Dear Editor:
Hand eczema, one of the most common dermatological conditions presents with various morphological forms of varying severity and etiology12. Chronic hand eczema is defined as hand eczema that shows a prolonged and relapsing course or is unresponsive to standard treatment using emollients and topical corticosteroids3. It is estimated that 5%~7% of hand eczema patients show severe chronic hand eczema and 2%~4% are unresponsive to standard treatment3. Systemic therapy may be needed in severe, chronic, and refractory cases4. Cyclosporine has been studied at dosing levels of 3 mg/kg/day and 5 mg/kg/day for the treatment of severe chronic hand eczema56. Although patients showed improvement with treatment, frequent relapses were reported shortly after discontinuation of cyclosporine567. Our retrospective study involved a review of medical records and pictures obtained from patients, and evaluation of the clinical efficacy of oral cyclosporine for treatment of patients with chronic hand eczema refractory to conventional therapy.
Among patients who visited the Dermatology Clinic at the National Medical Center, Seoul, Korea between June 2013 and May 2015, we investigated 17 patients with chronic hand eczema that was refractory to conventional treatment. Inclusion criteria for the study were: patients with continuous symptoms over at least a year, patients without a satisfactory response to conventional treatment including systemic steroids, patients without contraindications to use of cyclosporine, patients without history of psoriasis including palmoplantar psoriasis, and those with a negative result on patch testing. Patients were categorized into 3 types based on the features of hand eczema: fissured, hyperkeratotic, and pompholyx type. This study was reviewed and approved by the Institutional Review Board of the National Medical Center (IRB no. H-1612-073-002). Treatment was initiated in all 17 patients with a starting dose of oral cyclosporine administered at 200 mg/day and a maintenance dose of 25~100 mg/day used after an initial response. The starting dose was maintained until the patient achieved at least >50% clearance of palmar lesions. Additionally, the use of topical corticosteroids and emollients was continued as usual. The Static Physician's Global Assessment (sPGA) scores and hand photographs were checked by clinicians for 4 weeks. Efficacy of systemic cyclosporine administration was evaluated using two assessment tools7. These were: 1) The sPGA score to evaluate the severity of hand eczema based on clinician-estimated intensity and assessment of area involved. 2) Photographical assessment using the hand eczema severity index (HECSI). The severity of hand eczema was assessed by two clinicians who performed a detailed study of clinical photographs and calculated a mean score. The primary goal of treatment was to achieve an sPGA score that was clear or almost clear. After achieving the primary goal, the need for a further maintenance period was determined based on patient compliance. Recurrence was defined as a return of the sPGA score to a baseline value. Adverse events associated with use of cyclosporine were evaluated at each follow-up.
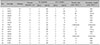
Our study included 10 (58.8%) men and seven (41.2%) women with mean age of 49 years, and a mean disease duration of 2.4 years. Occupation wise, seven patients (41.2%) were homemakers, five patients (29.4%) were office worker, two patients (11.8%) were market workers, and one patient (5.9%) was a construction worker. The medication was discontinued in one patient after 5 days of treatment due to dizziness. We compared the result of sPGA and HECSI before and after treatment for 4 weeks (Fig. 1). An sPGA score of 0 or 1 (clear or almost clear) was noted in four patients (25%) at week 4. There was 32.1% improvement in the sPGA from 2.8 to 1.9 indicating that the severity of the disease decreased from moderate to mild. HECSI showed prominent improvement by 53.9% after 4 weeks of treatment decreasing from 43.4 to 20. An sPGA score of 1 (almost clear) was achieved in 14 of 16 patients, and the mean treatment duration required to achieve this sPGA score of 1 was 9.9 weeks. After achieving an sPGA score of 1, eight patients discontinued medication use while six patients continued maintenance doses of cyclosporine for 1 to 10 weeks (Table 1). Recurrence was observed in four patients, and a mean remission period in these patients was 2.3 months. No patient reported severe adverse effects. Mild elevation in blood pressure was observed in four patients, which did show normalization following reduction/discontinuation of cyclosporine.
The first published report describing hand eczema treated with cyclosporine was a case of recalcitrant chronic vesicular hand eczema6. The patient showed remarkable improvement within 2 weeks of cyclosporine therapy administered as a daily dose of 5.0 mg/kg. Previous studies reporting the role of systemic cyclosporine treatment for hand eczema patients used simplified tools such as PGA for clinical assessment; therefore, its efficacy might have been under- or over-estimated based on a physician's subjective opinion. We attempted an objective and accurate assessment of clinical improvement using clinical photographs and detailed scales and evaluation by two physicians. In this study, based on the clinicians' evaluation, a satisfactory response was obtained after 4 weeks of treatment. We found that 14 of 16 patients achieved an sPGA score 0 or 1 and showed a variable remission period. Recurrence was observed in four patients during the follow up period, although three of these four had received maintenance doses. The small sample size was a limitation of our study. Because a small number of patients was evaluated, we could not determine the relevant factors influencing relapse of hand eczema including disease duration and subtypes. Patients showed no adverse effects necessitating withdrawal of the medication. A short remission period and a high recurrence rate were drawbacks associated with cyclosporine use in patients showing hand eczema. However, combination therapy using low-dose cyclosporine over a prolonged maintenance period and topical corticosteroids may be helpful. We propose that cyclosporine can be an effective and safe treatment option in cases of chronic hand eczema refractory to standard treatment.
Figures and Tables
References
1. Lakshmi C, Srinivas CR. Hand eczema: an update. Indian J Dermatol Venereol Leprol. 2012; 78:569–582.

2. Johansen JD, Hald M, Andersen BL, Laurberg G, Danielsen A, Avnstorp C, et al. Classification of hand eczema: clinical and aetiological types. Based on the guideline of the Danish Contact Dermatitis Group. Contact Dermatitis. 2011; 65:13–21.

3. Diepgen TL, Agner T, Aberer W, Berth-Jones J, Cambazard F, Elsner P, et al. Management of chronic hand eczema. Contact Dermatitis. 2007; 57:203–210.

4. Bissonnette R, Diepgen TL, Elsner P, English J, Graham-Brown R, Homey B, et al. Redefining treatment options in chronic hand eczema (CHE). J Eur Acad Dermatol Venereol. 2010; 24:Suppl 3. 1–20.

5. Granlund H, Erkko P, Eriksson E, Reitamo S. Comparison of cyclosporine and topical betamethasone-17,21-dipropionate in the treatment of severe chronic hand eczema. Acta Derm Venereol. 1996; 76:371–376.
6. Petersen CS, Menné T. Cyclosporin A responsive chronic severe vesicular hand eczema. Acta Derm Venereol. 1992; 72:436–437.
7. Granlund H, Erkko P, Reitamo S. Comparison of the influence of cyclosporine and topical betamethasone-17,21-dipropionate treatment on quality of life in chronic hand eczema. Acta Derm Venereol. 1997; 77:54–58.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download