INTRODUCTION
Ampullary cancer could develop from adenomas by adenomacarcinoma progression similar to the development of colorectal cancer [
1]. Therefore, both benign and malignant ampullary tumors should be resected completely [
23].
Although endoscopic papillectomy (EP) is a simple procedure and globally recognized as the first choice for treatment of benign ampullary tumors, it can only be applied to small tumors confined at the papilla, without involvement of the common bile duct (CBD) or pancreatic duct (P-duct) [
45]. If EP is not successful or the ampullary tumor recurs, a surgical approach needs to be considered.
Pancreaticoduodenectomy (PD) is the standard surgical treatment approach for ampullary tumors, especially malignant tumors [
236]. However, although the postoperative mortality and morbidity associated with PD have decreased, they remain high. In addition, several reports have been published regarding the development of diabetes mellitus (DM) after PD. The quality of life after surgery should be considered in patients with benign and low-grade tumors.
Transduodenal ampullectomy (TDA) was first introduced by Halsted in 1899, but the use of this procedure remains controversial, and has failed to be widespread because the surgical technique had not been standardized, along with apprehension for the possibility of recurrence [
78]. TDA has been reported in limited cases and in a small number of series.
However, several reports have indicated that TDA can be used as an alternative treatment approach for large ampullary tumors not indicated for EP, and poor surgical candidates for PD [
7910].
The aim of this study was to analyze perioperative and long-term clinical outcomes of patients with ampullary tumors who underwent TDA in a single large-volume center.
Go to :

METHODS
Patients and perioperative outcomes
A retrospective review of data from 2004 to 2016 revealed 26 patients who underwent TDA at Asan Meidical Center. Patients' demographic characteristics, preoperative- or postoperative endoscopic interventions, operative procedures, postoperative morbidity and mortality, hospitalization, and follow-up time were analyzed. All surgery-related morbidities were evaluated. Postoperative surgical complications were described in accordance with the classification proposed by Dindo et al. [
11]. Postoperative mortality was defined as in-hospital or 90-day death. The T stage of the ampulla of Vater cancer was staged according to the seventh edition of the American Joint Committee on Cancer system.
Indication for TDA at our institution
TDA is indicated for the following patients:
(1) Those determined not to be suitable for EP by a gastroenterologist owing to the presence of high-grade dysplasia (HGD) with CBD or p-duct invasion on endoscopic ultrasonography (EUS), large size, or flat lesion.
(2) Those with recurrent adenoma after EP.
(3) Those who have incomplete resection (positive resection margin) after EP.
(4) Those with malignancy but poor general condition for PD.
Preoperative work-up
Magnetic resonance imaging cholangiopancreatography, contrast-enhanced computed tomography, endoscopy, and EUS were used for examining the patients, as required. Preoperative endoscopic biopsy is also routinely performed.
Surgical procedure for TDA
No significant difference in indication was found between open and laparoscopic TDA. Surgeons have preference regarding operation methods. All patients received full explanation about both the strengths and weaknesses of open and laparoscopic TDA, and decided with the guidance of the surgeon which operation will be performed.
Open-TDA
Under general anesthesia, the patient was laid in the supine position. We usually used a midline or reversed- L-incision for the open approach. We performed adequate kocherization of the duodenum, followed by identification of the ampullary lesion by palpation of the second part of the duodenum. A lateral duodenotomy incision (3 cm) was then made at the site overlying the palpated lesion longitudinally along the long axis of the duodenum. Stay sutures at corners of the incision were then applied to keep the duodenotomy open. Submucose infiltration around the lesion was performed with a syringe, by filling it with saline with or without adrenaline, to elevate the lesion off the submucosa. The lesion was excised using monopolar cautery, and both ducts were excised under direct vision.
The specimen was extracted. We routinely performed intraoperative frozen biopsy during TDA. The specimen was sent to a pathologist together with the tumor orientation details. Examination of the frozen section (FS) revealed the bile duct and pancreatic duct, and 4 lateral margins (3, 6, 9, and 12 o'clock) without any tumor involvement.
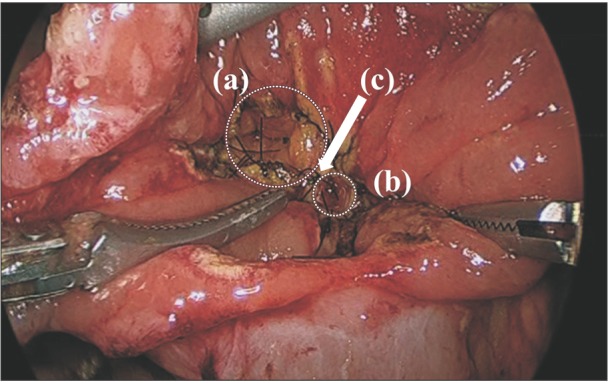
Stay sutures on the pancreatic duct and the CBD for making a common channel were then applied. The adjacent walls of the pancreatic duct and CBD were sutured with 5/0 PDS (Ethicon US, LLC, Cincinnati, OH, USA) to reconstruct the common channel of the ampulla. Single-layer duct-to-mucosa choledochoduodenostomy and pancreaticoduodenostomy were performed with 5/0 PDS (
Fig. 1). The duodenotomy incision was then closed transversely with 1 or 2 layers. After inserting a drain tube, the wounds were closed in the usual manner.
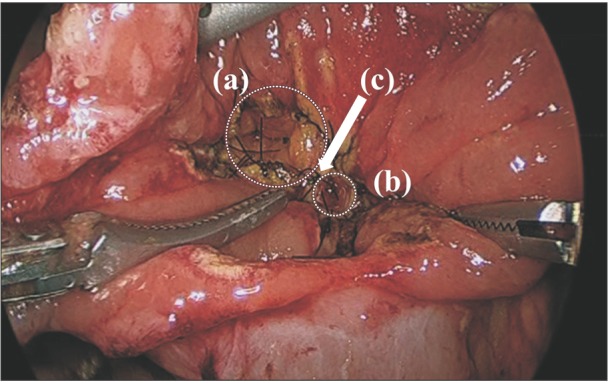 | Fig. 1Choledochoduodenostomy (a), pancreaticoduodenostomy (b), and common channel (c). After the lesion is excised with both ducts, single layer duct to mucosa choledochoduodenostomy, pancreaticoduodenostomy, and common channel between bile and pancreatic duct are done with 5/0 PDS (Ethicon US, LLC, Cincinnati, OH, USA).
|
Laparoscopic TDA
Under general anesthesia, the patient was placed in the supine and anti-Trendelenburg (10°–30°) position. The surgeon stood on the patient's right side, a 12-mm umbilical port was inserted, and pneumoperitoneum was established with carbon-dioxide (CO2) insufflation; intra-abdominal pressure was maintained at < 12 mmHg.
A laparoscope was used and additional 3 ports (two 5-mm and one 12-mm) were inserted as shown in
Fig. 2. Adequate kocherization was then performed. After locating the tumor, longitudinal duodenotomy of approximately 3 cm was performed on the antimesenteric side of the duodenum, just opposite the tumor. The ampullary mass was identified, and ampullectomy was performed using ultrasonic shears and by electrocautery. When the p-duct and CBD were identified, these were cut sharply with care to ensure an adequate margin.
 | Fig. 2Placement of trocars for laparoscopic transduodenal ampullectomy. (a) 12 mm trocar on the umbilicus for the right hand of the operator. (b) 5mm trocar on the right flank for the left hand of the operator. (c) 5mm trocar on the left flank for surgical assistance. (d) 12mm trocar for the laparoscope.
|
The specimen was inserted in a vinyl bag and extracted through the wound at the umbilical port. It was then sent to a pathologist for evaluation. The next steps are the same as for the open technique.
Statistical analysis
The categorical variables are presented as number (%). The continuous variables are presented as mean with standard deviation. The categorical variables were compared using the chi-square test or Fisher exact test according to the minimum expected count. If the minimum expected count was <5, we used the Fisher exact test. Continuous variables were compared using a t-test. A P-value of <0.05 was considered statistically significant.
Ethical statement
The study protocol and all documents used were approved by the Institutional Review Board of Asan Medical Center (S2018-1164).
Go to :

RESULTS
Patients
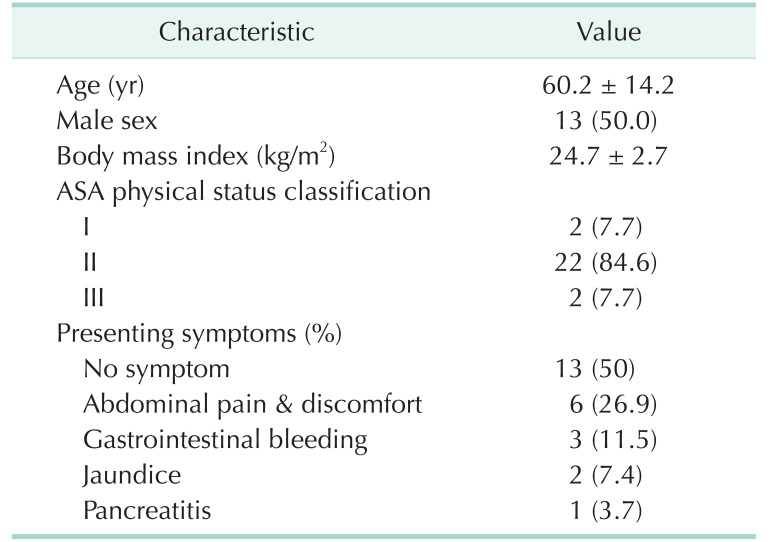
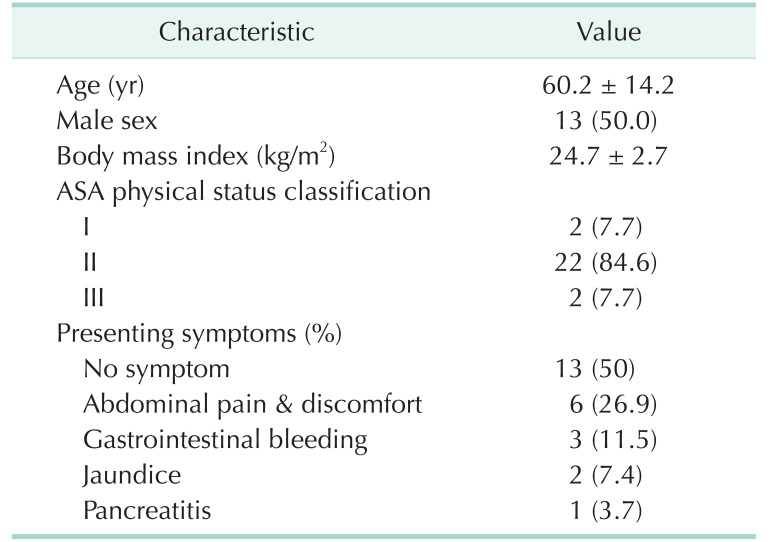
The demographic and clinical characteristics of the patients who underwent TDA are presented in
Table 1. The study subjects included 13 men and 13 women, with a mean age of 60 ± 14.2 years. Most patients were diagnosed by regular checkup without any symptoms (50%). The most frequently presenting symptom was abdominal pain/discomfort (26.9%), followed by gastrointestinal bleeding (11.5%) and jaundice (7.4%).
Table 1
Patient characteristics (n = 26)

Preoperative interventions, indications of TDA, and type of surgical procedure
Preoperative endoscopic biopsy was performed in all 26 patients. Three patients had adenocarcinoma. Two patients were very old, with poor general conditions, and the third patient had collateral enlarged varix connecting the superior mesenteric vein and main portal vein, which made PD difficult; all subsequently underwent TDA rather than PD. Preoperative endoscopic biopsies for the other 23 were adenomas and other benign masses such as hamartomatous mass or paraganglioma. Eight patients were offered TDA because of the huge size of the mass, 6 were due to HGD on endoscopic biopsy and 2 due to CBD invasion. Six patients experienced EP failure: 4 with incomplete resections with positive resection margins and 2 with recurrences of adenoma after EP. The last patient underwent TDA because of poor cooperation with EP.
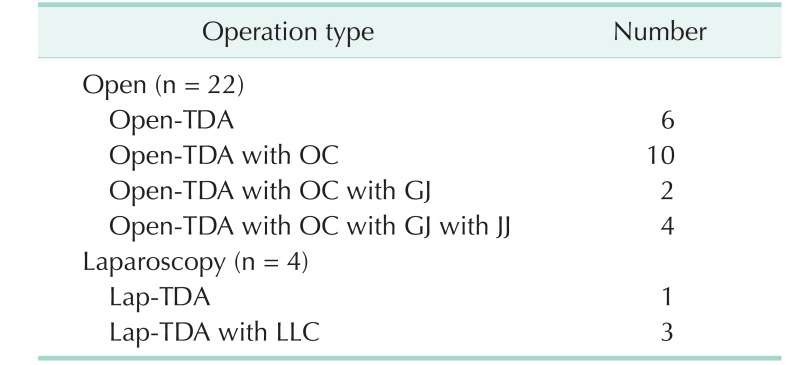
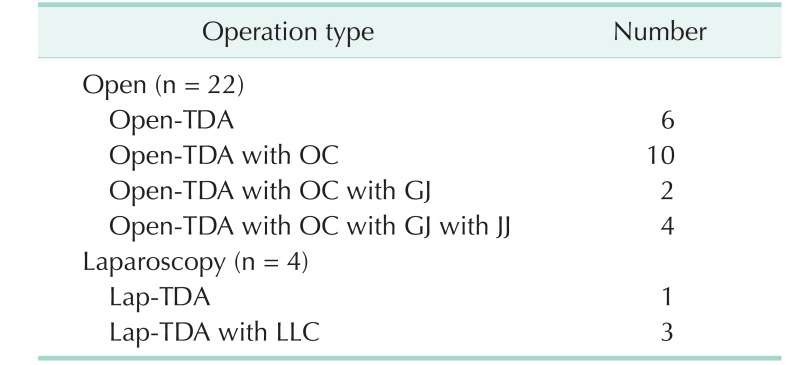
Open TDA was performed in 22 patients (84.6%), whereas laparoscopic-TDA (Lap-TDA) was performed in four (15.4%). Six underwent TDA with additional gastrojejunostomy (GJ; 23.1%).
The operation types are listed in
Table 2. One patient who underwent Lap-TDA switched to open PD because of severe bleeding. The patient was excluded from the present study.
Table 2
Operation type

Histological findings
FS analysis of the operative specimen was performed for all patients. FSs were obtained from the CBD and p-duct margin, and four lateral margins (3, 6, 9, and 12 o'clock) and were sent to a pathologist together with the orientation details. The resection margins for all the patients were negative.
For 3 preoperative biopsies proven to be invasive adenocarcinomas, FS analysis revealed invasive adenocar cinomas with negative resection margins. The final pathologies also revealed negative resection margins with T2 stage for three of them. The tumor sizes were 2, 1, and 1.5 cm, respectively.
The FS analysis result of one of the other 23 masses was cancer, but the resection margins were negative and the mass did not seem to be advanced; therefore, TDA was performed, rather than PD, after discussion with the guardian. Two cases were adenoma in the FS analyses, but identified to be invasive adenocarcinomas in the final pathological report. The final pathologies for three of them revealed T1 stage with negative resection margins.
Fifteen masses were confirmed as adenomas, 1 as gangliocytic paraganglioma, 1 as neuroendocrine tumor, 1 as having an hamartomatous nature, 1 as Brunner's gland hyperplasia, and 1 as intra-ampullary tubulopapillary neoplasm in both FS and final analyses.
The mean tumor size was 2 ± 1.4 cm. Postoperative histopathology revealed ampullary adenomas in 15 patients (57.7%). Of those, 7 had low-grade dysplasia and 8 had high-grade dysplasia (carcinoma in situ, Tis).
Perioperative outcomes
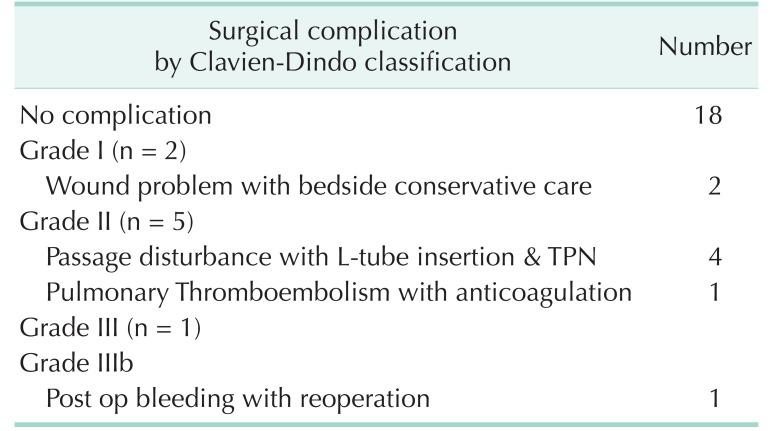
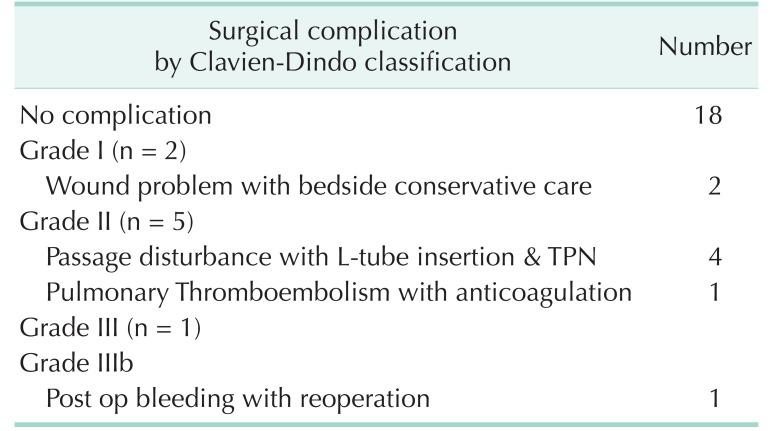
The mean operative time was 250.9 ± 63.3 minutes, and there was no case of 90-day mortality. In-hospital complications occurred in 8 patients (30.8%) and were classified according to the Clavien-Dindo Classification (
Table 3). Two wound problems (7.7%) occurred, which required bedside wound care and were classified as grade I. Five grade II complications (19.2%) occurred as follows: 4 cases of passage disturbance that needed nil per os (NPO) and total parenteral nutrition (TPN) therapy and 1 pulmonary thromboembolism (PTE), which needed anticoagulation. One patient underwent reoperation due to postoperative bleeding (grade IIIb, 3.8%).
Table 3
In hospital complications of 26 patients who underwent TDA (n = 26)

Follow-up and recurrence
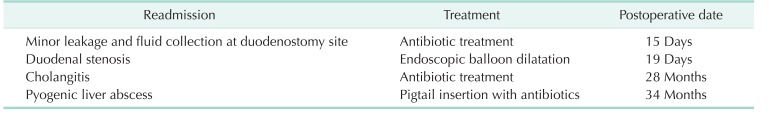
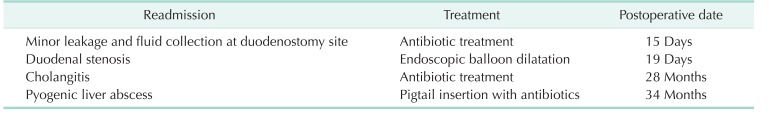
The mean follow-up was 72 ± 40 months. Two of 3 patients with adenocarcinoma (T2) had recurrence after TDA and died. One of them was diagnosed as having recurrence with multiple liver metastases after about 16 months after TDA, and the other one had recurrence with liver and lung metastases and peritoneal seeding after about 32 months after TDA. The remaining one patient had metachronous pancreatic cancer without recurrence 53 months after TDA. However, no recurrence occurred in the other patients with early cancer (Tis or T1), and benign and low grade malignant tumors. No newly onset DM was found after TDA. Complications occurred after discharge in four patients, and all of them were readmitted. One patient was readmitted 15 days after the discharge because of minor leakage at the duodenostomy site, and was treated with conservative care and antibiotics. The second patient was treated with NPO with TPN therapy because of duodenal stenosis and improved, but had to be readmitted only 19 days after discharge with worsened duodenal stenosis; this patient underwent balloon dilatation. The third patient was readmitted with cholangitis 28 months after the operation and received antibiotic therapy. The last one was readmitted because of liver abscess 34 months after the operation and treated with external drainage and antibiotics (
Table 4).
Table 4
Readmission of the patients who underwent transduodenal ampullectomy

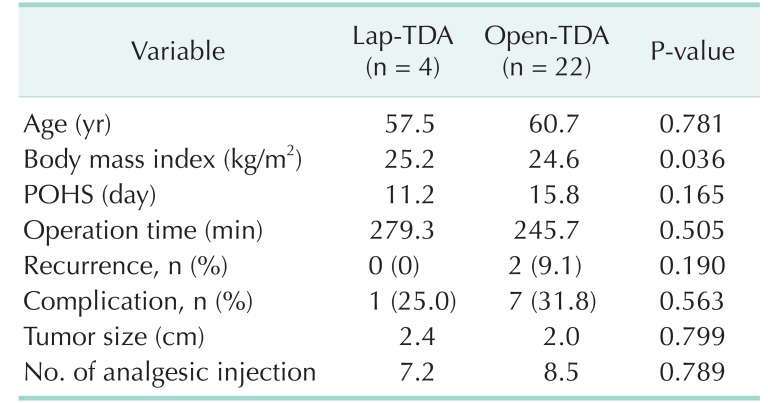
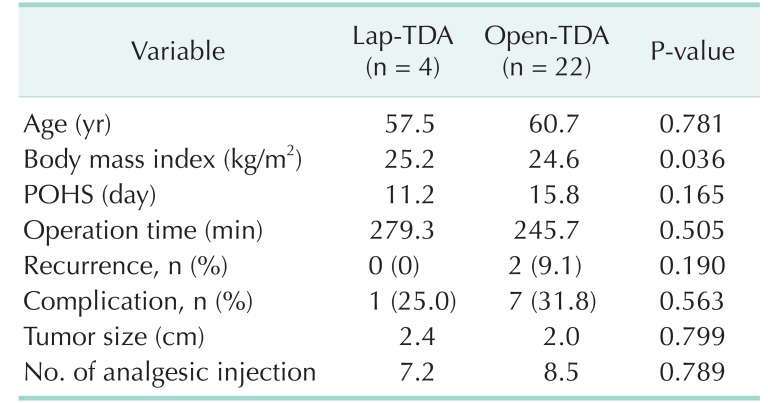
Comparison between open-TDA and Lap-TDA
Open-TDA was performed in 22 patients (84.6%) and Lap-TDA was performed in 4 patients (15.4%). Open-TDA took 245.7 minutes and Lap-TDA took 279.3 minutes (P = 0.505). The patients who underwent open-TDA took painkillers 7.5 times during hospital stay and those who underwent lap-TDA took painkillers 8.5 times (P = 0.789). The postoperative hospital stay (POHS) with open-TDA was longer than that with Lap-TDA, but the difference was not statistically significant (11 days
vs. 16 days, P = 0.165). The body mass index of the open-TDA group was higher than that of the Lap-TDA group (24.6
vs. 25.2, P = 0.036). One complication occurred in the Lap-TDA group and seven complications occurred in the open-TDA group, although the difference was not statistically significant (P = 0.563); 1 passage disturbance in the Lap-TDA group, and 2 wound problems, 3 passage disturbances, 1 PTE, and 1 postoperative bleeding in the open-TDA group (
Table 5).
Table 5
Lap-TDA versus Open-TDA

Go to :

DISCUSSION
In the present study, we report a single-center experience of 26 cases of TDA.
To our knowledge, this study represents the largest cohort reported in the literature so far. The results demonstrate that TDA is a feasible method with low morbidity and mortality rates, as well as good oncological outcomes and high long-term efficacy in terms of DM.
EP is an attractive option, as it involves no scars, allows for early return to routine life, and is associated with less morbidity and mortality than the other treatment options. In selected patients, EP is worth attempting especially for small-size tumors with low-risk malignancies [
451213]. However, it is difficult to perform full-thickness ampullectomy and to achieve a negative margin in multiple sessions with endoscopy alone. The procedure requires a highly skilled interventional endoscopist. In addition, EP is associated with several procedure-related complications, including pancreatitis, bleeding, perforation, cholangitis, and papillary stenosis. Therefore, the role of EP is limited to smaller lesions without features suggestive of tumor invasion to CBD and p-duct. In the present study, 6 patients underwent TDA after EP. Four patients experienced incomplete resection with positive resection margin and remnant adenoma, and the other 2 patients had recurrence after EP; they subsequently underwent TDA. By contrast, there was no recurrence after TDA for early cancer (Tis and T1) or adenoma showing successful complete resection.
Kim et al. [
14] reported a study in which 3 positive resection margins and 6 remnant tumors were found after 22 EPs, while 1 recurrence and 1 positive resection margin were found after 21 TDAs. EP is associated with higher rates of positive resection and false-negative margin results than TDA, which can result in tumor recurrence.
The surgical treatment of ampullary tumors mainly includes PD and TDA. PD has been widely accepted as the standard treatment approach for ampullary cancer, even though it is associated with high morbidity and mortality. On the contrary, TDA is a less invasive procedure than PD [
3681516]. The advantage of TDA is that it allows complete circumferential resection of the ampulla of Vater for precise pathological examination. It is also a feasible approach to avoid pancreatic head resection [
15].
Therefore, TDA should be indicated for patients not suitable for EP, such as those with large adenomas, those with HGD on endoscopic biopsy, and poor candidates for PD.
Surgeons also consider the risk of recurrence after TDA. A high local recurrence rate is predicted after TDA for advanced cancer, especially lymph node metastasis. Several studies have suggested PD as the choice of treatment for ampullary cancer owing to the risk of recurrence and chances of lymph node positivity [
1718]. On the other hand, in several other studies, TDA could be performed for Tis and T1 ampullary neoplasms without lymph node metastasis, showing similar 5-year survival and recurrence rates but lower surgical morbidity, estimated blood loss, intraoperative transfusion, and operation time than with PD [
1920]. The feasibility of TDA for ampullary cancer is remains controversial.
TDA has the advantage over PD in terms of pancreatic parenchymal preservation. Postoperative endocrine insufficiency, including DM, has been reported to develop following pancreatic resection. According to the previous study from our center, the development of DM is significantly correlated to pancreatic resection volume and residual volume ratio [
21]. The incidence of newly developed DM was up to 39% [
212223]. On the contrary, none of the patients reported newly developed DM in the present study. In addition, patients with DM had low quality of life because of the requirement of insulin, and the presence of depression and comorbidities, especially diabetic retinopathy. TDA can be suggested to prevent endocrine insufficiency that might occur after PD [
24].
Of the 26 patients, 4 had passage disturbance. They needed NPO with TPN therapy and showed improvement, but 1 of them had to be readmitted because of worsened duodenal stenosis; this patient underwent balloon dilatation with prolonged hospital stay. By contrast, no passage disturbance occurred in 6 patients who underwent additional GJ. Performing TDA with GJ might be an effective treatment option for preventing postoperative passage disturbance.
Currently, the application of laparoscopic surgery has been widened owing to increased experience and improved laparoscopic instrument. However, the use of Lap-TDA has been rarely reported. The laparoscopic approach has both strengths and weaknesses. Lap-TDA is still a challenging and technically demanding operation. In our study, 1 patient who underwent Lap-TDA patient underwent reoperation because of postoperative bleeding at the small bowel mesentery. Two Lap-TDA cases were converted to open procedure. The first case was converted to open-TDA because we could not find the opening because of fibrotic change around the ampulla of Vater; the patient underwent surgery because of failure of EP. In addition, though not included in this study, the second case experienced intraoperative bleeding during Lap-TDA and eventually underwent open PD. Laparoscopic surgery is still regarded as a difficult procedure that can be performed for highly selected patients by skillful surgeons.
By contrast, the laparoscopic approach is also recognized as a less invasive and favorable procedure than open surgery, with expectation of lower intraoperative blood loss and total amount of analgesics used and small size of the wound. Patients who underwent laparoscopic surgery also showed better quality of life in terms of physical, role, emotional, and social functioning [
2526].
In the present study, Lap-TDA was performed in 4 cases for ampullary tumors. Although it was not statistically significant, the POHS was shorter for Lap-TDA than that for open-TDA (P = 0.165). Painkillers were administered similarly to both the open TDA and Lap-TDA groups. However, among the 4 Lap-TDA patients, 1 patient took pain killers more frequently (21 times) than the others (<3 times). He had acute pancreatitis and underwent interventions such as EP once and argon plasma coagulation ablation 4 times because of recurrent adenoma and ERCP with endoscopic retrograde biliary and pancreatic drainage insertion before TDA. Therefore, he might have been more sensitive to pain and addicted to painkillers. Assuming this was an unusual case, we can propose that patients undergoing Lap-TDA experience have lesser pain than those undergoing open-TDA.
Although Lap-TDA is a challenging procedure, we could expect that it has typical advantages of a minimally invasive abdominal surgery, such as lower pain, quicker recovery times, and shorter hospital stays.
In conclusion, TDA is a feasible and effective surgical procedure for treatment of selected patients with ampullary tumors. It is an alternative treatment option for cases of ampullary tumors not amenable to EP or PD.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download