Abstract
Background
The objective of this study was to compare hemodynamic and recovery characteristics of total intravenous anesthesia using propofol target-controlled infusion (TCI) versus sevoflurane for extraction of four third molar teeth.
Methods
One hundred patients undergoing extraction of four third molar teeth under general anesthesia were randomized to one of two groups. Group 1 received propofol TCI-oxygen for induction and propofol TCI-oxygen-air for maintenance. Group II received a propofol bolus of 2 mg/kg for induction and sevoflurane-oxygen-air for maintenance. Heart rate, mean arterial pressure (MAP), operating time, time to emergence, nausea and vomiting, and sedation and pain scores were measured in each group.
Results
Demographic data, including age, gender, weight, and height, were not significantly different between the two groups. The MAP was significantly higher after intubation (P = 0.007) and injection of anesthesia (P = 0.004) in the propofol group than in the sevoflurane group, with significant reflex bradycardia (P = 0.028). The mean time to emergence from anesthesia using propofol was 25 s shorter than that of sevoflurane (P = 0.02). Postoperatively, the propofol group was less sedated than the sevoflurane group at 30 min (0.02 versus 0.12), but this difference was not significant (P = 0.065).
Conclusion
Both propofol TCI and sevoflurane are good alternatives for induction and maintenance of anesthesia for short day-case surgery. However, propofol TCI does not blunt the hemodynamic response to sudden, severe stimuli as strongly as sevoflurane, and this limitation may be a cause for concern in patients with cardiac comorbidities.
The extraction of four third molar teeth under general anesthesia is one of the most common day-case procedures performed in operating theatres. Day-case anesthesia requires smooth induction, intraoperative hemodynamic stability, rapid recovery of cognitive function after the procedure, and minimal postoperative side effects such as pain, nausea, and vomiting.
The use of sevoflurane is common because of its high potency, low blood-gas partition coefficient allowing rapid induction and awakening [1], stable hemodynamic properties, and relatively low cost. Propofol has been associated with rapid recovery, low incidence of postoperative nausea and vomiting [2], and a possible decrease in postoperative pain [3], which are desirable in day-case surgery. The development of target-controlled infusion (TCI) pharmacokinetic models such as those of Marsh and Schnider [45] have allowed easier and more precise delivery of propofol for maintaining anesthesia using TCI-programmed pumps [67]. Propofol has a direct arterial vasodilator effect and reduces stroke volume more strongly than sevoflurane [8]. However, the effects of propofol on intraoperative hemodynamic stability are yet unknown [910].
In the past, it was difficult to compare these two different anesthetic techniques because standardizing the depth of anesthesia was unfeasible [29111213]. However, new depth of anesthesia monitors such as bispectral index monitoring and entropy monitoring developed by Datex-Ohmeda [1415] have allowed controlling the depth of anesthesia in the intraoperative period. In this study, hemodynamic stability and the postoperative levels of sedation, nausea and vomiting, and pain were compared between these two methods using a known depth of anesthesia.
This study was carried out from June 21, 2016, to January 12, 2018. One hundred consenting patients who were scheduled for extraction of four third molars at the Holroyd Private Hospital were randomized to one of two groups, with 50 patients in each group. Written informed consent was obtained from all patients. The study was approved by the Research Ethics Committee of Holroyd Private Hospital (Approval Number HPH 02082016:4.6). The only exclusion criterion was allergy to any of the study medications.
After enrolment, the patients were prospectively and randomly assigned to one of two study groups by drawing out sticks from a bag labeled as “sevoflurane” or “propofol.” The patients were maintained under anesthesia using either intravenous propofol with target-controlled infusion (group P) or sevoflurane (group S). The patients and recovery nursing staff were blinded to group assignment.
The patients were not premedicated. In the operating room, standard monitoring was started, and entropy monitoring (Entropy EasyFit sensor, GE Healthcare, Australia) was applied. All patients were induced with midazolam 1 mg and fentanyl 1 mcg/kg. Dexamethasone 8 mg, parecoxib 40 mg, and ondansetron 4 mg were administered immediately after injection of local anesthetic. In group P, anesthesia was induced and maintained using TCI (Injectomat TIVA Agilia syringe pump, Fresenius Kabi, Australia) of propofol. In group S, anesthesia was induced intravenously (IV) using propofol 2 mg/kg and maintained with sevoflurane. Sevoflurane was commenced immediately after induction. Propofol was administered to group P using the pharmacokinetic model of Schnider. Nasal tracheal intubation was facilitated with atracurium 0.4 mg/kg, and the lungs were mechanically ventilated with oxygen: air at a ratio of 1:1 L/min to provide a FiO2 of 60%. The delivery of propofol TCI and sevoflurane was adjusted to keep state entropy between 40 and 55. The surgeon infiltrated 30 mL of bupivacaine 0.25% with adrenaline 1:400,000 in bilateral inferior alveolar nerve blocks plus local infiltration in teeth 18, 28, 38, and 48. At the end of surgery, neostigmine 2.5 mg with glycopyrrolate 0.4 mg IV was used to reverse neuromuscular blockade. Patients were extubated after they could breathe spontaneously and make purposeful movements.
Non-invasive mean arterial blood pressure (MAP) was measured intraoperatively every 2 min. Heart rate and MAP were measured and recorded before operation, during induction, after intubation, and after injection of bupivacaine by the surgeon. The minimum and maximum heart rate and MAP levels were also recorded during surgery. The time to emergence from anesthesia was considered the time in which either sevoflurane or propofol TCI was ceased to the time in which state entropy was >80 or the patient could make purposeful movements.
In the post-anesthesia care unit (PACU), postoperative pain was treated with fentanyl boluses. In the PACU, the incidence of nausea and vomiting, amount of administered fentanyl, and the pain scores using the visual analog scale (VAS) at 30 min after arrival in the PACU were recorded. Sedation was measured at 0 and 30 min after arrival in the PACU using a four-point scale (0, fully awake; 1, awake but still sedated; 2, asleep but wakes to verbal command; 3, unresponsive). The VAS pain scores were also recorded in the surgical ward 120 min after surgery.
The calculation of sample size was based on previous studies comparing propofol TCI and sevoflurane anesthesia [81116]. Data on patient's age, weight, height, operating time, time to emergence, sedation score, amount of administered fentanyl, VAS pain scores, heart rate, and MAP were analyzed using Student's t-test. Box-and-whisker plots were derived from the above variables.
There was no significant difference in age, weight, height, and operating time between the two groups. The number of male patients in the sevoflurane and propofol group was 27 and 24, respectively (Table 1).
There was no significant intergroup difference in nausea and vomiting, and sedation and postoperative pain scores. The mean time to emergence from anesthesia using propofol was significantly shorter by 25 s compared with that of sevoflurane (P = 0.02) (Table 2).
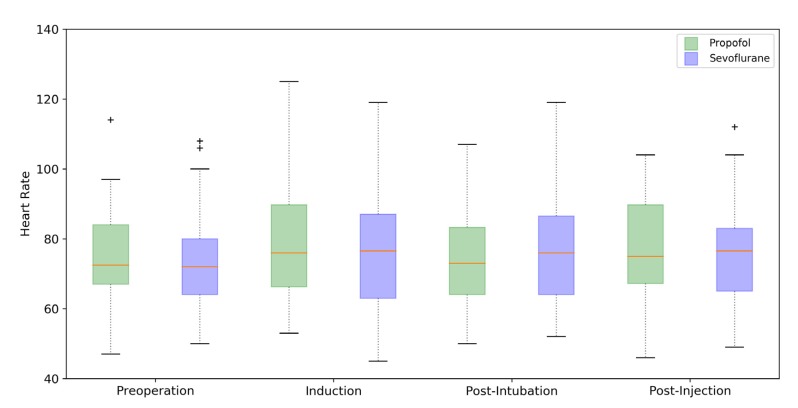
The heart rate was significantly decreased post-intubation in the propofol group compared with the sevoflurane group (P = 0.028). In the propofol group, the heart rate was decreased from induction to intubation (mean = −4.100) and from injection to induction (mean = −1.380) (Table 3, Fig 1, and 2).
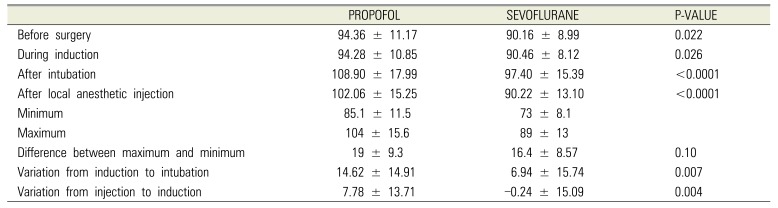
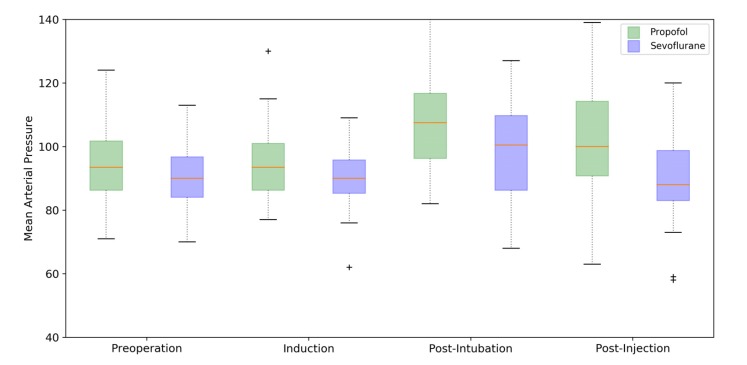
The MAP was significantly higher in the propofol group before operation, during induction, after intubation, and after injection of local anesthesia compared with the sevoflurane group. The MAP in the sevoflurane group was lower after injection than during induction (mean = −0.240 mmHg). The variation in the MPA from induction to intubation (P = 0.007) and from injection to induction (P = 0.004) was significantly higher in the propofol group than in the sevoflurane group. There was no significant intergroup difference between the maximum and minimum MAP intraoperatively (P = 0.100) (Table 4).
This study investigated the intraoperative hemodynamic responses and recovery profile of patients who underwent extraction of four third molar teeth and compared maintenance anesthesia using either propofol TCI or sevoflurane. All other aspects of anesthesia regarding the usual routine of the anesthetist and the operating surgeon remained unchanged between the two groups. In addition, the exclusion criteria were minimal to make the study as close as possible to real-life situations.
The results of the MAP during anesthesia are conflicting, and a few studies reported that patients on propofol TCI presented a lower MAP than patients on sevoflurane [816] whereas another study indicated that the rate of hypotension in the sevoflurane group was higher than that in the propofol TCI group [9]. In our study, the MAP was comparatively higher in the propofol group before operation, during induction, after intubation, and after the injection of local anesthetic (Fig. 3). The variation in the MAP from induction to intubation (P = 0.007) and from injection to induction (P = 0.004) was significantly higher in the propofol group than in the sevoflurane group (Fig. 4). Propofol TCI does not blunt the hemodynamic response to painful stimuli as strongly as sevoflurane at the same depth of anesthesia. This result was also evidenced by the presence of reflex bradycardia after intubation and injection of local anesthetic in the propofol group. In this respect, sevoflurane may attenuate arterial baroreceptors [10].
As reported in previous studies, the time to emergence was comparatively shorter in the propofol TCI group [1216], but this difference was less than 30 s, which is not clinically significant. Other studies reported that emergence from anesthesia was faster in patients receiving sevoflurane; however, the lack of monitoring of the depth of anesthesia limits the interpretation of the results [1]. Moreover, a difference in postoperative pain between the two groups was not expected considering the analgesic adjuvants used, particularly local anesthetic block and infiltration.
It is known that the rate of vomiting during tooth extraction is high. Both dexamethasone and ondansetron are given routinely in our practice to prevent this postoperative complication because these drugs target different pathways. The fact that only one patient in the propofol group and two patients in the sevoflurane group experienced nausea suggests that this protocol was effective. Furthermore, none of the evaluated patients had vomiting. Therefore, a larger cohort of patients and the omission of other anti-emetics would be required to detect significant differences in postoperative nausea and vomiting between these two forms of anesthesia, which is beyond the scope of this study.
Previous studies found that both propofol [12] and sevoflurane [1] significantly decreased recovery time in some cases; however, surgical time was longer and the depth of anesthesia was not standardized in these cases [12]. Our results indicated that there was no significant difference in the recovery time between the two groups, and most patients had a sedation score of zero at 30 min after arrival in the PACU (Table 2).
Previously, the higher cost of propofol compared to sevoflurane had discouraged the use of propofol infusions [1113]. However, the cost of a bottle of 50 mL of generic propofol 500 mg at our institution was AUD 0.33, whereas a bottle of 250 mL of sevoflurane was AUD 98, indicating that propofol infusions, even with extra apparatus, including minimum extension tubing and larger syringes, are cheaper than sevoflurane.
In conclusion, for short day-case anesthesia, propofol TCI is cheaper and has a recovery profile similar to that of sevoflurane. However, propofol TCI does not blunt the hemodynamic response to stimuli as strongly as sevoflurane. Notwithstanding, the use of either induction technique is appropriate and depends on patient comorbidities, anesthetist preference, and degree of familiarity with the technique.
Notes
References
1. Raeder J, Gupta A, Pedersen FM. Recovery characteristics of sevoflurane- or propofol-based anaesthesia for day-care surgery. Acta Anaesthesiol Scand. 1997; 41:988–994. PMID: 9311396.

2. Matsuura H, Inoue S, Kawagucji M. The risk of postoperative nausea and vomiting between surgical patients received propofol and sevoflurane anesthesia: A matched study. Acta Anaesthesiol Taiwan. 2016; 54:114–120. PMID: 27825646.

3. Pokkinen SM, Yli-Hankala A, Kalliomaki ML. The effects of propofol vs. sevoflurane on post-operative pain and need of opioid. Acta Anaesthesiol Scand. 2014; 58:980–985. PMID: 25039403.

4. Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol – defining and illuminating the devil in the detail. Br J Anaesth. 2009; 103:26–37. PMID: 19520702.
5. Russell D, Wilkes MP, Hunter SC, Glen JB, Hutton P, Kenny GNC. Manual compared with target-controlled infusion of propofol. Br J Anaesth. 1995; 75:562–566. PMID: 7577281.

6. Glen JB. The development of ‘Diprifusor’: a TCI system for propofol. Anaesthesia. 1998; (53 Suppl 1):13–21.

7. Gray JM, Kenny GN. Development of the technology for ‘Diprifusor’ TCI systems. Anaesthesia. 1998; (53 Suppl 1):22–27. PMID: 9640111.

8. Bharti N, Chari P, Kumar P. Effect of sevoflurane versus propofol-based anesthesia on the hemodynamic response and recovery characteristics in patients undergoing microlaryngeal surgery. Saudi J Anaesth. 2012; 6:380–384. PMID: 23493938.

9. Godet G, Watremez C, Kettani CE, Soriano C, Coriat P. A comparison of sevoflurane, target-controlled infusion propofol, and propofol/isoflurane anesthesia in patients undergoing carotid surgery; a quality of anesthesia and recovery profile. Anesth Analg. 2001; 93:560–565. PMID: 11524318.

10. Shimonov M, Ezri T, Blecher M, Cherniak A, Azamfirei L. Hemodynamic effects of sevoflurane versus propofol anesthesia for laparoscopic radiofrequency ablation of liver tumours. S AFR J Anesth Analg. 2006; 12:149–152.
11. Smith I, Thwaites AJ. Target-controlled propofol vs. sevoflurane; a double-blind, randomized comparison in day-case anaesthesia. Anaesthesia. 1999; 54:745–752. PMID: 10460526.
12. Akkurt BC, Temiz M, Inanoglu K, Aslan A, Turhanoglu S, Asfuroglu Z, et al. Comparison of recovery characteristics, postoperative nausea and vomiting, and gastrointestinal motility with total intravenous anesthesia with propofol versus inhalation anesthesia with desflurane for laparoscopic cholecystectomy: a randomized controlled study. Curr Ther Res Clin Exp. 2009; 70:95–103.

13. Watson KR, Shah MV. Clinical comparison of ‘single agent’ anaesthesia with sevoflurane versus target controlled infusion of propofol. Br J Anaesth. 2000; 85:541–546. PMID: 11064611.

14. Fahy BG, Chau DF. The technology of processed electroencephalogram monitoring devices for assessment of depth of anesthesia. Anesth Analg. 2018; 126:111–117. PMID: 28786839.

15. Ellerkmann RK, Soegle M, Riese G, Zinserling J, Wirz S, Hoeft A, et al. The Entropy Module and Bispectral Index as guidance for propofol-remifentanil anaesthesia in combination with regional anaesthesia compared with a standard clinical practice group. Anaesth Intensive Care. 2010; 38:159–166. PMID: 20191792.

16. Höcker J, Tonner PH, Böllert P, Paris A, Scholz J, Meier-Paika C, et al. Propofol/remifentanil vs. sevoflurane/remifentanil for longlasting surgical procedures: a randomized controlled trial. Anaesthesia. 2006; 61:752–757. PMID: 16867087.
Fig. 2
Box-and-whisker plot comparing the heart rates from anesthetic induction to intubation and from anesthetic injection to induction.
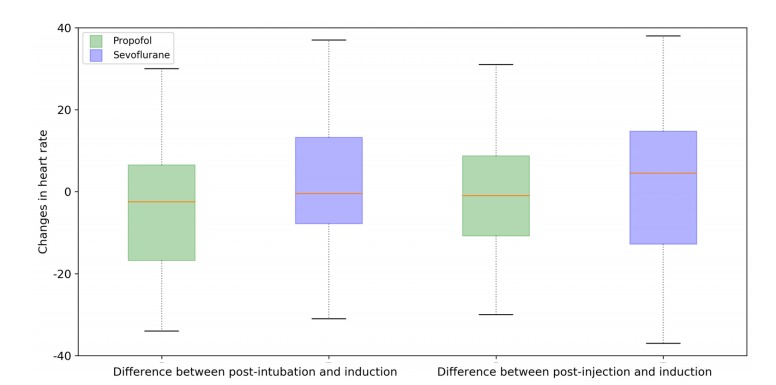
Fig. 4
Box-and-whisker plot comparing the mean arterial pressure from induction to intubation and from injection to induction.
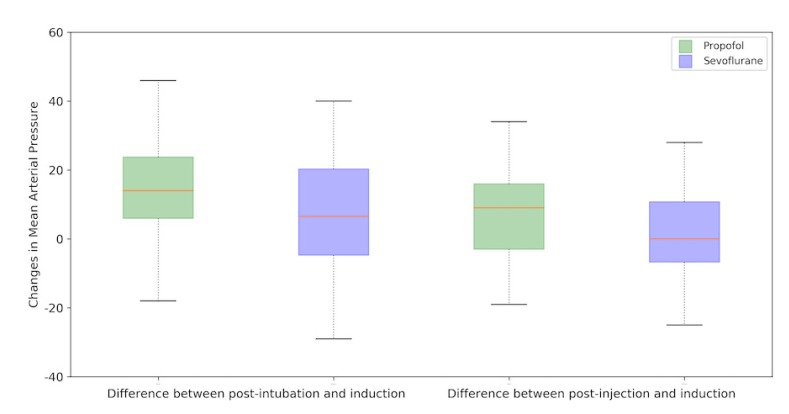
Table 1
Demographic data in the two anesthetic groups. The values are means ± SD or number of occurrences
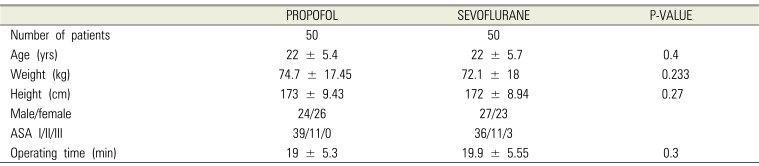
Table 2
Recovery parameters in the two anesthetic groups. The values are means ± SD or number of occurrences. VAS, visual analog scale.
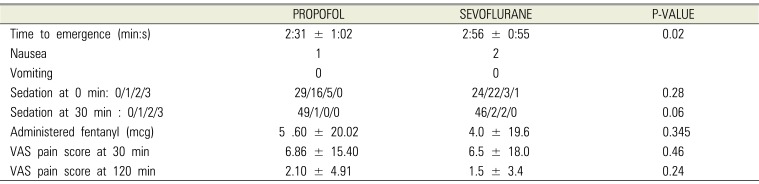
Table 3
Heart rate in the two anesthetic groups. Values are means ± SD.
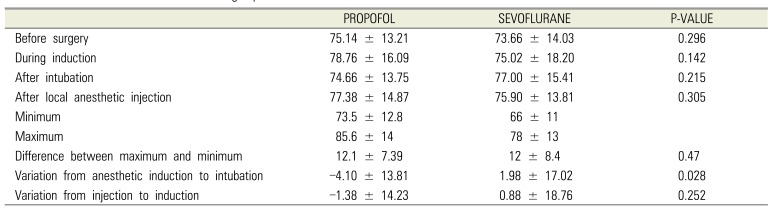
Table 4
Mean arterial blood pressure in the two anesthetic groups. The values are means ± SD.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download