Abstract
The palmaris longus is harvested as a tendon graft in various surgical procedures. Several tests are used to assess the presence of palmaris longus tendon. In the present study, we attempted to assess the interobserver and intraobserver reliability of five of the most famous methods and also the examination of fifth superficial flexor function. Two observers, who had been trained on the tests and had practiced them, examined 105 volunteers on two separate occasions and in 1-month interval the results were recorded. The reliability of each method was assessed with Kappa measurement. Kappa ranged from 0.541 (moderate reliability) to 0.813 (almost complete agreement) for palmaris. The highest interobserver and intraobserver reliability and also the best agreement with other tests were of Schaeffer. The lowest kappa was for Thompson and the others have good to excellent reliability. Kappa for interobserver and intraobserver reliability for the fifth flexor were 0.415 and 0.500 (moderate reliability), respectively. The tests that were assessed have good reliability except for Thompson that has a moderate one. It seems that the standard test (Schaeffer) is the best method for the assessment of the absence or presence of palmaris longus. The method used for the evaluation of fifth superficial flexor variations assessment has a moderate interobserver and intraobserver reliability.
The palmaris longus is a muscle visible as a small tendon between the flexor carpi radialis and the flexor carpi ulnaris, although it is not always present. Palmaris longus and little finger superficial flexor varies anatomically in human body, as one may be present or both are absent in the hand and wrist [1]. These variations may be assessed by several clinical tests and these tests are more superior to the other according to some studies [2345678]. A recent study showed that different tests may suggest different results when the presence of Palmaris Longus is assessed by them [9]. This may represent different results or different interpretations by the examiner. In the present study, we tried to answer the question that when a single examiner examines the presence of Palmaris by several tests, will she/he reach the same result and at different occasions? And, if different examiners perform a single test on a single individual, will the results be the same? We examined our proposal on the assessment of fifth superficial flexor function too. This study aims to assess the interobserver and intraobserver reliability of five of the most famous methods of examination of the presence of palmaris longus and also the examination of fifth superficial flexor function.
This study was performed by two observers (examiners) on 105 volunteers from June 2016 to March 2017. Inclusion criteria for the volunteers includes females and males above 18 years old, informed consent for participation, no history of surgery on the upper limb, no history of neuromuscular disorders. Two final year medical students (examiners) were trained face to face for different tests and then they practice the test several times on a number of out of study volunteers. Five tests were employed for palmaris longus assessment:
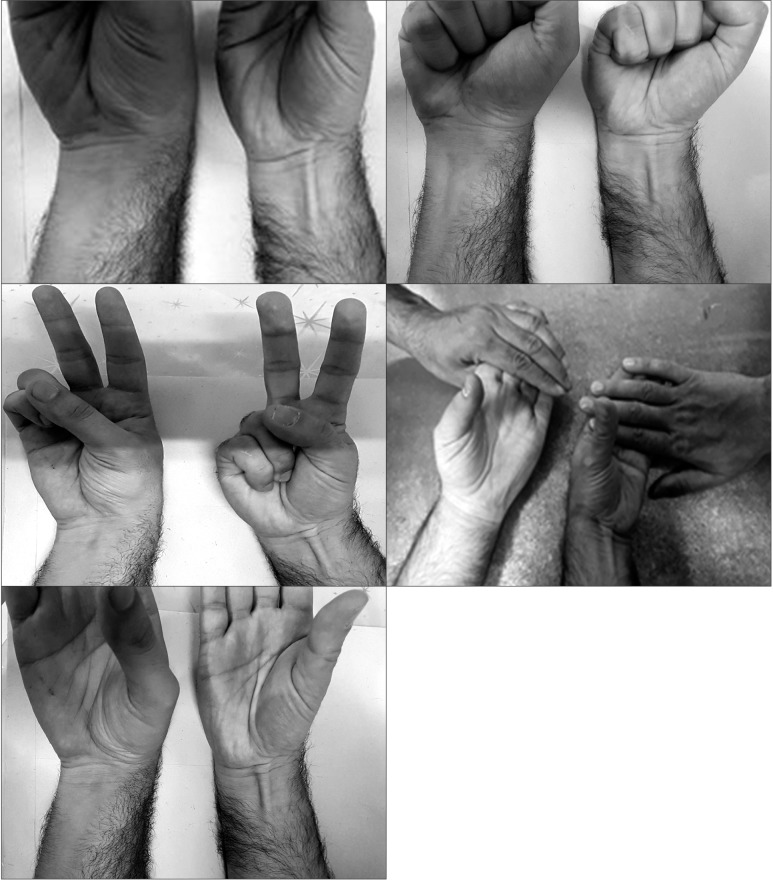
- Schaeffer or standard test (Fig. 1)
- Thompson test (Fig. 2)
- Pushpakumar test (Fig. 3)
- Mishra test (Fig. 4)
- Abnormal Involuntary Movement Scale test (Fig. 5)
Fig. 6 shows all of tests in a hand with and another without Palmaris longus. For fifth flexor, we utilized only the standard test [11] to which the dependent situation was added [12]: the examiner holds the first four fingers of the volunteer in hyperextension and if the fifth finger proximal interphalangeal joint can be flexed to 90°, that means the person has a functional flexor. If she/he cannot perform the task, the fourth finger is released and if the two fingers can be flexed in this situation together then the fifth flexor is dependent and if it is not possible at all, it means that the fifth flexor is absent. Most studies on the topic have utilized this test solely [1314].
Each examiner assessed the 20 volunteers on one occasion and with one test for palmaris and the above mentioned test for fifth flexor. The result was recorded by an out of study person. The volunteer would have palmaris longus present or absent and the fifth superficial flexor absent, present or dependent. At this point, the examiner would return to the first volunteer and examine palmaris presence by another test and again the result would be recorded in the same way. After the first volunteer has finished with the task of utilizing all five tests for palmaris longus, the second examiner would begin and repeat the same process. At the second occasion, one week later, 20 other volunteers were enrolled and this was repeated until the end. At the last occasion, 25 volunteers were examined. One month later, the entire process was repeated. At the end, the results were analyzed with Pentium 4 computer and SPSS version 20 software (IBM Corp., Armonk, NY, USA) by reliability analysis tests and kappa measurement. Kappa was interpreted by previously established criteria [15]: equal or less than zero would mean poor reliability; 0.01 to 0.2, slight; 0.21 to 0.4, fair; 0.41 to 0.6 moderate; 0.61 to 0.8, substantial, and 0.81 to 1 was interpreted as almost perfect.
At the end of the study, 105 volunteers were examined twice and 12 examinations were performed on each individual. So, there were 2,520 results. No loss to follow up occurred and all the volunteers in the first stage were examined again one month after the first examination.
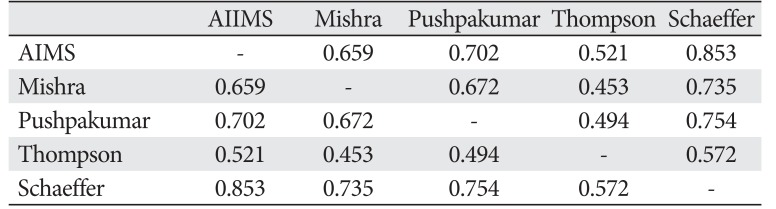
Kappa was calculated for each stage and for each observer of palmaris longus and the mean value for intraobserver reliability is shown in Table 1. Kappa for interobserver reliability of palmaris longus presence is shown in Table 2. The agreement of different tests for palmaris longus presence is shown in Table 3.
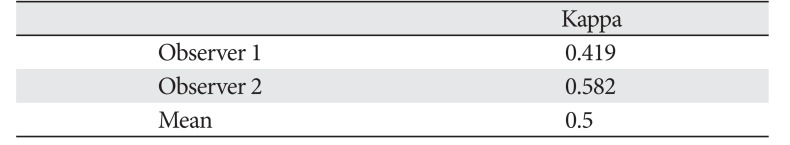
Table 4 shows the results of intraobserver reliability measurement for fifth superficial flexor function assessment by the test we had utilized. Kappa for interobserver reliability was calculated as 0.415.
We assessed the interobserver and intraobserver reliability of different tests commonly utilized for examination of Palmaris longus and fifth superficial flexor and found a relatively high reliability for all of palmaris tests except for Thompson test and medium reliability for flexor.
Palmaris longus is the first choice for tendon and ligament reconstructions [16]. For this reason, it has been the subject of many investigations and an important issue has been its variations in different populations [171819202122232425262728]. The first prerequisite for performing such studies would be the utilization of a test that is “suitable” for assessment of the tendon presence. But, what test is a “suitable” one? Undoubtfully, a test that is simple (easy to understand and perform for both the examiner and the subject, not time consuming, not disturbing for the subject, no need for help from an instrument), easy to interpret, and after this, perhaps the most important characteristic would be high interobserver and intraobserver reliability and in other words repeatability of the results. In this study we reached the conclusion that tests for palmaris longus presence are in the “good” class, considering kappa, except for Thompson which was “moderate.”
Schaeffer was the first to introduce a “test” for the assessment of palmaris longus presence, more than 100 years ago (1909), a method that is considered “standard” nowadays [2]. After this new tests were designed and introduced repeatedly, Mishra proposed to a test that is possible to perform in patients with median nerve palsy and unable to oppose their thumb [19]. The number of these new tests was so increased that the need for them was questioned [20], but the new tests introduction continued [212223]. In the present study, we utilized only five tests among the many proposed, as they were most frequently used in other studies and also for the sake of patience of the examiners and the volunteers.
The most important difficulty encountered in the examination of palmaris longus presence is the misinterpretation of flexor carpi radialis as palmaris longus. Interesting to note that in Thompson test this is likely, as the muscle becomes contracted [24] and perhaps this rationalizes the findings of this present study about lower kappa value of this test.
It has been mentioned that the most accurate test for palmaris longus assessment is the standard or Schaeffer test [25] and the test has been utilized in most studies, in order to have a positive result to be considered by the person having the tendon. In the present study, Schaeffer and Mishra's test showed the best interobserver and intraobserver reliability and Schaeffer had the best agreement with other tests.
In practice, it will be difficult to determine the sensitivity and specificity of the palmaris longus tests, as this necessitates a surgery to examine the result. A study performed to determine the accuracy of sonography for the detection of plantaris tendon showed an interesting design. Patients who were candidates for surgery on their calves for any reason would undergo sonography and the result compared with intraoperative findings [26]. A similar study may be designed for palmaris longus and tests for its detection. But the present study and at least one other studies [22] suggested that not all tests have similar accuracies and this makes an exact study more difficult. Anyway, this may be a good topic for further research.
The present study reached a medium reliability for fifth superficial flexor, which was unexpected. In fact, the examination method was so easy in our mind especially in comparison to other designed methods [272829] that it seemed unnecessary to be assessed for reliability. But the results showed clearly that we were in mistake. We cannot rationalize this findings, except for the possibility that the emphasis on “at least 90 degrees of flexion” may have caused a doubt in the examiner for “functional status” determination. Anyway, this may reflect the need for assessment of other tests, both on themselves and in contrast to the standard method.
The most important limitation of the present study is the limited number of utilized tests. As previously stated for the sake of examiners and volunteers, we enrolled five tests for palmaris and one for fifth flexor, the tests that had been used in most of the previous studies, but there are a large number of tests that were ignored. On the other hand, we are not sure whether this “small” number of tests has caused fatigue in our study population.
Based on the findings of the present study, all of the examined tests for palmaris longus presence assessment have good interobserver and intraobserver reliability, except for Thompson test that showed moderate reliability. Schaeffer test showed the best agreement with other tests. We reached a moderate reliability for fifth superficial flexor.
References
1. Capdarest-Arest N, Gonzalez JP, Turker T. Hypotheses for ongoing evolution of muscles of the upper extremity. Med Hypotheses. 2014; 82:452–456. PMID: 24529649.
2. Schaeffer JP. On the variations of the palmaris longus muscle. Anat Rec. 1909; 3:275–278.
3. Thompson JW, McBatts J, Danforth CH. Hereditary and racial variations in the musculus palmaris longus. Am J Phys Anthropol. 1921; 4:205–218.
4. Mishra S. Alternative tests in demonstrating the presence of palmaris longus. Indian J Plast Surg. 2001; 34:12–14.
5. Pushpakumar SB, Hanson RP, Carroll S. The ‘two finger’ sign: clinical examination of palmaris longus (PL) tendon. Br J Plast Surg. 2004; 57:184–185. PMID: 15037188.
6. Machhindra MV, Garg B, Tiwari V, Kotwal P. AIIMS test: a simple test to look for presence of palmaris longus. Musculoskelet Surg. 2015; 99:155–158. PMID: 25860500.
7. Mahajan AL. The ‘fingers fan out’ sign: stick out your palmaris longus even better. Br J Plast Surg. 2005; 58:278–279. PMID: 15710132.
8. Oudit D, Crawford L, Juma A, Howcroft A. The “four-finger” sign: to demonstrate the palmaris longus tendon. Plast Reconstr Surg. 2005; 116:691–692. PMID: 16079735.
9. Kyung DS, Lee JH, Choi IJ, Kim DK. Different frequency of the absence of the palmaris longus according to assessment methods in a Korean population. Anat Cell Biol. 2012; 45:53–56. PMID: 22536552.
10. Vercruyssen J, Scafoglieri A, Cattrysse E. The impact of palmaris longus muscle on function in sports: an explorative study in elite tennis players and recreational athletes. J Funct Morphol Kinesiol. 2016; 1:167–182.
11. Vučinić N, Erić M, Savić M. How often absence of palmaris longus and functional deficiencyof flexor digitorum superficialis occurs? Acta Orthop Belg. 2016; 82:405–411. PMID: 27682306.
12. Tan JS, Oh L, Louis DS. Variations of the flexor digitorum superficialis as determined by an expanded clinical examination. J Hand Surg Am. 2009; 34:900–906. PMID: 19410995.
13. Guler F, Kose O, Turan A, Baz AB, Akalin S. The prevalence of functional absence of flexor digitorum superficialis to the little finger: a study in a Turkish population. J Plast Surg Hand Surg. 2013; 47:224–227. PMID: 23617293.
14. Raouf HA, Kader GA, Jaradat A, Dharap A, Fadel R, Salem AH. Frequency of palmaris longus absence and its association with other anatomical variations in the Egyptian population. Clin Anat. 2013; 26:572–577. PMID: 23339087.
15. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005; 85:257–268. PMID: 15733050.
16. Cannon DL. Flexor and extensor tendon injuries. In : Canale ST, Beaty JH, editors. Campbell's Operative Orthopedics. 12th ed. St. Louis: Mosby;2013. p. 2213–2247.
17. Ashouri K, Lahiji FA, Esmailijah AA, Hoseini Khameneh SM, Madadi F, Bagheri F, Rahimi M, Zandi R, Safdari F. Palmaris longus agenesis. Iran J Orthop Surg. 2011; 9:18–21.
18. Sebastin SJ, Lim AY. Clinical assessment of absence of the palmaris longus and its association with other anatomical anomalies: a Chinese population study. Ann Acad Med Singapore. 2006; 35:249–253. PMID: 16710495.
19. Sankar KD, Bhanu PS, John SP. Incidence of agenesis of palmaris longus in the Andhra population of India. Indian J Plast Surg. 2011; 44:134–138. PMID: 21713200.
20. Sebastin SJ, Lim AY. Clinical assessment of the palmaris longus: too many newer techniques? J Plast Reconstr Aesthet Surg. 2006; 59:784–786. PMID: 16782584.
21. Sankar KD, Bhanu PS, John SP. Incidence of agenesis of palmaris longus in the Andhra population of India. Indian J Plast Surg. 2011; 44:134–138. PMID: 21713200.
22. Gangata H. The clinical surface anatomy anomalies of the palmaris longus muscle in the Black African population of Zimbabwe and a proposed new testing technique. Clin Anat. 2009; 22:230–235. PMID: 19173262.
23. Hiz Ö, Ediz L, Ceylan MF, Gezici E, Gülcü E, Erden M. Prevalence of the absence of palmaris longus muscle assessed by a new examination test (Hiz-Ediz Test) in the population residing in the area of Van, Turkey. J Clin Exp Invest. 2011; 2:254–259.
24. Kigera JW, Mukwaya S. Frequency of agenesis Palmaris longus through clinical examination: an East African study. PLoS One. 2011; 6:e28997. PMID: 22174943.
25. Kigera JW, Mukwaya S. Clinical assessment of the palmaris longus: accuracy of common tests. Ann Afr Surg. 2012; 9:41–44.
26. Simpson SL, Hertzog MS, Barja RH. The plantaris tendon graft: an ultrasound study. J Hand Surg Am. 1991; 16:708–711. PMID: 1880370.
27. Doğan T, Celebiler O, Gürünlüoğlu R, Bayramiçli M, Numanoçlu A. A new test for superficialis flexor tendon function. Ann Plast Surg. 2000; 45:93–96. PMID: 10917107.
28. Mishra S. A new test for demonstrating the action of flexor digitorum superficialis (FDS) tendon. J Plast Reconstr Aesthet Surg. 2006; 59:1342–1344. PMID: 17113514.
29. Tan J, Kim CH, Lee HJ, Chen J, Chen QZ, Jeon IH. A new examination method for anatomical variations of the flexor digitorum superficialis in the little finger. Clin Orthop Surg. 2013; 5:138–144. PMID: 23730479.
Fig. 1
Schaeffer test. Adapted from Vercruyssen et al. J Funct Morphol Kinesiol 2016;1:167-82, according to the Creative Commons license MDPI [10].
Fig. 2
Thompson test. Adapted from Vercruyssen et al. J Funct Morphol Kinesiol 2016;1:167-82, according to the Creative Commons license MDPI [10].

Fig. 3
Pushpakumar test. Adapted from Vercruyssen et al. J Funct Morphol Kinesiol 2016;1:167-82, according to the Creative Commons license MDPI [10].

Fig. 4
Mishra test. Adapted from Vercruyssen et al. J Funct Morphol Kinesiol 2016;1:167-82, according to the Creative Commons license MDPI [10].

Table 1
Kappa for intraobserver reliability of palmaris longus presence assessment tests
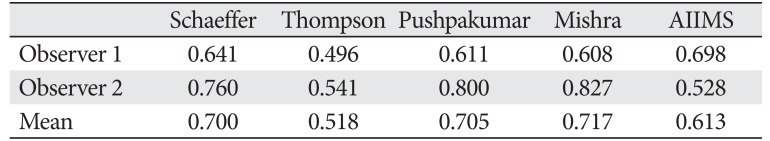
| Schaeffer | Thompson | Pushpakumar | Mishra | AIIMS | |
|---|---|---|---|---|---|
| Observer 1 | 0.641 | 0.496 | 0.611 | 0.608 | 0.698 |
| Observer 2 | 0.760 | 0.541 | 0.800 | 0.827 | 0.528 |
| Mean | 0.700 | 0.518 | 0.705 | 0.717 | 0.613 |
Table 2
Kappa for interobserver reliability of palmaris longus presence assessment tests
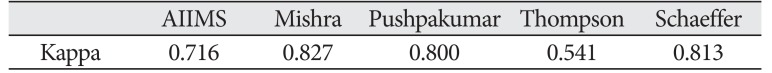
| AIIMS | Mishra | Pushpakumar | Thompson | Schaeffer | |
|---|---|---|---|---|---|
| Kappa | 0.716 | 0.827 | 0.800 | 0.541 | 0.813 |
Table 3
Kappa for agreement of different tests of palmaris longus presence assessment




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download