT. Intestinal apical amino acid absorption during development of the pig. Am J Physiol Regul Integr Comp Physiol. 2001; 280:R241–R247.

30. Bjornvad CR, Schmidt M, Petersen YM, Jensen SK, Offenberg H, Elnif J, et al. Preterm birth makes the immature intestine sensitive to feeding-induced intestinal atrophy. Am J Physiol Regul Integr Comp Physiol. 2005; 289:R1212–R1222.

31. Rigo J, Salle BL, Picaud JC, Putet G, Senterre J. Nutritional evaluation of protein hydrolysate formulas. Eur J Clin Nutr. 1995; 49:Suppl 1. S26–S38.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download