Abstract
Purpose
There have only been a few studies on optimal usage of injection material in the regional nerve block for lower extremity operations. The purpose of this study was to evaluate the efficacy of different concentrations of ropivacaine.
Materials and Methods
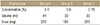
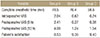
A total of 339 patients underwent lower extremity surgery under ultrasound-guided nerve block (combined femoral and sciatic nerve block) at a Chungnam National University Hospital between March 2016 and February 2017 and were randomly assigned to three groups: Group A (0.5%, 44 ml), group B (0.6%, 30 ml), and group C (0.75%, 30 ml). The interval between nerve block procedure and onset of the complete anesthetic effect (complete anesthetic time) was investigated. The degrees of intraoperative pain, and postoperative pain were evaluated using a visual analogue scale (VAS) score. Patient's satisfaction (0–10) was investigated. To evaluate the efficacy in accordance with the concentration under the same dose and same volume, group A and B were compared with group C respectively.
Results
There were 108, 118, and 113, in groups A, B, and C, respectively; and there were no significant differences with respect to the number, age, sex, and type of operation (p>0.05). The mean complete anesthetic times were 78.5, 76.4, and 58.6 minutes, respectively. The mean intraoperative VAS scores were 2.04, 0.62, and 0.24; and the mean postoperative VAS scores (6 hours/12 hours) were 2.41/4.08, 0.27/1.24, and 0.38/1.54. The mean patient's satisfactory scores were 8.53, 9.38, and 9.40, respectively. Compared with group C, group A showed significantly longer complete anesthetic time (p<0.05) and higher intra, postoperative VAS scores (all p<0.05). Group B showed longer complete anesthetic time (p<0.05), but no significant difference of intra, postoperative VAS scores (all p>0.05). Patient's satisfactory scores in both group A and B were similar to group C (p>0.05, p>0.05). There were no specific adverse reactions in all groups.
Figures and Tables
 | Figure 1Ultrasound-guided femoral nerve block procedure. (A) Gross photograph shows ultrasound probe and spinal needle position for the right femoral nerve block with the patient positioned supine. (B) It is an ultrasound image on the right femoral triangle area (level of Fig. 1A image). (C) Ultrasound image shows the anesthetic and spinal needle around the right femoral nerve during injection. |
 | Figure 2Ultrasound-guided sciatic nerve block procedure. (A) Gross photograph shows ultrasound probe and spinal needle position for the right sciatic nerve block with patient's hip flexed in supine position. The probe is located on the posterior thigh. (B) Ultrasound image shows sciatic nerve and spinal needle more proximally than the popliteal crease level (level of Fig. 2A image). (C) Ultrasound image shows that anesthetic surrounds the right sciatic nerve after injection. |
 | Figure 3Comparison of the mean complete anesthetic time, patient's satisfaction, and VAS score in groups A and C. (A) Compared with group C, group A shows a significantly longer complete anesthetic time. (B) Group A shows a statistically similar patient's satisfaction to group C. (C) Compared with group C, group A shows significantly higher intra, postoperative (6 h/12 h) VAS scores. VAS, visual analogue scale; I, intraoperative; P6, postoperative 6 hours; P12, postoperative 12 hours. |
 | Figure 4Comparison of mean complete anesthetic time, patient's satisfaction, and VAS score in groups B and C. (A) Compared with group C, group B shows a significantly longer complete anesthetic time. (B) Group B shows a statistically similar patient's satisfaction to group C. (C) Group B shows similar intraoperative, postoperative (6 h/12 h) VAS scores statistically. VAS, visual analogue scale; I, intraoperative; P6, postoperative 6 hours; P12, postoperative 12 hours. |
References
1. Kang C, Hwang DS, Kim YM, et al. Ultrasound-guided femorosciatic nerve block by orthopaedist for ankle fracture operation. J Korean Foot Ankle Soc. 2010; 14:90–96.
2. Kang C. Ultrasound-guided regional nerve block in lower extremity. J Korean Orthop US Soc. 2012; 1:50–59.
3. Mohan V. TKR under combined femoral and sciatic nerve blocks. Kerala J Orthop. 2015; 27:104–106.
4. Klein SM, Greengrass RA, Steele SM, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998; 87:1316–1319.

6. McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs. 2000; 60:1065–1093.
7. Zhai W, Wang X, Rong Y, Li M, Wang H. Effects of a fixed low-dose ropivacaine with different volume and concentrations on interscalene brachial plexus block: a randomized controlled trial. BMC Anesthesiol. 2016; 16:80.

8. Su Y, Zhang Z, Zhang Y, Li H, Shi W. Efficacy of ropivacaine by the concentration of 0.25%, 0.5%, and 0.75% on surgical performance, postoperative analgesia, and patient's satisfaction in inguinal hernioplasty: a randomized controlled trial. Patient Prefer Adherence. 2015; 9:1375–1379.
9. Fredrickson MJ, Abeysekera A, White R. Randomized study of the effect of local anesthetic volume and concentration on the duration of peripheral nerve blockade. Reg Anesth Pain Med. 2012; 37:495–501.

10. Marhofer P, Eichenberger U, Stöckli S, et al. Ultrasonographic guided axillary plexus blocks with low volumes of local anaesthetics: a crossover volunteer study. Anaesthesia. 2010; 65:266–271.

11. O'Donnell B, Riordan J, Ahmad I, Iohom G. Brief reports: a clinical evaluation of block characteristics using one milliliter 2% lidocaine in ultrasound-guided axillary brachial plexus block. Anesth Analg. 2010; 111:808–810.
12. Wank W, Büttner J, Maier KR, Emanuelson BM, Selander D. Pharmacokinetics and efficacy of 40 ml ropivacaine 7.5 mg/ml (300 mg), for axillary brachial plexus block--an open pilot study. Eur J Drug Metab Pharmacokinet. 2002; 27:53–59.
13. Baddoo H. A preliminary report on the use of peripheral nerve blocks for lower limb amputations. Ghana Med J. 2009; 43:24–28.
14. Denny NM, Harrop-Griffiths W. Editorial I: Location, location, location! Ultrasound imaging in regional anaesthesia. Br J Anaesth. 2005; 94:1–3.

15. O'Donnell BD, Szűcs S. Peripheral nerve block and local anaesthetic dose, how much is enough? Anaesthesia. 2014; 69:665–668.
16. Nader A, Kendall MC, De Oliveira GS, et al. A dose-ranging study of 0.5% bupivacaine or ropivacaine on the success and duration of the ultrasound-guided, nerve-stimulator-assisted sciatic nerve block: a double-blind, randomized clinical trial. Reg Anesth Pain Med. 2013; 38:492–502.
17. Markham A, Faulds D. Ropivacaine. A review of its pharmacology and therapeutic use in regional anaesthesia. Drugs. 1996; 52:429–449.
18. Krenn H, Deusch E, Balogh B, et al. Increasing the injection volume by dilution improves the onset of motor blockade, but not sensory blockade of ropivacaine for brachial plexus block. Eur J Anaesthesiol. 2003; 20:21–25.

19. Kimura Y, Kamada Y, Kimura A, Orimo K. Ropivacaine-induced toxicity with overdose suspected after axillary brachial plexus block. J Anesth. 2007; 21:413–416.

20. Satsumae T, Tanaka M, Saito S, Inomata S. Convulsions after ropivacaine 300 mg for brachial plexus block. Br J Anaesth. 2008; 101:860–862.

21. Wong AK, Keeney LG, Chen L, Williams R, Liu J, Elkassabany NM. Effect of local anesthetic concentration (0.2% vs 0.1% ropivacaine) on pulmonary function, and analgesia after ultrasound-guided interscalene brachial plexus block: a randomized controlled study. Pain Med. 2016; 17:2397–2403.

22. Schoenmakers KP, Fenten MG, Louwerens JW, Scheffer GJ, Stienstra R. The effects of adding epinephrine to ropivacaine for popliteal nerve block on the duration of postoperative analgesia: a randomized controlled trial. BMC Anesthesiol. 2015; 15:100.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download