1. Rees TD. Physical considerations for the aesthetic surgery of the neck and face. In : Rees TD, editor. Aesthetic plastic surgery. Philadelphia: W.B. Saunders;1980. p. 587.
2. Maas CS, Merwin GE, Wilson J, Frey MD, Maves MD. Comparison of biomaterials for facial bone augmentation. Arch Otolaryngol Head Neck Surg. 1990; 116:551–556. PMID:
2158331.

3. Wolfe SA, Berkowitz S. Plastic surgery of the facial skeleton. Boston: Little, Brown;1989. p. 687.
4. Spector M, Harmon SL, Kreutner A. Characteristics of tissue growth into proplast and porous polyethylene implants in bone. J Biomed Mater Res. 1979; 13:677–692. PMID:
479215.

5. Breadon GE, Kern EB, Neel HB 3rd. Autografts of uncrushed and crushed bone and cartilage. Experimental observations and clinical implications. Arch Otolaryngol. 1979; 105:75–80. PMID:
367338.

6. Gosain AK. Plastic Surgery Eductional Foundation DATA Committee. Biomaterials for reconstruction of the cranial vault. Plast Reconstr Surg. 2005; 116:663–666. PMID:
16079708.

7. Wellisz T, Lawrence M, Jazayeri MA, Golshani S, Zhou ZY. The effects of alloplastic implant onlays on bone in the rabbit mandible. Plast Reconstr Surg. 1995; 96:957–963. PMID:
7652071.

8. Gui L, Huang L, Zhang Z. Genioplasty and chin augmentation with Medpore implants: a report of 650 cases. Aesthetic Plast Surg. 2008; 32:220–226. PMID:
18158607.

9. Rubin JP, Yaremchuk MJ. Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 1997; 100:1336–1353. PMID:
9326803.

10. Yaremchuk MJ. Infraorbital rim augmentation. Plast Reconstr Surg. 2001; 107:1585–1592. PMID:
11335841.

11. Shanbhag A, Friedman HI, Augustine J, von Recum AF. Evaluation of porous polyethylene for external ear reconstruction. Ann Plast Surg. 1990; 24:32–39. PMID:
2301880.

12. Frodel JL, Lee S. The use of high-density polyethylene implants in facial deformities. Arch Otolaryngol Head Neck Surg. 1998; 124:1219–1223. PMID:
9821923.

13. Wellisz T, Dougherty W. The role of alloplastic skeletal modification in the reconstruction of facial burns. Ann Plast Surg. 1993; 30:531–536. PMID:
8368781.
14. Romano JJ, Iliff NT, Manson PN. Use of Medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993; 4:142–147. PMID:
8241356.

15. Nélaton C, Ombrédanne L, Berger P, Hartmann H. La rhinoplastie. Paris: G. Steinheil;1904.
16. Joseph J. Treatise on rhinoplasty. Berl Klin Wochenschr. 1907; 44:470.
17. Israel J. Two new methods of rhinoplasty. Plast Reconstr Surg. 1970; 46:80–83. PMID:
4914406.

18. Von Mangold H. Correction of saddle nose by cartilage transplant. Gesell Chir. 1900; 29:460–463.
19. Brown JB, Fryer MP, Randall P, Lu M. Silicones in plastic surgery; laboratory and clinical investigations, a preliminary report. Plast Reconstr Surg (1946). 1953; 12:374–376. PMID:
13111916.
20. Niazi TN, Coppens J, Liu JK, Couldwell WT. Medpor implant in cranioorbitomaxillary reconstruction: institutional experience and a review of the literature. J Oral Maxillofacial Surg. 2008; 7:444–448.
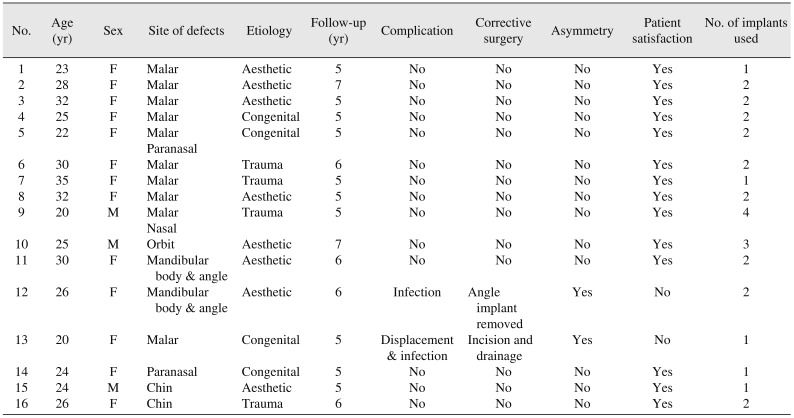
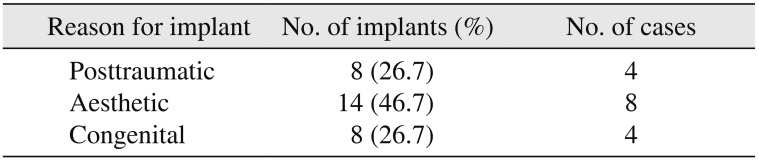
21. Deshpande S, Munoli A. Long-term results of high-density porous polyethylene implants in facial skeletal augmentation: an Indian perspective. Indian J Plast Surg. 2010; 43:34–39. PMID:
20924447.

22. Ram H, Singh RK, Mohammad S, Gupta AK. Efficacy of Iliac crest vs. Medpor in orbital floor reconstruction. J Maxillofac Oral Surg. 2010; 9:134–141. PMID:
22190772.

23. Cenzi R, Guarda-Nardini L. [Use of porous plyethylene (Medpor) in maxillofacial surgery]. Minerva Stomatol. 1995; 44:559–582. Italian. PMID:
8725075.
24. Rubin PA, Bilyk JR, Shore JW. Orbital reconstruction using porous polyethylene sheets. Ophthalmology. 1994; 101:1697–1708. PMID:
7936569.

25. Klawitter JJ, Bagwell JG, Weinstein AM, Sauer BW. An evaluation of bone growth into porous high density polyethylene. J Biomed Mater Res. 1976; 10:311–323. PMID:
1254618.

26. Spector M, Flemming WR, Sauer BW. Early tissue infiltrate in porous polyethylene implants into bone: a scanning electron microscope study. J Biomed Mater Res. 1975; 9:537–542. PMID:
1176523.

27. Kim HS, Park SS, Kim MH, Kim MS, Kim SK, Lee KC. Problems associated with alloplastic materials in rhinoplasty. Yonsei Med J. 2014; 55:1617–1623. PMID:
25323900.

28. Ridwan-Pramana A, Wolff J, Raziei A, Ashton-James CE, Forouzanfar T. Porous polyethylene implants in facial reconstruction: outcome and complications. J Craniomaxillofac Surg. 2015; 43:1330–1334. PMID:
26276064.

29. Niechajev I. Facial reconstruction using porous high-density polyethylene (Medpor): long-term results. Aesthetic Plast Surg. 2012; 36:917–927. PMID:
22684610.

30. Mohammadi S, Mohseni M, Eslami M, Arabzadeh H, Eslami M. Use of porous high-density polyethylene grafts in open rhinoplasty: no infectious complication seen in spreader and dorsal grafts. Head Face Med. 2014; 10:52. PMID:
25534471.

31. Baj A, Spotti S, Marelli S, Beltramini GA, Giannì AB. Use of porous polyethylene for correcting defects of temporal region following transposition of temporalis myofascial flap. Acta Otorhinolaryngol Ital. 2009; 29:265–269. PMID:
20162028.
32. Rapidis AD, Day TA. The use of temporal polyethylene implant after temporalis myofascial flap transposition: clinical and radiographic results from its use in 21 patients. J Oral Maxillofac Surg. 2006; 64:12–22. PMID:
16360852.

33. Xu JJ, Teng L, Jin XL, Ji Y, Lu JJ, Zhang B. Porous polyethylene implants in orbital blow-out fractures and enophthalmos reconstruction. J Craniofac Surg. 2009; 20:918–920. PMID:
19480046.
34. Tsouknidas A, Maropoulos S, Savvakis S, Michailidis N. FEM assisted evaluation of PMMA and Ti6Al4V as materials for cranioplasty resulting mechanical behaviour and the neurocranial protection. Biomed Mater Eng. 2011; 21:139–147. PMID:
22072078.

35. Sun L, Xiao J, Lan Y, Xiong Y, Zhang L, Zhou H, et al. [Reconstruction of the orbital fracture with enophthalmos using customized titanium mesh combined with Medpor]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2015; 33:272–275. Chinese. PMID:
26281256.
36. He D, Li Z, Shi W, Sun Y, Zhu H, Lin M, et al. Orbitozygomatic fractures with enophthalmos: analysis of 64 cases treated late. J Oral Maxillofac Surg. 2012; 70:562–576. PMID:
21752509.

37. Yilmaz M, Vayvada H, Aydin E, Menderes A, Atabey A. Repair of fractures of the orbital floor with porous polyethylene implants. Br J Oral Maxillofac Surg. 2007; 45:640–644. PMID:
17681408.

38. Lin IC, Liao SL, Lin LL. Porous polyethylene implants in orbital floor reconstruction. J Formos Med Assoc. 2007; 106:51–57. PMID:
17282971.

39. Cenzi R, Farina A, Zuccarino L, Carinci F. Clinical outcome of 285 Medpor grafts used for craniofacial reconstruction. J Craniofac Surg. 2005; 16:526–530. PMID:
16077294.

40. Yaremchuk MJ. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconstr Surg. 2003; 111:1818–1827. PMID:
12711941.

41. Gosau M, Schiel S, Draenert GF, Ihrler S, Mast G, Ehrenfeld M. [Craniofacial augmentation with porous polyethylene implants (Medpor): first clinical results]. Mund Kiefer Gesichtschir. 2006; 10:178–184. German. PMID:
16685567.
42. Menderes A, Baytekin C, Topcu A, Yilmaz M, Barutcu A. Craniofacial reconstruction with high-density porous polyethylene implants. J Craniofac Surg. 2004; 15:719–724. PMID:
15346006.

43. Romo T 3rd, Litner JA, Sclafani AP. Management of the severe bulbous nasal tip using porous polyethylene alloimplants. Facial Plast Surg. 2003; 19:341–348. PMID:
14737703.

44. Emsen IM. E-M shaped septal encircling with Medpor reconstruction on crooked noses: personal technique and postoperative results. J Craniofac Surg. 2008; 19:216–226. PMID:
18216692.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download