Abstract
Objectives
Temporomandibular joint ankylosis (TMJA) is a joint pathology caused by bony and/or fibrous adhesion of the joint apparatus, resulting in partial or total loss of function.
Materials and Methods
This is a retrospective study conducted between 2012 and 2016 in the northwest region of Nigeria. The data retrieved includes gender, age, etiology of ankylosis, duration of ankylosis, laterality of ankylosis, type of imaging technique, type of airway management, types of incision, surgical procedure, mouth opening, interpositional materials used, and complications. Results were presented as simple frequencies and descriptive statistics.
Results
Thirty-six patients with TMJA were evaluated during the study period. There were 21 males (58.3%) and 15 females (41.7%), yielding a male:female ratio of 1.4:1. The patients' age ranged from 5 to 33 years with mean±standard deviation (13.8±6.6 years). Thirty-five cases (97.2%) were determined to be true/bony ankylosis, while only 1 case (2.8%) was false/fibrous ankylosis. Most of the TMJA cases (16 cases, 44.4%) were secondary to a fall. In our series, the most commonly utilized incision was the Bramley-Al-Kayat (15 cases, 41.7%). The mostly commonly performed procedures were condylectomies and upper ramus ostectomies (12 cases each, 33.3%), while the most commonly used interpositional material was temporalis fascia (14 cases, 38.9%). The complications that developed included 4 cases (11.1%) of severe hemorrhage, 1 case (2.8%) of facial nerve palsy, and 1 case (2.8%) of re-ankylosis.
Temporomandibular joint ankylosis (TMJA) is a joint pathology caused by bony and/or fibrous adhesion of the joint apparatus, resulting in partial or total loss of function12. Since the temporomandibular joint (TMJ) is unique in that it requires the synchronous motion of two joints for function, any pathology in one or both joints results in functional problems that can lead to low self-esteem and poor quality of life. The aetio-pathogenesis of TMJA includes trauma (e.g., forceps delivery)3, fall on the chin45, middle ear infection, and cancrum oris. Recent reports have established a progressive ankylosis gene that controls osteoblast differentiation6.
Several classifications of TMJA have been proposed to determine the difficulty of surgical treatment7. Currently, TMJA is classified simply as true or false ankylosis. Sawhney8 further classified true ankylosis into types I, II, III, and IV. The management of TMJA poses a great challenge due to technical difficulties in investigating and treating the disease, as well as the high incidence of recurrence9. Several techniques have been reported in literature; however, no single method has produced a uniform success rate21011. Such technical difficulties are further aggravated in resource- and personnel-scarce countries. Healthcare funding in sub- Saharan Africa, especially Nigeria, has often been described as grossly inadequate, with the budgetary provision to health hardly exceeding 3% of the nation's total1213. These issues are further compounded by the out-of-pocket payment system with inadequate health insurance coverage12.
The main aim of this study, therefore, is to present an audit of TMJA management in a resource-scarce population.
This is a retrospective study conducted from 2012 to 2016 at two tertiary referral centers (Usmanu Danfodiyo University Teaching Hospital, Sokoto; Sokoto State and National Orthopaedic Hospital Dalla, Kano, Kano State) in the northwest region of Nigeria. The data collected includes gender, age, etiology of ankylosis, duration of ankylosis, laterality of ankylosis, type of imaging technique, type of airway management, types of incision, surgical procedure, mouth opening, interpositional materials used, and complications. Ethical approval was obtained from the ethics and research committee of Usmanu Danfodiyo University Teaching Hospital (UDUTH/HREC/2017/No. 590).
The data was analyzed using IBM SPSS Statistics for Windows (ver. 20.0; IBM Co., Armonk, NY, USA). Results were presented as simple frequencies and descriptive statistics. Tests of significance were used as appropriate, and a P-value of less than 0.05 was considered significant.
Thirty-six patients with TMJA were examined during the study period. There were 21 males (58.3%) and 15 females (41.7%), resulting in a male:female ratio of 1.4:1. Patients' age ranged from 5 to 33 years, yielding a mean±standard deviation (SD) of 13.8±6.6 years. The duration of TMJA ranged from 1 to 28 years (mean±SD, 8.9±5.9 years). There was no significant difference associated with age and gender.(Table 1) Thirty-five cases (97.2%) were classified as true/bony ankylosis, while only 1 case (2.8%) was false/fibrous ankylosis. In most cases, TMJA was secondary to a fall (16 cases, 44.4%), or road traffic accidents and cancrum oris, which made up 7 cases (19.4%) each. Only 6 cases (16.7%) were caused by middle ear infection.(Table 2) There were 22 cases (61.1%) of bilateral TMJA.(Table 2) All cases of ankylosis with maxillary extension were secondary to cancrum oris, with a statistically significant difference of P=0.001. Seventy-five percent of the patients had plain radiographs, while only 25% had undergone computed tomography (CT).(Fig. 1) Eighteen patients (50.0%) underwent tracheostomy, 17 patients (47.2%) had fiber optic intubation, and only one patient (2.8%) had blind nasal intubation. The Bramley-Al-Kayat incision (Fig. 2. A) was the most used in our series (15 cases, 41.7%).(Table 3) A post-ramus incision (Fig. 2. B) was carried out in 9 patients (25.0%), while 7 patients (19.4%) underwent pre-auricular incision.(Table 3)
The most common procedures performed in our series were condylectomies and upper ramus ostectomies (12 each; 33.3%), while the temporalis fascia (14 cases, 38.9%; Fig. 2. C) and masseter (11 cases, 30.6%; Fig. 2. D) were the most favored interpositional material used, with a significant difference of P=0.001.(Table 4) The maximum and minimum intraoperative mouth openings achieved were 5 cm and 3.2 cm, respectively (mean±SD, 4.01±0.54 cm). There was no significant difference when comparing degree of intraoperative mouth opening with type of procedure (P=0.333).(Table 5)
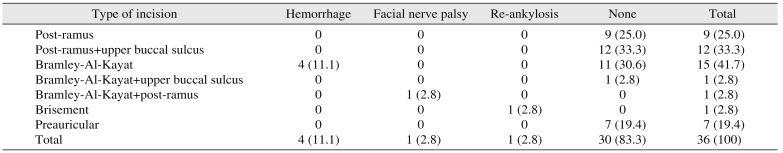
Complications encountered include severe hemorrhage in 4 cases (11.1%), facial nerve palsy in 1 case (2.8%), and reankylosis in 1 case (2.8%).(Table 6) When comparing complications encountered with the type of procedure, there was a significant difference (χ2=45.28, degree of freedom=15, P=0.000).(Table 6) Follow-up examinations occurred for all patients for a minimum of 10 months. Table 7 showed complications encountered with different types of incision done to expose the ankylotic site.
If it is not treated early, TMJA is the most common cause of acquired mandibular deformity in both children and adults14. The main objectives of ankylosis treatment are to achieve maximum mouth opening and optimal joint mobility, avoid inflammation and pain, and restore the initial occlusion in order to obtain facial symmetry15. Successful treatment of TMJA requires detailed preoperative assessment of the type and degree of deformity16. The most common etiopathogeneses of TMJA have previously been reported to be preceding trauma (road traffic accidents and falls), closely followed by infection171819. In the present study, most TMJA cases were caused by preceding trauma (23 cases, 63.9%) or infection (middle ear infection and cancrum oris; 13 cases, 36.1%).
CT has been reported as the most important imaging technique for accurate surgical management of TMJA2021. Unfortunately, this mode of investigation is inadequate in resource-scarce countries, and, where available, it is out of the financial reach of a majority of citizens due to out-of-pocket payment systems in healthcare delivery. Most of our patients (75%) could only afford plain radiographs; only 25% could afford CT. Conventional radiographs have been reported to misjudge the extent of bony ankylosis that is discovered during surgery22. However, Posnick and Goldstein23 have reported that CT scans provide some added information to plain radiographs. The authors of this study differ on this position because, in our series, the extent of ankylotic mass was discovered during surgery. Imaging is not beneficial in the case of fibrous ankylosis because only osseous ankylosis presents on radiographs24. Therefore, fibrous ankylosis is more of a clinical diagnosis than a radiographic one24. We found only 1 case (2.8%) of fibrous ankylosis in our series, and, corresponding with literature, plain radiographs were unable to characterize it.
TMJA can negatively affect a growing child, as shortening of mandibular rami can narrow airways and reduce space between the mandibular angles25. These structural abnormalities, combined with a limited or no mouth opening, cause difficulties in securing the airway25. A tracheotomy was necessary in half of the cases in our series (18 cases, 50.0%). Several techniques have been described for airway management in TMJA, including blind or fiber optic guided awake nasal intubation, retrograde intubation, and tracheostomy2526. Tracheostomy is generally regarded as a last option because of the severe morbidity, long-term side effects, and high mortality rates associated with the procedure; however, with limited options for fiber optics, this method has been our primary choice for airway management. Previous reports have indicated that the complications associated with tracheostomy can be minimized by early decannulation in the immediate postoperative stage, usually within 24 hours27.
The type of surgical incision used to expose the ankylotic mass is largely determined by the extent of ankylosis. The Bramley-Al-Kayat incision was used when the ankylotic mass was limited to the joint space and condylar head (15 cases, 41.7%). This incision type has been reported to provide outstanding visibility due to a larger flap while maintaining an intact temporal fascia that is not reflected with the incision28. Additional benefits of the Bramley-Al-Kayat incision include: reduced likelihood of sensory damage28, simplicity of administration, proximity to the temporal joint, and successful functional and clinical results2930. A post-ramus incision was utilized for easy access when the ankylotic mass extended into the ramus.(Fig. 2. B) This approach into the ankylotic mass has been reported in literature27. An intraoral incision was employed to expose the ankylotic mass when the ankylotic mass involved the maxilla.
The surgical technique used to release the ankylotic mass following TMJA is termed gap arthroplasty, in which an interpositioning material is applied to prevent re-ankylosis. Other techniques, like total joint replacement using costo-chondria grafts from the ribs, have also been reported31. First reported in 1880 by Abbe32, gap arthroplasty involves the removal of a block of bone, leaving a gap between the ascending ramus and temporal bone. Ramus and condylar ostectomies (Fig. 3. A) were the most frequently conducted procedures in our study (24 cases, 66.7%). The maximal inter-incisal distance achieved intraoperatively following gap arthroplasty was 5 cm.(Fig. 3. B) This maximum was observed frequently in the ramus procedures in the current study, though the frequency was not statistically significant. Several techniques have been developed to prevent re-ankylosis, which is the greatest concern following TMJA release. Using the autogenous temporalis muscle as a myofascial flap has gained acceptance due to its proximity to the surgical site. In our series, when the Bramley-Al-Kayat incision was employed, we used the temporalis fascia or temporalis muscle as the interpositional material. Similarly, when using the post-ramus incision, we chose the masseter muscle as the interpositional material. While the temporalis muscle has been favored as the interpositional material in preventing re-ankylosis, it has been reported to fail due to postoperative contraction of the muscle. Balaji30 addressed this issue by anchoring the temporalis muscle flap to the submandibular region in order to inhibit the aforementioned postoperative muscle contraction. Other graft materials include the masseter muscle, fascia lata, and auricular cartilage33. Silastic, Proplast-Teflon, and metallic fossa implants and acrylic marbles have also been used as alloplastic interpositional materials; however, use of these materials is fraught with high failure rates10. No alloplastic material was used in our series.
The oldest method of managing fibrous ankylosis involves the application of brisement force using instruments to force the mouth open while the patient is under local or general anesthesia. The only patient with fibrous ankylosis in our series was treated in this manner.
Massive intraoperative hemorrhaging was observed as a complication in 4 patients (11.1%) who underwent condylar and coronoid ostectomies (2 each, 5.6%). We reason that, because most of our patients could not afford CT, using plain radiographs limited the extent of preoperative assessment. Furthermore, Metwalli34 have reported that the distances between the internal carotid artery, the internal jugular vein, the maxillary artery, and the medial pole of the mandibular condyle were reduced in TMJA patients when compared to patients without ankylosis. The severe hemorrhaging was managed by blocking the bridged sigmoid sinus with bone wax and a pressure pack. The use of bone wax in controlling osseous bleeding has been documented in literature35. However, this process is fraught with complications like delayed bone healing36, surgical site infection, and osteomyelitis37. In our case, however, these complications were not observed. The pressure pack was removed 5 days after the operation. The patient, who was suffering from facial nerve palsy, was prescribed and administered vitamin B complex followed by physical therapy of the facial muscles. The patient's condition improved with time as injury to the facial nerve was neuropraxia38. Temporal loss of motor function of a nerve due to blockage of nerve conduction from compression of the nerve by bruising of the nerve or by inflammatory edema. A bilateral condylectomy was planned for the patient with reankylosis, but the patient did not report back to the hospital. During the follow-up period, almost all patients (35 patients, 97.2%) did not have a reduced mouth opening compared to the intraoperative measurement. We attribute this to the strict instructions they received on the importance of jaw physiotherapy for at least 6 months. Only 1 case (2.8%) of reankylosis was observed in our series, and it occurred in the patient with fibrous ankylosis. This patient is a young boy in secondary school who is living in the school student house with no supervision on jaw physiotherapy, which may have led to re-ankylosis. The patient's compliance to aggressive physiotherapy is essential to prevent re-ankylosis in the case of either bony or fibrous ankylosis.
Although CT is the standard investigative procedure for TMJA, plain radiographs, with their shortcomings, have a significant role in resource-scarce environments. Interpositional gap arthroplasty using a temporalis fascia/muscle flap is a viable treatment choice in managing TMJA due to its excellent vascular supply and association with minimal complications and morbidity. Anchoring the flap to the submandibular region is encouraged. Furthermore, aggressive postoperative physiotherapy for a sufficient period of time (minimum of 6 months) is paramount.
Acknowledgements
The authors are grateful to the Health Records Departments of Usmanu Danfodiyo University Teaching Hospital, Sokoto, Sokoto State and National Orthopaedic Hospital Dalla, Kano, Kano State for the retrieval of case notes.
Notes
Ethics Approval and Consent to Participate: Ethical approval was obtained from the ethics and research committee of Usmanu Danfodiyo University Teaching Hospital (UDUTH/HREC/2017/No. 590).
References
1. Erol B, Tanrikulu R, Görgün B. A clinical study on ankylosis of the temporomandibular joint. J Craniomaxillofac Surg. 2006; 34:100–106. PMID: 16423530.

2. Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:166–169. PMID: 10052370.
3. Obiechina AE, Arotiba JT, Fasola AO. Ankylosis of the temporomandibular joint as a complication of forceps delivery: report of a case. West Afr J Med. 1999; 18:144–146. PMID: 10504875.
4. Güven O, Keskin A. Remodelling following condylar fractures in children. J Craniomaxillofac Surg. 2001; 29:232–237. PMID: 11562093.

5. Singh V, Sudhakar KNV, Mallela KK, Mohanty R. A review of temporomandibular joint-related papers published between 2014-2015. J Korean Assoc Oral Maxillofac Surg. 2017; 43:368–372. PMID: 29333366.

6. Pilmane M, Skagers A. Growth factors, genes, bone proteins and apoptosis in the temporomandibular joint (TMJ) of children with ankylosis and during disease recurrence. Stomatologija. 2011; 13:96–101. PMID: 22071418.
8. Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986; 77:29–40. PMID: 3941847.
9. Vasconcelos BC, Porto GG, Bessa-Nogueira RV, Nascimento MM. Surgical treatment of temporomandibular joint ankylosis: follow-up of 15 cases and literature review. Med Oral Patol Oral Cir Bucal. 2009; 14:E34–E38. PMID: 19114954.

10. Erdem E, Alkan A. The use of acrylic marbles for interposition arthroplasty in the treatment of temporomandibular joint ankylosis: follow-up of 47 cases. Int J Oral Maxillofac Surg. 2001; 30:32–36. PMID: 11289618.

11. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990; 48:1145–1151. PMID: 2213309.

12. Orubuloye IO, Oni JB. Health transition research in Nigeria in the era of the Structural Adjustment Programme. Health Transit Rev. 1996; (6 Suppl):6:301–324. PMID: 10165307.
14. Singh V, Mohammad S, Singh G. Management of TMJ ankylosis and post ankylotic deformities a simultaneous procedure. J Maxillofac Oral Surg. 2005; 5:17–19.
15. Miranda HB, Miranda VJE. Temporomandibular joint ankylosis treated with arthroplasty in a patient with reumathoid arthritis. Rev Odont Mex. 2011; 15:164–169.
16. Kao SY, Chou J, Lo J, Yang J, Chou AP, Joe CJ, et al. Using three-dimensional-computerized tomography as a diagnostic tool for temporo-mandibular joint ankylosis: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1999; 62:244–249. PMID: 10367487.
17. Loveless TP, Bjornland T, Dodson TB, Keith DA. Efficacy of temporomandibular joint ankylosis surgical treatment. J Oral Maxillofac Surg. 2010; 68:1276–1282. PMID: 20304543.

18. Zhi K, Ren W, Zhou H, Gao L, Zhao L, Hou C, et al. Management of temporomandibular joint ankylosis: 11 years' clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:687–692. PMID: 19782622.

19. Elgazzar RF, Abdelhady AI, Saad KA, Elshaal MA, Hussain MM, Abdelal SE, et al. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. 2010; 39:333–342. PMID: 20149597.

20. de Bont LG, van der Kuijl B, Stegenga B, Vencken LM, Boering G. Computed tomography in differential diagnosis of temporomandibular joint disorders. Int J Oral Maxillofac Surg. 1993; 22:200–209. PMID: 8409559.

21. El-Hakim IE, Metwalli SA. Imaging of temporomandibular joint ankylosis. A new radiographic classification. Dentomaxillofac Radiol. 2002; 31:19–23. PMID: 11803384.

22. Sanders R, MacEwen CJ, McCulloch AS. The value of skull radiography in ophthalmology. Acta Radiol. 1994; 35:429–433. PMID: 8086247.

23. Posnick JC, Goldstein JA. Surgical management of temporomandibular joint ankylosis in the pediatric population. Plast Reconstr Surg. 1993; 91:791–798. PMID: 8460181.

24. Joshi UM, Patil SG, Shah K, Allurkar S. Brisement force in fibrous ankylosis: a technique revisited. Indian J Dent Res. 2016; 27:661–663. PMID: 28169267.
25. Kulkarni J, Shah K, Ahadghaffarkhan A, Khaire S. Anaesthetic management of temporomandibular joint ankylosis without fibrotic bronchoscope: a review of 31 cases. J Dent Med Sci. 2013; 8:50–54.
26. Shah FR, Sharma KR, Hilloowalla RN, Karandikar AD. Anaesthetic considerations of temporomandibular joint ankylosis with obstructive sleep apnoea: a case report. J Indian Soc Pedod Prev Dent. 2002; 20:16–20. PMID: 12435028.
27. Braimah RO, Oladejo T, Olarinoye TO, Adetoye AO, Osho PO. A multidisciplinary approach to the management of temporomandibular joint ankylosis in a sickle-cell anemia patient in a resource-limited setting. Ann Maxillofac Surg. 2016; 6:130–134. PMID: 27563622.

28. Ellis E, Zide MF. Approaches to the temporomandibular joint. In : Ellis E, Zide MF, editors. Surgical approaches to the facial skeleton. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 191–212.
29. Clauser L, Curioni C, Spanio S. The use of the temporalis muscle flap in facial and craniofacial reconstructive surgery. A review of 182 cases. J Craniomaxillofac Surg. 1995; 23:203–214. PMID: 7560105.

30. Balaji SM. Modified temporalis anchorage in craniomandibular reankylosis. Int J Oral Maxillofac Surg. 2003; 32:480–485. PMID: 14759105.

31. Mohan CM, Prasad BR, Bhat S, Bhat SS. Reconstruction of condyle following surgical correction of temporomandibular joint ankylosis: current concepts and considerations for the future. Nitte Univ J Health Sci. 2014; 4:39–46.
32. Abbe R. An operation for the relief of ankylosis of the temporomaxillary joint, by exsection of the neck of the condyle of the lower jaw; with remarks. New York Med J. 1880; 31:362–366.
33. Feinberg SE, Larsen PE. The use of a pedicled temporalis musclepericranial flap for replacement of the TMJ disc: preliminary report. J Oral Maxillofac Surg. 1989; 47:142–146. PMID: 2913247.

34. Metwalli S. Computerized tomography of the temporal bone in TMJ ankylosis. Cairo: Cairo University;1993.
35. Wellisz T, Armstrong JK, Cambridge J, Fisher TC. Ostene, a new water-soluble bone hemostasis agent. J Craniofac Surg. 2006; 17:420–425. PMID: 16770175.

36. Wellisz T, Armstrong JK, Cambridge J, An YH, Wen X, Kang Q, et al. The effects of a soluble polymer and bone wax on sternal healing in an animal model. Ann Thorac Surg. 2008; 85:1776–1780. PMID: 18442583.

37. Wellisz T, An YH, Wen X, Kang Q, Hill CM, Armstrong JK. Infection rates and healing using bone wax and a soluble polymer material. Clin Orthop Relat Res. 2008; 466:481–486. PMID: 18196435.

38. Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008; 119:1951–1965. PMID: 18482862.

Fig. 1
A. Three-dimensional (3D) computed tomography (CT) view of right temporomandibular joint ankylosis (TMJA). B. 3D CT view of left TMJA. C. CT coronal view showing right TMJA.
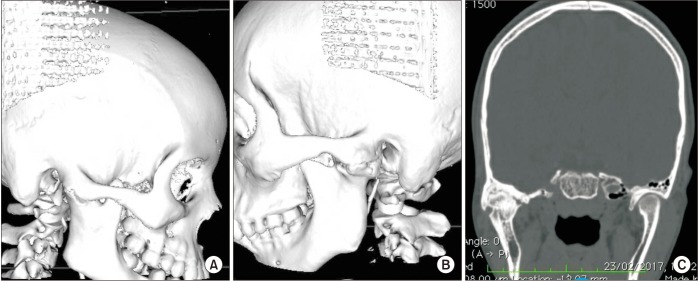
Fig. 2
A. Bramley-Al-Kayat incision for access to temporomandibular joint ankylosis (TMJA). B. Post-rami incision in gap arthroplasty for access to TMJA. C. Temporalis muscle/fascia for gap arthroplasty. D. Masseter muscle for gap arthroplasty.
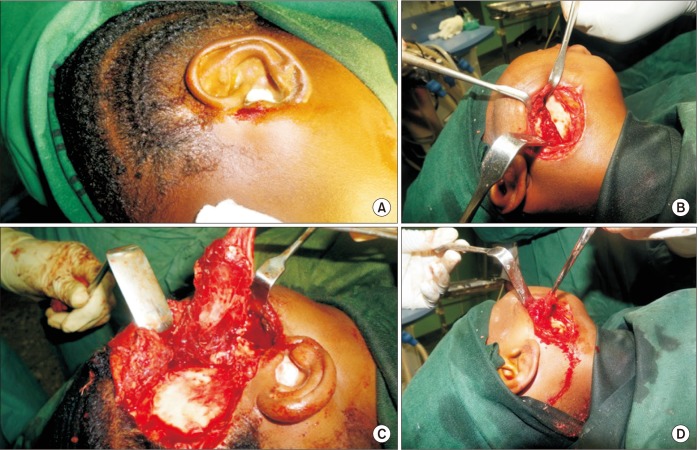
Fig. 3
A. Ramus ostectomy for release of temporomandibular joint ankyloses (TMJA). B. Intraoperative inter-incisal distance achieved in TMJA.
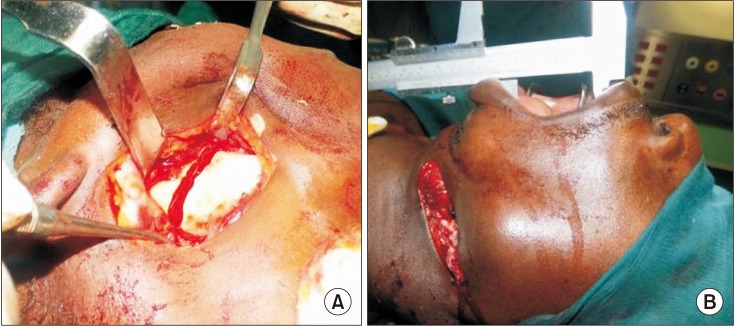
Table 1
Age and gender distribution of patients with temporomandibular joint ankylosis
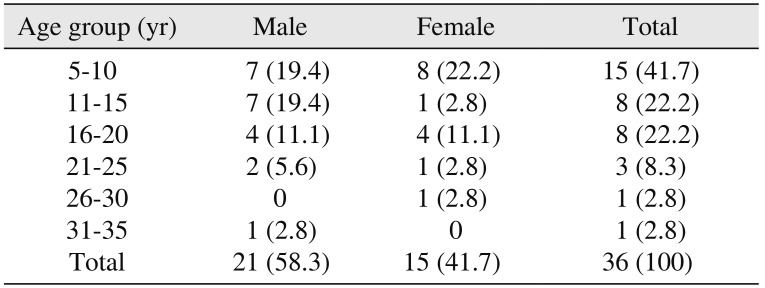
Table 2
Distribution of site and etiology of temporomandibular joint ankylosis
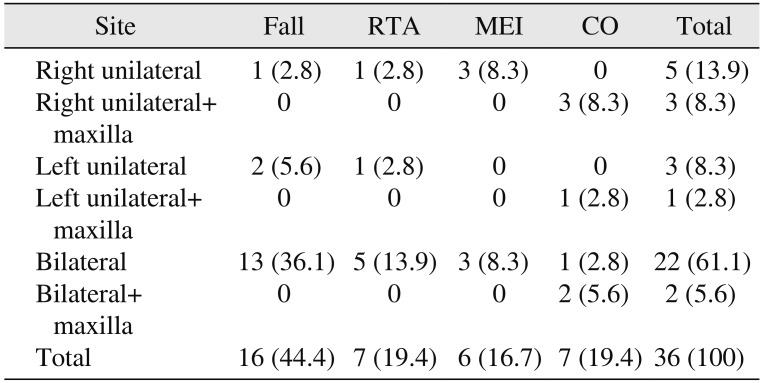
Table 3
Distribution of types of incisions used to access the ankylotic mass
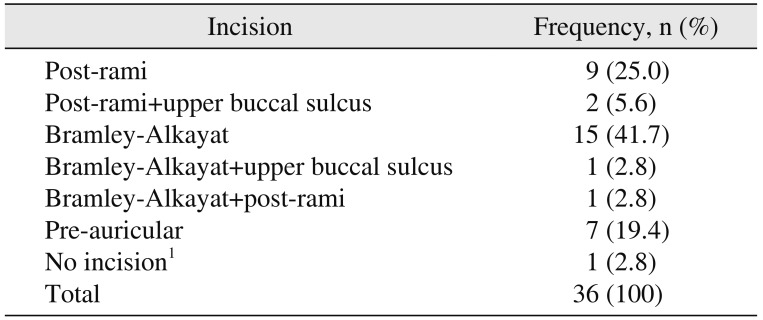
Table 4
Distribution of procedure conducted and interpositional material utilized
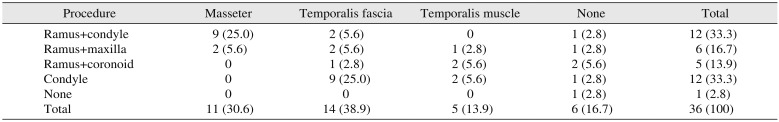
Table 5
Distribution of degree of intraoperative mouth opening and type of procedure
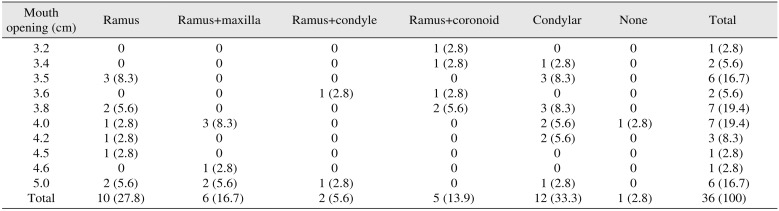
Table 6
Distribution of procedure conducted and complications
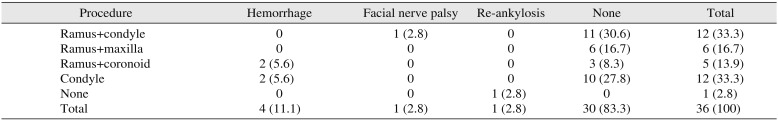
Table 7
Distribution of type of incision and complications




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download