Abstract
Purpose
The purpose of this study was to determine the extent of safety of medial dissection of the thyroid gland along the trachea. Medial to lateral dissection of the thyroid gland along the trachea after early division of the isthmus has been known to be a useful technique in thyroid surgery, especially for difficult cases, but the risk of injury of the recurrent laryngeal nerve (RLN) has constrained thyroid surgeons from utilizing this technique to its full extent.
Methods
Distances of the laryngeal entry point (LEP) of 134 RLNs of 71 patients from the midline of the trachea, and some other anatomical distances, were measured intraoperatively. The relationships of the intraoperatively measured data with circumferences of the cartilaginous portion of the trachea (CCT) around LEP measured preoperatively by CT scan were evaluated.
Results
LEP was always located within 2 mm vertically from the horizontally extended line of the inferior border of the cricoid cartilage and was the closest point from the midline in the whole course of the RLN. The distance between LEP and the midline was very closely correlated with CCT measured on preoperative CT scan, and it can be accurately calculated with a regression equation; Distance between LEP and the midline = (0.42 × CCT) + (1.2 × sex) + 3.2 (mm) (sex: female=0, male=1; R2 = 0.85).
The thyroid gland is surrounded by one of the deep cervical fasciae, the pretracheal fascia, which splits to enclose and form a capsule over the thyroid gland. The thyroid capsule faces the deep layer of the superficial cervical fascia of the strap muscles anterolaterally, the carotid sheath posteromedially, and the trachea posteriorly. Around the cricoid cartilage and upper tracheal rings, this capsule is strongly condensed into the posterior suspensory, or Berry's ligament. Between these fasciae lie various vascular structures and the recurrent laryngeal nerves (RLNs).
Thyroidectomy involves dissection along its capsule while preserving critical structures such as the RLNs and the parathyroid glands. Various surgical techniques to facilitate the mobilization of the thyroid gland h ave been introduced. As Kocher described, and most thyroid surgeons do, the thyroid gland and laryngotracheal complex is medially retracted with simultaneous lateral retraction of the strap muscles. However, this technique cannot be applied to difficult cases, for example, huge goiters or severe Hashimoto's thyroiditis.
Early division of the isthmus can be helpful because it enables the thyroid gland to be dissected along the trachea in a medial to lateral direction. This procedure can ease mobilization of the thyroid gland and expose the operative field by separating the thyroid gland from its relatively strong attachment onto the cricoid cartilage and trachea. However, there are 2 possible problems in this procedure. The first is if there are isthmic nodules, and second, how to avoid direct injury of the RLN around the ligament of Berry in doing so. Preoperative ultrasonography gives us the exact location of every thyroid nodule, so the isthmus can be divided without touching the nodules in almost all cases. As for the second problem, the answer to the question of how far we can safely dissect the thyroid along the trachea is needed.
The laryngeal entry point (LEP) of RLN is important for several reasons. It is usually located around the inferior and medial border of the inferior constrictor muscle and approximately 1 cm below and just anterior to the inferior cornu of the thyroid cartilage (IC) that is palpable during operation [12]. LEP is also known to be the most constant and medial point in the notoriously variable course of RLN [12]. This study was performed to set a safe extent to which we can dissect the thyroid gland along the trachea in a medial to lateral direction by evaluating the relative location of LEP to several anatomic landmarks.
We performed a prospective study with 134 RLNs of 71 consecutive patients (113 RLNs of 60 females and 21 RLNs of 11 males) who underwent thyroid surgery from February 2009 to September 2009 in Hallym University Sacred Heart Hospital, Korea. Mean age was 47.34 years (range, 20 to 80 years). Patients whose preoperative neck CT scan was not available or who had large tumors (>5 cm) that might distort the neck anatomy or had been previously operated on were excluded from the study. The study protocol was approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (approval number: 2009-I040).
CT scans were performed preoperatively using multidetector CT scanners (Brilliance 64; Philips Medical systems, Best, The Netherlands) with a reconstructed slice thickness of 3 mm. Thyroid operations were carried out by two endocrine surgeons. Just after thyroidectomy, we exposed the whole course of RLN from near the neck base to LEP and measured the transverse distance from the midline of the trachea to LEP and the vertical distance from the transverse extension line of the inferior border of the cricoid cartilage to LEP. The distances between LEP and several other landmarks which could be identified during operation including the inferior tubercle and IC were also measured (Fig. 1). In case of any extralaryngeal branches of the RLN, the measurements were made with the anterior branch of the RLN, which is known as the motor branch. We also recorded where the closest point of RLN course from the midline of the trachea was located. Intraoperative measurements were carried out by 2 well-educated surgeons with measuring tapes and were recorded in millimeters (Fig. 2).
Independently, 1 author (KHK) measured the outer circumference of the cartilaginous portion of the trachea (CCT) on the CT scan at the estimated LEP level without knowing the intraoperatively measured data. The LEP level in the CT scan was regarded as the cut where the cricoid cartilage ring first disappeared while moving downward (Fig. 3). Thereafter, we evaluated the relationship between the measured data. We focused especially on the relationship of the distance between LEP and the midline of the trachea with CCT measured on the CT scan and tested the relationship using Pearson correlation analysis. For statistical analysis, we used SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
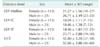
The vertical distance between LEP and the transverse extension line of the inferior border of the cricoid cartilage was within ± 2 mm in all patients. LEP was always the closest point from the midline of the trachea in the course of RLN and was located lateral to the Berry ligament. There was no nonrecurrent nerve in our cases. In females, the minimum and the maximum distance between LEP and the midline of the trachea were 18 and 27 mm, respectively, and the mean value was 21.27 mm. In males, the minimum, maximum, and mean were 23, 33, and 26.71 mm, respectively. CCT around LEP measured on CT scans were between 37 and 58 mm with the mean value of 42.80 mm in females, and between 46 and 60 mm with the mean value of 52.86 mm in males. The other measured data are also shown in Table 1.
When we performed Pearson correlation analysis to evaluate the relationship of the distance between LEP and the midline of the trachea, which was measured intraoperatively, with preoperatively measured CCT on the CT scan, there was a very strongly positive correlation with the correlation coefficients, r of 0.915 (Fig. 4). After correcting for the effect of sex, we carried out a multiple regression analysis with independent variables of CCT and sex to estimate the distance between LEP and the midline of the trachea. The following equation was acquired:
R2 of 0.85 means that the distance between LEP and the midline of the trachea can be explained by CCT and sex, for 85.1%, not 100% and, therefore, there is a difference between the calculated values and the real distances. If we were to dissect the thyroid gland along the trachea in a medial to lateral direc tion based on the calculated values without the risk of iatrogenic injury of RLN during dissection, the calculated values should always be less than the real distances. That is to say:
Residuals, meaning the gaps between the estimated values and the measured values, were analyzed to seek the safety margin. As a result, 2 mm and 3 mm of safety margins proved to protect more than 98% and 99.9% of RLN at risk, respectively.
In this study, we offer a safe extent for medial dissection of the thyroid gland along the trachea after early division of the isthmus, by estimating the location of LEP with inferior border of cricoid cartilage and CCT measured on preoperative CT scan. This study is significant in several aspects. Firstly, this is the earliest report to suggest a mathematic equation based on measurements from live humans, which can be used to determine LEP during operations.
The inferior thyroid artery, the IC, the ligament of Berry, and the tubercle of Zuckerkandl have been used as landmarks in the search for the RLN. Traditionally, the technique of identifying the RLN at its crossing with the inferior thyroid artery has been used by the many surgeons. Although this technique is relatively simple and reliable in the majority of cases, occasional anatomic variations of both the artery and nerve [34], and in those particular cases where the access to the inferior pole of the thyroid is difficult [5], may be problematic. Regarding the relationship of the RLN to the ligament of Berry, there are controversies in the literature. Berlin [6] and Yalcin and Ozan [7] reported that some RLNs penetrate through the ligament of Berry posteriorly. On the other hand, Sasou et al. [8] and Moreau et al. [3] observed that in all cases the nerve was dorsolateral to the ligament just as in our study. According to our observations, the RLN may be attached to the thyroid capsule but never penetrates it or its condensation, the ligament of Berry. The tubercle of Zuckerkandl, if present, can also be used to search the RLN because in general, the RLN passes medial to it in a fissure [9].
As a consistent and palpable landmark indicating LEP, the IC was described by some authors [12]. LEP is generally expected to be located approximately 1 cm below and just anterior to it, and Cakir et al. [1] reported that the mean distances between LEP and IC were 11.22 mm and 11.74 mm in female and male autopsies, respectively. Our data showed slightly shorter than Cakir's report (10.04 mm in females and 10.86 mm in males) and that is regarded to reflect the differences between different ethnic groups and between autopsies and live humans. Although we also identified the relationship of IC to LEP, the rough palpation of IC was not very helpful in identifying the LEP during operation because of its relatively deep-seated location. In their study, Cakir et al. [1] measured not only the distance of IC to LEP, but also that of inferior tubercle and the most anterior portion of the arch of the cricoid cartilage to LEP in 65 adult autopsies, and they concluded these three landmarks are reliable markers for the identification of LEP. However, according to our experiences, finding the LEP with mean distances from these 3 landmarks during operation was not as easy as measuring distances between LEP and the landmarks. On the other hand, it was relatively easy to search for a point that was located at the height of the inferior border of the cricoid cartilage and as far from the midline as the calculated distance along the trachea. Furthermore, our method can correct for sex and size variation between the individuals.
The second significance of our report is that we suggested a safe guidance method for medial dissection of the thyroid gland along the trachea after early division of the isthmus for the first time. This technique in thyroid surgery has been commented on in some textbooks and articles. Randolph [10] introduced this technique in their textbook as a useful maneuver for the exposure of the superior thyroid pole region, in situations when the dissection is, for whatever reason, difficult. But they also pointed out that isthmus division early on does not significantly enhance lobe mobilization because the thyroid lobe is still anchored firmly to the airway by the more lateral ligament of Berry [10]. In another textbook, when searching for the nerve at its usual cross point with the inferior thyroid artery is difficult or impossible, it is very useful to find the RLN at its LEP, which requires previous dissection of the upper pole, or an “inside-out” approach, after division of the isthmus [11]. Furthermore Page et al. [5] reported 25 patients with cervicothoracic goiter who underwent total thyroidectomy, and in their study, early division of the isthmus was performed when possible to facilitate the operation. As in the previous study, this ‘medial to lateral dissection’ was usually reserved only for especially difficult cases.
For some types of oncoplastic or cosmesis oriented thyroidectomy, the ‘medial to lateral dissection’ after early division of isthmus is being used routinely. In Bilateral Axillo-Breast Approach technique of endoscopic or robotic thyroidectomy, the isthmus is divided in the early stage using a harmonic scalpel [121314]. More recently, in ‘natural orifice surgery on thyroid gland’ or ‘transoral access for endoscopic thyroid resection’ as well, isthmus transection and blunt dissection of the thyroid gland from the trachea were performed as soon as the isthmus was exposed [1516]. Even in conventional open surgery, a certain portion of endocrine surgeons, at least in Korea, divide the isthmus early for its known or personally experienced advantages. One clear advantage of medial dissection of the thyroid gland is that it mobilizes the thyroid lobe and facilitates the exposure of the lateral surface and superior pole of the thyroid. Consequently, it might prevent traction injury of the RLN, the most frequent type of injury caused by excessive traction of the thyroid gland intended for its exposure [17]. In a similar way, it can contribute to the protection of the external branch of superior laryngeal nerve during dissection of the superior thyroid pole. Although it can make thyroid surgery easier and safer, especially in difficult cases, there has never been an objective description on the extent of medial dissection along the trachea. In this study, the authors suggested a safe and accurate extent for medial dissection calculated with sex and CCT measured on the preoperative CT scan. We believe that to maximize the advantages of medial dissection and to avoid the tragedy of injury to the RLN during this maneuver, our results would be very helpful.
A potential criticism of our study is that the data were produced from the measurement on the preoperative CT scan. Although CT scan is not recommended as a routine imaging tool for thyroid surgery for now, its complementary role to ultrasonography for detecting cervical metastatic lymph nodes in thyroid malignancy and its worth for evaluating the extent of large goiter enables CT scan to be used more frequently [1819]. In our institution, we routinely perform CT scan for thyroid malignancies and substernal goiters. The iodine load for CT scan may also be problematic [20]. However, about 2- to 3-month intervals between CT scan and radioiodine ablation therapy can minimize its effect [19]. Since the results were achieved, the authors applied medial dissection of the thyroid gland routinely, with the exception of 2 cases with large isthmic nodules, in 141 thyroid operations including 134 conventional open, 2 endoscopic, and 5 robotic thyroidectomies. With medial dissection, we could separate the thyroid gland almost completely from the trachea and cricoid cartilage except for several millimeters around the ligament of Berry without experiencing any injury of the RLN during the procedure. In doing so, interestingly, we found that measuring CCT on preoperative CT scan is not always necessary to determine a safe extent for medial dissection.
LEP was always lateral to the Berry ligament and the closest point from the midline of the trachea in the course of RLN. Therefore, we can detach the thyroid gland completely and safely from the mid and lower part of the trachea, where the RLN is relatively far from the trachea, without preoperatively calculated values. The tracheal cartilaginous circumferences around the mid or lower part of the trachea perceived intraoperatively are almost the same as those around LEP. Although LEP is still lateral to the trachea, for the sake of the safety, we should leave several millimeters around LEP, at the level of the inferior border of the cricoid cartilage. To facilitate a safe dissection, keeping to the exact plane between the thyroid and the trachea with lateral retraction of the thyroid lobe and medial retraction of the trachea is important. If one only keeps this plane precisely, he or she would never encounter the RLN but only the cartilage deficient trachea posterior surface, instead, if the dissection went too far.
In conclusion, LEP was always the closest point from the midline and had a similar height with the inferior border of the cricoid cartilage. In addition, the distance between LEP and the midline could be calculated by CCT measured on CT scan. Based on these results, early division of the isthmus and dissecting the thyroid off the trachea to the calculated extent can be a safe and effective procedure.
Figures and Tables
Fig. 1
Anatomical landmarks, related to laryngeal entry point of recurrent laryngeal nerve (LEP). A, midline of the trachea; B, transverse extension line of the inferior border of cricoid cartilage.
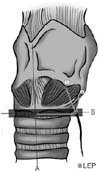
Fig. 2
Measuring the distance between the LEP and the midline of the trachea on the right side with a measuring tape after the removal of the thyroid gland. LEP, laryngeal entry point of recurrent laryngeal nerve.

Fig. 3
Two consecutive levels of 3mm thickness CT scan. (A) The cricoid cartilage ring is seen. (B) The cricoid cartilage ring has disappeared. We measured outer cir cumference of cartilaginous portion of the trachea on this level.
Fig. 4
The regression graph showing a close correlation of the distance between LEP and the midline of the trachea with CCT measured on the preoperative CT scan. LEPMidline, the distance between the laryngeal entry point of recurrent laryngeal nerve and the midline of the trachea; CCT, circumference of cartilaginous portion of the trachea.

References
1. Cakir BO, Ercan I, Sam B, Turgut S. Reliable surgical landmarks for the identification of the recurrent laryngeal nerve. Otolaryngol Head Neck Surg. 2006; 135:299–302.

2. Wang C. The use of the inferior cornu of the thyroid cartilage in identifying the recurrent laryngeal nerve. Surg Gynecol Obstet. 1975; 140:91–94.
3. Moreau S, Goullet de Rug M, Babin E, Salame E, Delmas P, Valdazo A. The recurrent laryngeal nerve: related vascular anatomy. Laryngoscope. 1998; 108:1351–1353.

4. Sturniolo G, D'Alia C, Tonante A, Gagliano E, Taranto F, Lo Schiavo MG. The recurrent laryngeal nerve related to thyroid surgery. Am J Surg. 1999; 177:485–488.

5. Page C, Peltier J, Charlet L, Laude M, Strunski V. Superior approach to the inferior laryngeal nerve in thyroid surgery: anatomy, surgical technique and indications. Surg Radiol Anat. 2006; 28:631–636.

6. Berlin DD. The recurrent laryngeal nerves in total ablation of the normal thyroid gland: an anatomical and surgical study. Surg Gynecol Obstet. 1935; 60:19–26.
7. Yalcin B, Ozan H. Detailed investigation of the relationship between the inferior laryngeal nerve including laryngeal branches and ligament of Berry. J Am Coll Surg. 2006; 202:291–296.
8. Sasou S, Nakamura S, Kurihara H. Suspensory ligament of Berry: its relationship to recurrent laryngeal nerve and anatomic examination of 24 autopsies. Head Neck. 1998; 20:695–698.

9. Pelizzo MR, Toniato A, Gemo G. Zuckerkandl' tuberculum: an arrow pointing to the recurrent laryngeal nerve (constant anatomical landmark). J Am Coll Surg. 1998; 187:333–336.
10. Randolph GW. Surgery of the thyroid and parathyroid glands. Philadelphia (PA): W.B. Saunders;2003.
11. Clark OH, Duh QY, Kebebew E. Textbook of endocrine surgery. 2nd ed. Philadelphia (PA): Elsevier Saunders;2005.
12. Lee KE, Rao J, Youn YK. Endoscopic thy roidectomy with the da Vinci robot sys tem using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech. 2009; 19:e71–e75.
13. Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, et al. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg. 2007; 31:2302–2306.

14. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606.

15. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endo scopic thyroid resection. Surg Endosc. 2008; 22:1871–1875.
16. Benhidjeb T, Wilhelm T, Harlaar J, Kleinrensink GJ, Schneider TA, Stark M. Natural orifice surgery on thyroid gland: totally transoral video-assisted thy roidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc. 2009; 23:1119–1120.
17. Snyder SK, Lairmore TC, Hendricks JC, Roberts JW. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg. 2008; 206:123–130.

18. Ahn JE, Lee JH, Yi JS, Shong YK, Hong SJ, Lee DH, et al. Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg. 2008; 32:1552–1558.

19. Kim E, Park JS, Son KR, Kim JH, Jeon SJ, Na DG. Preoperative diagnosis of cervical meta static lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid. 2008; 18:411–418.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download