Dear Editor:
Pruritus is one of the most frequent and unpleasant symptoms in patients with chronic renal failure. The reported prevalence ranges from 50% to 90%
1. Pruritus has negative emotional and psychosocial effects and affects patients' quality of life (QOL). Hence, we conducted this study on patients undergoing regular hemodialysis to evaluate the clinical and biochemical data of pruritus and to identify whether pruritus influences QOL.
The study was approved by the Institutional Review Board of the Wonkwang University Hospital (IRB no. 201507-HR-056).
We enrolled 83 patients with end-stage renal disease undergoing regular hemodialysis. The patients agreed to an interview using a questionnaire about pruritus. The questionnaire was designed to evaluate following clinical features of uremic pruritus: intensity of pruritus as quantified by the visual analog scale (VAS, 0~10), and the dermatology life quality index (DLQI, 0~34)
2 to assess the QOL; patient medical records were reviewed retrospectively for identification of associated laboratory parameters.
Zucker's
3 definition was used in this study. Uremic pruritus was defined as appearance soon before the initiation of hemodialysis or during hemodialysis, with no evidence of any other disease that could explain the pruritus. Pruritus was defined as (1) at least three episodes of itching occurring several times a day, for 2 weeks or less, with symptoms lasting a few minutes that were annoying to the patient or (2) cyclic itching over a period of 6 months or more with a lower frequency than in definition (1).
Of the 83 subjects, 38 (45.8%) were men and 45 (54.2%) were women. Ages ranged from 29 to 84 years (mean, 59.8±12.9). The duration of hemodialysis ranged from 1 month to 14 years (mean, 36.3±36.7 months). Pruritus was present in 23 cases (27.7%) at the time of the examination, and 60 (72.3%) had no history of pruritus.
Among the pruritic patients (n=23), the most common location of pruritus was the back (30.4%), followed by the leg (21.7%), abdomen (17.4%), face and neck (17.4%), arm (13.0%), chest (8.7%), and scalp (4.4%), with generalized itching in 13.0%. Most patients had a prolonged duration of pruritus. In 17 patients (73.9%), the symptoms were present for more than 1 year. In 19 patients (82.6%), symptoms appeared more than once a day and either more than once a week or more than once a month in 4 (17.4%). Sleep disturbance caused by pruritus was found in 13 cases (56.5%), with difficulty falling asleep in two (8.7%); Three patients (13.0%) were awakened by pruritus, and eight (34.8%) reported symptoms both while falling asleep and on awakening. In 17 patients (73.9%), dialysis had no effect on pruritus. The intensity of pruritus decreased after hemodialysis treatment in three patients (13.0%), whereas three (13.0%) noted that pruritus was aggravated after treatment.
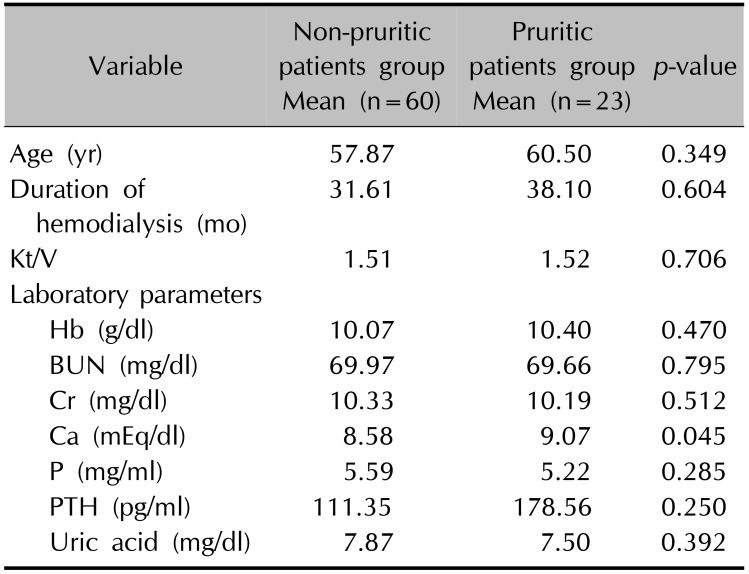
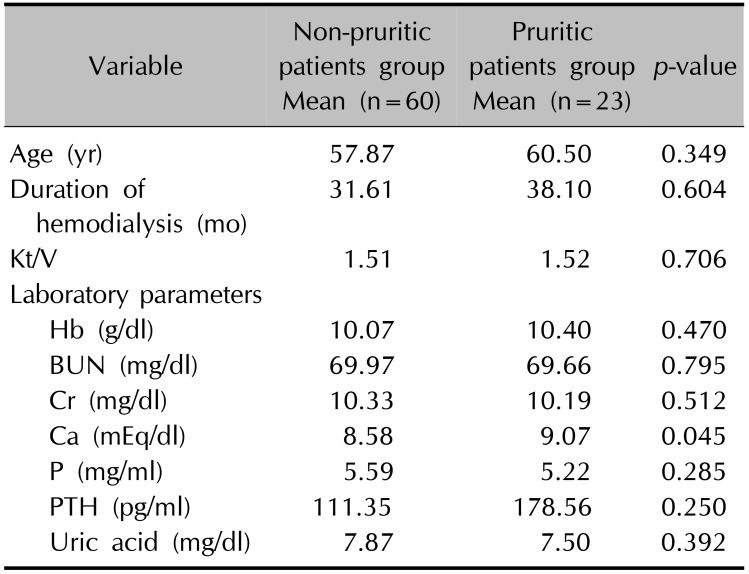
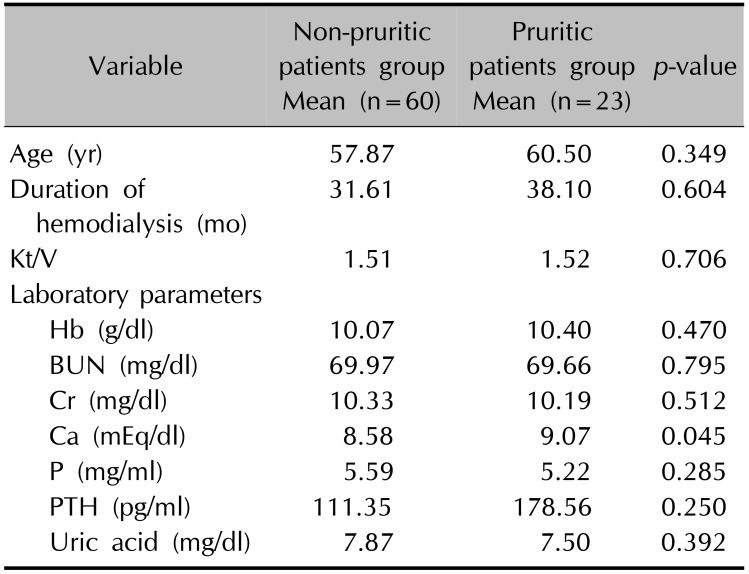
Table 1 shows the differences in serum calcium between pruritic and non-pruritic patients (
p=0.045).
Table 1
Clinical parameters influencing pruritus
|
Variable |
Non-pruritic patients group Mean (n=60) |
Pruritic patients group Mean (n=23) |
p-value |
|
Age (yr) |
57.87 |
60.50 |
0.349 |
|
Duration of hemodialysis (mo) |
31.61 |
38.10 |
0.604 |
|
Kt/V |
1.51 |
1.52 |
0.706 |
|
Laboratory parameters |
|
|
|
|
Hb (g/dl) |
10.07 |
10.40 |
0.470 |
|
BUN (mg/dl) |
69.97 |
69.66 |
0.795 |
|
Cr (mg/dl) |
10.33 |
10.19 |
0.512 |
|
Ca (mEq/dl) |
8.58 |
9.07 |
0.045 |
|
P (mg/ml) |
5.59 |
5.22 |
0.285 |
|
PTH (pg/ml) |
111.35 |
178.56 |
0.250 |
|
Uric acid (mg/dl) |
7.87 |
7.50 |
0.392 |

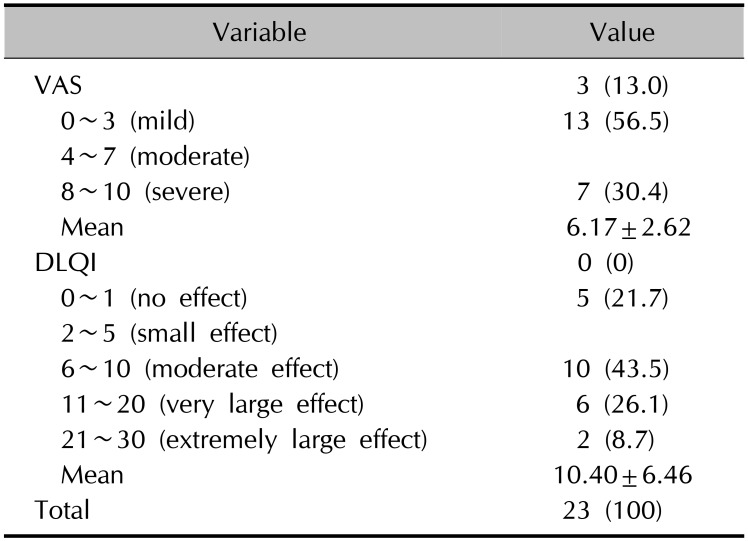
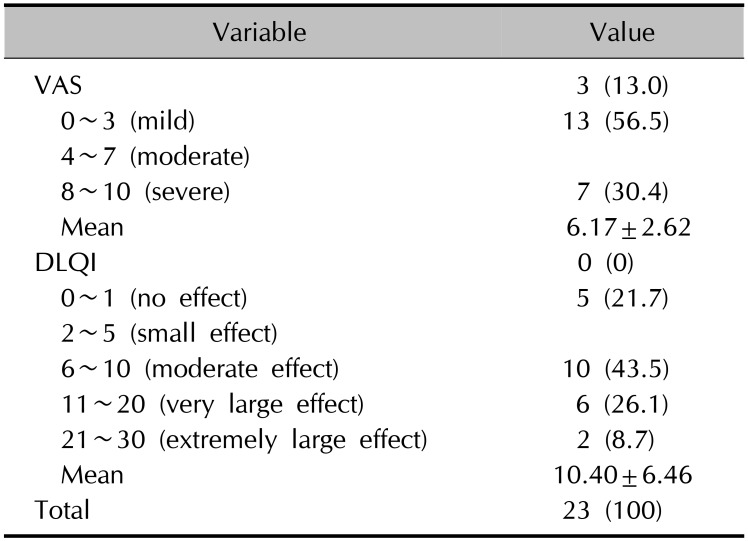
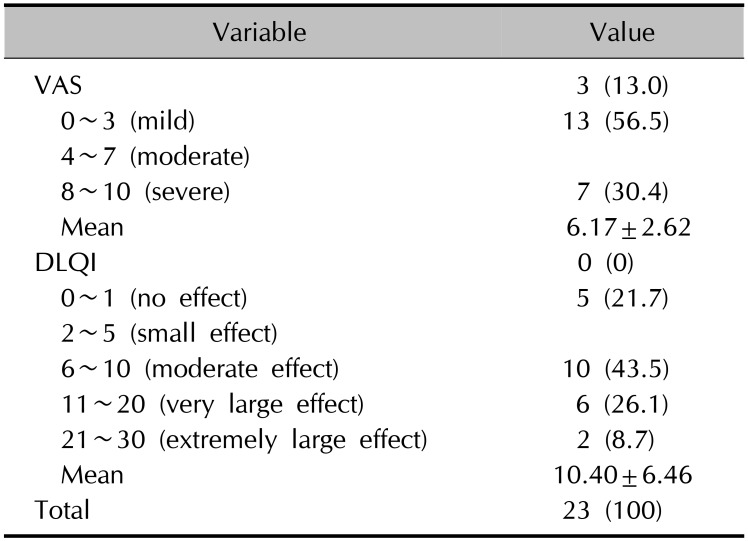
The severity of pruritus assessed with VAS score and the effect of pruritus on QOL evaluated by DLQI are shown in
Table 2.
Table 2
Intensity of pruritus and effect of QOL on pruritus
|
Variable |
Value |
|
VAS 3 (13.0) |
|
|
0~3 (mild) |
13 (56.5) |
|
4~7 (moderate) |
|
|
8~10 (severe) |
7 (30.4) |
|
Mean |
6.17±2.62 |
|
DLQI 0 (0) |
|
|
0~1 (no effect) |
5 (21.7) |
|
2~5 (small effect) |
|
|
6~10 (moderate effect) |
10 (43.5) |
|
11~20 (very large effect) |
6 (26.1) |
|
21~30 (extremely large effect) |
2 (8.7) |
|
Mean |
10.40±6.46 |
|
Total |
23 (100) |

The early prevalence rate of uremic pruritus in maintenance hemodialysis patients is reportedly as high as 86%
4. A study published in 1995 showed a high prevalence of uremic pruritus (59%)
5. Our study revealed a lower prevalence of 27.7%, but the reason is unclear. However, a more precise calculation of dialysis based on Kt/V or creatinine clearance measurements may account for this lower prevalence
6. All patients in the present study underwent hemodialysis using bicarbonate-based dialysate (H.D. Sol-BC A®; GAMBRO Dialysatroren GmbH, Hechingen, Germany), while previous studies used both acetate-based and bicarbonate-based dialysis fluids5. Kt/V values that assessed the adequacy of dialysis were not significantly different between groups with and without pruritus. The analysis of dialysis adequacy using Kt/V quantifies the clearance of small molecules (e.g., urea) and cannot assess the removal of mid- or large-sized molecules
7. Thus, it is thought that the accumulation of mid- or large-sized molecules is the cause of pruritus in recent hemodialysis patients.
In our study, we did not find significant differences in serum hemoglobin, blood urea nitrogen, creatinine, phosphate, uric acid, and the parathyroid hormone of patients with and without pruritus. However, a higher serum calcium level was more commonly associated with pruritus. Prior studies that examined the association between calcium and itching found that hyperparathyroidism was a frequent problem in patients undergoing hemodialysis. Pruritus may recur after parathyroidectomy, when patients are indicated as hypercalcemic and are treated with vitamin D or calcium-containing agents
8. Our study supports the role of calcium as a factor in uremic pruritus. The study examining the skin of hemodialysis patients with pruritus revealed that the calcium ion concentration of the epidermis was distributed equally in all layers, which indicated disruption of the calcium gradient so that water flows towards the epidermis. They found higher transepidermal water loss in dialysis patients with pruritus compared to those without pruritus
9. It is believed that the impaired permeability barrier function could cause itching by drying the skin in a dialysis patient. Therefore, we could elaborate on the importance of moisturization in a dialysis patient. It is speculated that the increase in serum calcium concentration may have affected the level of epidermal calcium concentration.
Pruritus adversely affects sleep and QOL
10. We examined QOL with a DLQI questionnaire. The six categories assessed were mental status, activities of daily living, leisure activities, self-perception, treatment-induced restrictions, and social functions
2. A moderate to extremely large effect on QOL was found in 18 (78.3%) patients. A moderate to severe VAS score reflecting the severity of pruritus was found in 20 (86.9%) patients. There was a positive correlation between DLQI and VAS (
r=0.86,
p=0.01). Long duration, high frequency, and the high intensity of uremic pruritus are very troublesome symptoms, and can impair the QOL. This is reflected in the large percentage of patients with sleep difficulty secondary to pruritus. In conclusion, this study identified the current prevalence of uremic pruritus in hemodialysis patients, and provided information on its clinical features and pathogenesis. The increase in serum calcium concentration in dialysis patients may have affected the level of epidermal calcium concentration. The altered calcium levels will weaken the barrier function of the skin, leading to increased transepidermal water loss, which may cause itching by drying the skin in dialysis patients.