Abstract
Purpose
Lactose intolerance (LI) is perceived to be frequent in Asia and has been reported to have considerable impact on dietary intake, nutritional status and the quality of life. We aimed to gather information from healthcare professionals on the perceived incidence, diagnosis and management of LI in 1 to 5 year old children in Southeast Asia.
Methods
An anonymous electronic survey was sent randomly among healthcare professionals registered in the database of the pediatric societies in Thailand, Indonesia, and Singapore between June and October 2016.
Results
In total, 259 health care professionals responded of which 45.5% (n=118) were from Thailand, 37.4% (n=97) from Indonesia and 16.9% (n=44) from Singapore. Of the participants who responded (n=248), primary LI prevalence among children 1 to 3 years of age was estimated to be less than 5% by 56.8%. However, about 18.9% (n=47) answered they did not know/unsure. Regarding secondary LI, 61.6% of respondents (n=153) estimated the prevalence to be less than 15%. But again, 10.8% (n=27) answered they did not know or unsure. Rotavirus gastroenteritis was ranked as the top cause for secondary LI. There was considerable heterogeneity in the diagnostic methods used. The majority of respondents (75%) recommended lactose-free milk to manage primary and secondary LI.
Lactose intolerance (LI) is defined as the inability to digest dietary lactose. It is a common condition in the Asian population and has been reported to have a direct impact on dietary habits, nutritional status and quality of life [123].
LI is characterised by symptoms such as abdominal pain, bloating, flatulence and diarrhea [45]. LI can be defined as primary and secondary LI depending on the etiology. Primary LI is the result of primary lactase deficiency linked to genetic factors and is usually built up over time, resulting in a chronic LI. Congenital early onset primary lactase deficiency, which results in the inability to digest even breast milk, is extremely rare. Secondary LI may occur as the result of an underlying condition causing lactase deficiency leading to lactose malabsorption. It can develop at any age and is transient if the cause of the LI is recognised and adequately treated. The severities of symptoms due to the LI vary between individuals depending on the amount of enzyme remaining and other factors such as the amount of ingested lactose and gastro-intestinal transit time [1].
Little is known about regional differences and age of onset of primary LI [6] as it has been attributed to a combination of genetic factors and environmental factors [45]. LI has been suggested to be more prominent in older school-aged children because lactase activity does not decrease before the age of three years, in combination with a decrease of the consumption of lactose-containing foods [7]. However, a recent systematic review concluded that there is in fact little data to support this assumption, and that criteria and the methodology for the diagnosis of LI differ broadly [6]. The lack of consensus about adequate methods for LI diagnosis adds to the perceived heterogeneity of LI prevalence, including those in Asia.
Over-diagnosis of LI may lead to unnecessary recommendation of lactose-free foods which may impact the dietary pattern and nutritional status of the child. As an example, dairy products which contain considerable levels of lactose are good sources of calcium, protein and vitamin D which are important for bone health in a growing child [5]. Under-diagnosis may cause inadequate treatments, including nutritional interventions, and unneeded investigations.
Electronic surveys among healthcare professionals have been widely acknowledged as a reliable method to gather information due to their advantages such as ease of implementation and cost-effectiveness [8]. Since data on the prevalence and management of LI are scarce, especially for South East Asia, an electronic survey was conducted amongst healthcare professionals on the perceived prevalence of LI and its diagnosis in 1 to 5 year old children.
A link to an electronic survey using dedicated software (www.surveymonkey.com) was sent via email to selected members of the pediatric societies in Thailand (n=118), Indonesia (n=100), and Singapore (n=100), between July and September 2016. Ethical approval was obtained from the Singapore National Healthcare Group Domain Specific Review Board (NHG DSRB Ref no: 2015/0128) for the survey to be conducted in these three countries. Since the survey was anonymous, the waiver of informed consent request was approved by the DSRB. The questionnaire was developed by the authors and consisted of 13 questions which included demographics of the participants (4 questions asking the position title/function, setting of the current practice, country and years of practice), perceived incidence of LI (4 questions asking whether they distinguish primary and secondary LI, the estimate of the average incidence of children 1 to 3 years old with primary LI seen in the last 6 months, a similar question for 3 to 5 years old children and the last question for incidence of children 1 to 5 year old with secondary LI), perceived etiology of LI and diagnosis (2 questions—one for the etiology and one for the method commonly used for diagnosis) and final 3 questions on management of LI. The participants were asked to provide their best estimates for what they have seen or diagnosed/managed. The survey did not require any personal data collection and participation was on a voluntary basis. No incentive was given to the participants.
In order to make the survey responses as close-ended as possible, several options were provided for each question for the respondent to select from. Accordingly, the cut-off points for the percentage prevalence of LI were arbitrarily selected based on the systematic review by Harvey et al. [6] which found the prevalence of LI to be quite low.
Also, even though the questionnaire used the term ‘incidence’, for example, “What would be your best estimate incidence of children 1 to 3 year old with PRIMARY LI you have seen or diagnosed in YOUR COUNTRY in the last 6 months?”, the term is adjusted and referred in the manuscript as ‘prevalence’. This is because, since the survey asked the incidence within the last 6 months, it could refer to a proportion from the number of patients that the respondents observed, actually what the question referred to is prevalence.
The response rate of randomly selected participants in this survey is about 80%. A total of 259 responses were obtained as follows: 45.5% (n=118) responses from Thailand (of which 45.8% from public sectors), 37.4% (n=97) responses from Indonesia (of which 53.6% from public sectors), and 16.9% (n=44) responses from Singapore (of which 75.0% from public sectors). The respondents were mainly paediatricians (94.2%, n=244) and some general practitioner(s) (2.3%, n=6), and others (3.4%, n=9) consisting of paediatric resident(s) (n=6), a neonatologist, a retired doctor and a midwife. The respondents had comparable clinical experience; i.e., 33% having less than 5 years of experience, 35% with 5 to 15 years of experience, and the others had more than 15 years of experience. There was an average non-response rate across all questions of approximately 20%.
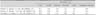
Around 95.7% (n=248) of the surveyed population responded to the estimated prevalence of primary and secondary LI. The majority of the respondents (56.8%, n=141) estimated primary LI in 1 to 3 years old to be less than 5%, while 24.1% (n=60) believed it to be higher, varying between 5% and >20% and 18.9% (n=47) was either unsure/don't know (Table 1). A similar majority (54.0%, n=134) estimated the prevalence of primary LI also to be less than 5% in children >3 to 5 years old. Around 24.1% (n=60) believed LI to be considerably higher than 5%, while 21.3% (n=53) was either unsure/don't know (Table 1). Regarding secondary LI, around 61.6% participants (n=153) estimated its prevalence among children 1 to 5 years old was less than 15% (17% reporting <5% prevalence, 24% reporting 5% to 9.9% prevalence and 21% reporting 10% to 14.9% prevalence) and 10.8% (n=27) were either unsure/don't know (Table 1). Around 89.9% (n=233) of participants reported gastroenteritis (GE) to be the main cause for secondary LI; of which 89.6% (n=209) perceived rotavirus GE to be a more common cause than non-rotavirus GE.
In multiple responses, according to the respondents (n=259), the most commonly used methods to diagnose LI are based on symptoms and response to dietary elimination of lactose (88.0%, n=228), stool pH (21.2%, n=55), and milk challenge test (25.9%, n=67). At least three-quarter of the respondents would recommend a lactose-free milk to manage primary and secondary LI, while 5% of respondents would recommend total milk avoidance in primary LI.
No striking differences were noted among the respondents from the three countries, despite the countries' differences in health services based on the recent World Health Organization (WHO) ranking on sustainable development goals [9]. Therefore, the overall results (instead of individual countries) were being presented in this paper.
To our knowledge, this is the first survey conducted across three different countries in South East Asia which attempted to address the prevalence of primary and secondary LI. Majority of the respondents perceived that the estimated prevalence rate of primary LI in 1 to 3 years old was comparable to those in >3 to 5 years old (which is less than 5%).
This is in contrast with the common belief that the prevalence of primary LI is much higher in older children [6]. In addition, the reported prevalence of lactose malabsorption measured with a hydrogen breath test in children 1 to 3 year old in Myanmar was 16.7% [10] and among children 3 to 5 year old in China was 12.2% [11]. However, LI includes only symptomatic individuals while malabsorption includes individuals in whom the non-absorbed lactose does not induce symptoms. In other words, lactose malabsorption is more frequent than LI.
The lower estimated prevalence of primary LI in this survey could also be due to the fact that parents of children with problems when consuming lactose-containing food or drink may not see a doctor and choose to implement a pragmatic approach such as milk avoidance. Lack of understanding of LI symptoms may also result in parents not bringing their child to a doctor if symptoms occurred after consumption of lactose-containing foods. In addition, there was a significant number of respondents (about 20%) who was “unsure” or “did not know” of the prevalence, highlighting the need for further education and training on the topics.
Most respondents estimated that the prevalence of secondary LI was between 5.0% and 9.9%. This is again quite a low prevalence in comparison to the reported prevalence in a recent systematic review which indicated a prevalence of 16% to 19% among 3 to 5 year old children in Germany and Spain [6]. The latter reported the prevalence of secondary LI due to rotavirus GE was around 16.9% among children in Spain [12], while among infants who suffered from rotavirus GE in China, the prevalence can reach as high as 67% [13]. The estimated prevalence of secondary LI in this survey seemed to be underestimated given that the incidence of GE in this region has been constantly high [14] and there is possibility of late-onset of congenital lactase deficiency among Asian children which was earlier reported to be observed at 4 to 5 years of age [15].
In this survey, clinical diagnosis was reported as the most preferred method for the diagnosis of LI. Although a good clinical history often reveals a relationship between lactose ingestion and symptoms, only objective measurements can confirm the diagnosis of LI. A confirmed diagnosis may allow adequate treatment and restriction of lactose-containing foods. Several methods have been validated to diagnose LI [6]. Among the diagnostic methods reported, stool pH and hydrogen breath test were reported as the most popular. The latter has been accepted as the gold standard of non-invasive testing for detecting lactase deficiency also in younger children [16]. False negative results are related to the inability of the colonic microbiome to produce hydrogen after ingestion of lactose as may occur after a recent intake of antibiotics or in a situation of rapid transit such as in acute diarrhoea. Therefore, the WHO did not recommend the hydrogen breath test as a standard test to diagnose LI in daily clinical practice [17].
When LI is suspected, a lactose-free or lactose-restricted diet is often recommended as reported in this survey. The degree of lactase deficiency differs among patients, what results in tolerance of varying amounts of dietary lactose. As high as 12 g of total lactose (amount in an 8-oz glass of milk) may be required to induce symptoms in children with chronic abdominal pain [18]. Thus, understanding the level of lactose tolerance is important in order to select appropriate lactose-containing foods based on estimates of digestible lactose [2].
Avoidance of (any) milk products to manage LI-related symptoms may be problematic for optimal bone mineralization especially for these younger age groups. Children who avoid milk generally consume less than recommended amounts of calcium, protein and vitamin D needed for normal bone calcium accretion and bone mineralization. Although calcium can be provided by alternate non-dairy dietary sources or as a dietary supplement, individuals who avoid milk intake also need to fulfill the protein requirement and other nutrients which are essential to support growth during childhood [19].
There are several limitations of this survey. Nearly 20% of respondents either did not answer a specific question or chose the option “unsure”. There was also no further demographic information on those who did not answer or chose the ‘unsure option’. These disadvantages could easily change the distribution of responses for each question and affect the conclusion. Also, in this survey, we defined general hospital as a government-owned hospital. The definition of third degree or community hospital was not further elaborated. The non-response rate in this survey was comparable with those reported earlier [8]. Since the participants are randomly selected, this could introduce a selection bias. In addition, the selected countries may not be representative for the entire South East Asia region. Lastly, the data generated represent perceived estimates by healthcare professionals.
The majority of the respondents estimated the prevalence of primary LI in children under the age of 5 years to be less than 5%, which is in accordance to literature. However, the most striking result is that about 20% of the respondents had no idea of the prevalence of primary LI in this age group, highlighting the need for training and education. The majority estimated the prevalence of secondary LI to be less than 15%, what is likely to seriously underestimate its prevalence as reported from other recent studies. These findings in combination with about 10% of the respondents unaware of the prevalence, highlights again the need for education and training on diagnosis and management of LI among young children. The current information should serve as a starting point to set up education programs and could help to prevent unnecessary avoidance of lactose-containing food such as milk in children 1 to 5 years. We are concerned that there may be unnecessary avoidance of lactose-containing food in children since they may be being falsely labelled as lactose intolerant.
The estimated prevalence of primary LI in children under the age of 5 years among the survey's participants is consistent with earlier reports, which was less than 5%. The estimated prevalence of secondary LI was less than 15%. This seemed to be underestimated in view of high prevalence of GE and the possible late-onset of congenital lactase deficiency among young children in South East Asia region.
The diagnosis and management of LI among paediatricians in the region appeared to be based more on clinical symptoms. The data from this survey could be a starting point to prevent unnecessary avoidance of lactose-containing food such as milk in children 1 to 5 years. Further education or training among healthcare professionals and epidemiological studies using standardized methods for diagnosis of LI are required.
ACKNOWLEDGEMENTS
The authors, Michelle LN Tan and Seng Hock Quak received an educational grant from Danone Nutricia Early Life Nutrition, Nutricia Research, Singapore as principal investigator to conduct and publish the survey. Leilani Muhardi, Thomas Ludwig, Jacques Bindels, and Eline M Van der Beek are employees of Danone Nutricia Early Life Nutrition, Nutricia Research. We thank Dr. Dimple Rajgor for her assistance in editing, formatting, reviewing, and in submitting the manuscript for publication.
References
1. Heyman MB. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006; 118:1279–1286.

2. Lukito W, Malik SG, Surono IS, Wahlqvist ML. From ‘lactose intolerance’ to ‘lactose nutrition’. Asia Pac J Clin Nutr. 2015; 24:Suppl 1. S1–S8.
3. Wahlqvist ML. Lactose nutrition in lactase nonpersisters. Asia Pac J Clin Nutr. 2015; 24:Suppl 1. S21–S25.
4. Perino A, Cabras S, Obinu D, Cavalli Sforza L. Lactose intolerance: a non-allergic disorder often managed by allergologists. Eur Ann Allergy Clin Immunol. 2009; 41:3–16.
5. EFSA Panel on Dietetic Products NaAN. Scientific opinion on lactose thresholds in lactose intolerance and galactosaemia. EFSA J. 2010; 8:1777.
6. Harvey L, Ludwig T, Hou AQ, Hock QS, Tan ML, Osatakul S, et al. Prevalence, cause and diagnosis of lactose intolerance in children aged 1–5 years: a systematic review of 1995–2015 literature. Asia Pac J Clin Nutr. 2018; 27:29–46.
7. Hegar B, Widodo A. Lactose intolerance in Indonesian children. Asia Pac J Clin Nutr. 2015; 24:Suppl 1. S31–S40.
8. Braithwaite D, Emery J, De Lusignan S, Sutton S. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003; 20:545–551.

9. GBD 2015 SDG Collaborators. Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016; 388:1813–1850.
10. Myo-Khin , Bolin TD, Khin-Mar-Oo , Tin-Oo , Kyaw-Hla S, Thein-Myint T. Ineffectiveness of breath methane excretion as a diagnostic test for lactose malabsorption. J Pediatr Gastroenterol Nutr. 1999; 28:474–479.

11. Yang Y, He M, Cui H, Bian L, Wang Z. The prevalence of lactase deficiency and lactose intolerance in Chinese children of different ages. Chin Med J (Engl). 2000; 113:1129–1132.
12. Gonzalez-Galan V, Sánchez-Fauqier A, Obando I, Montero V, Fernandez M, Torres MJ, et al. High prevalence of community-acquired norovirus gastroenteritis among hospitalized children: a prospective study. Clin Microbiol Infect. 2011; 17:1895–1899.

13. Hu Y, Gui L, Chang J, Liu J, Xu S, Deng C, et al. The incidence of infants with rotavirus enteritis combined with lactose intolerance. Pak J Pharm Sci. 2016; 29:1 Suppl. 321–323.
14. Fischer Walker CL, Black RE. Rotavirus vaccine and diarrhea mortality: quantifying regional variation in effect size. BMC Public Health. 2011; 11:Suppl 3. S16.

15. Vandenplas Y. Lactose intolerance. Asia Pac J Clin Nutr. 2015; 24:Suppl 1. S9–S13.
16. Newcomer AD, McGill DB, Thomas PJ, Hofmann AF. Prospective comparison of indirect methods for detecting lactase deficiency. N Engl J Med. 1975; 293:1232–1236.

17. Schirru E, Corona V, Usai-Satta P, Scarpa M, Cucca F, De Virgiliis S, et al. Decline of lactase activity and c/t-13910 variant in Sardinian childhood. J Pediatr Gastroenterol Nutr. 2007; 45:503–506.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download