Abstract
Purpose
Nowadays, minimally invasive surgical approach in thyroid surgery is getting more and more attention. The purpose of this report is to describe the surgical technique of transoral robotic thyroidectomy (TORT) in the cadaveric model which is the one of these minimally invasive methods.
Methods
Transoral thyroidectomy through vestibular approach was performed on 67 year old lady fresh cadaveric model. The da Vinci Xi surgical system (Intuitive Surgical, Inc.) was used to complete TORT. Total thyroidectomy was successfully completed.
Nowadays, the aim of all newly developed operation tecniques is to minimize postoperative pain, improve cosmetic results, and potentially reduce the length of hospital stay. Thyroid surgery is being performed at increasing frequency. Traditionally, thyroidectomy is usually performed through a midline neck skin incision which first described by Kocher in the late 1880s (1). Although this technique is safe, it has a disadvantage of a visible scar. First endoscopic thyroidectomy described in 1997 (2). Since this time there have been a great number of endoscopic and remote-access approaches to the neck described to minimize the cervical scar. These include thyroidectomy through chest (3), breast (4), axillary (56), bilateral axillo-breast aproach (7), and retroauricular (8) incisions. Each approach is far from perfect and fails to satisfy the criteria of minimally invasive surgery which aims to minimize surgical trauma.
Transoral thyroidectomy is recently described as a new method for minimally invasive thyroid resection. This tecnique was first described by Witzel et al. (9) using a single access port that included an accessory anterior neck port. After this technique Wilhelm et al. (10) described the transoral video-assisted thyroidectomy (TOVAT) technique which is an entirely transoral endoscopic approach, Karakas et al. (11) were the first to perform a transoral thyroid and parathyroid surgery using a lateral sublingual approach. Richmon et al. (12) also introduced a transoral technique for robotic thyroidectomy using the TOVAT method. The use of robots (da Vinci robot; Intuitive Surgical, Inc., Sunnyvale, CA, USA) in remote thyroid surgery is not novel and has since been demonstrated to be safe and to provide oncologic outcomes that are equivalent to open thyroidectomy with improved cosmesis, patient satisfaction and quality of life (13). The system provides a high-resolution, 3-dimensional view, which provides the surgeon with both depth perception and high magnification which aids with tissue handling, and identification of structures such as the recurrent laryngeal nerve and parathyroid glands, tremor filtration, precise movement with motion scaling, and individual camera operation. When contrasted with other remote-access approaches, the transoral robotic thyroidectomy (TORT) offers the potential for limited dissection and a completely hidden incision. Here we descirbe our experience using the transoral robotic vestibular approach for thyroidectomy on cadaveric model.
Transoral thyroidectomy through vestibular approach was performed on 67 years old lady fresh cadaveric model. The da Vinci Xi surgical system (Intuitive Surgical, Inc.) was used to complete TORT.
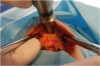
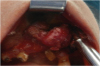
The cadaver was female who had no full dental structure. The patient was positioned supine, the neck was extended and a vestibular approach was utilized. To place the trochars a 3 cm transverse incision was performed in the midline of the lower lip at approximately 1 cm above the gingivobuccal sulcus (Fig. 1). Electrocautery was used to reach the mandibular periosteum. Once the submental space was reached and a pocket was created, a blunt-tipped dilator is used to develop the submental and subplatysmal plane atraumatically in the midline. Then, a 12-mm port was inserted fort he camera and 5-mm ports are passed lateral for the effector arms (Fig. 2). Insufflation tubing was attached to one of the cannulas and operation area expanded by CO2 insufflation at 5–7 mmHg. After surgical area prepared and trocars were placed, the da Vinci Xi surgical system (Intuitive Surgical, Inc.) was brought in and docked (Fig. 3). A 30° endoscope was advanced through the 12-mm port and a Maryland dissector and anaergy device were placed through the other ports. Under endoscopic visualization, first the platysma was elevated from the level of the mandible to the sternum inferiorly and laterally to the sternocleidomastoid muscles. The upper margin of the flap was thyroid cartilage, lower margin was sternal notch and the lateral magrin was medial aspect of the sternocleidomastoid muscle. The dissection was continued down to the level of the thyroid cartilage notch and the median raphe of the strap muscles was identified and divided to expose the thyroid gland. The thyroid was divided at the isthmus and the posterior surface of the isthmus was detached from the trachea to the ligament of Berry. First the superior pole was lifted, and the superior thyroidal vessels were divided with the energy device. The superior parathyroid gland was identified and preserved during laterally dissection. The recurrent laryngeal nerve was then identified at its entry point. The gland was then retracted further medially, allowing for a capsular dissection. The dissection was continued by dissecting Berry's ligament and the specimen was removed through the camera port and right thyroidectomy was successfully completed (Fig. 4). Bilateral total thyroidectomy was performed by applying the same technique on the other thyroid lobe.
Bilateral total thyroidectomy was successfully performed with transoral robotic technique. Bilateral recurrent laryngeal nerves and all 4 parathyroid glands were visualized and preserved during operation. Postoperative control was performed with conventional incision and it was confirmed that the recurrent laryngeal nerve and parathyroid glands were preserved (Fig. 5).
Today thyroid surgery is performed increasingly frequency and also carries bad cosmetic appearance anxiety. Endoscopic endocrine neck surgery had begun with the first description of a parathyroidectomy using CO2 inflation in 1996 by Gagner (14). After this technique Miccoli described a video-assisted resection of the thyroid gland with an incision of only 20 mm in the front neck in 2001 and after this numerous new techniques have been defined for non-scarred thyroid surgery in the neck region (9). However, the majority of these methods have good cosmetic results, the procedure was not minimally invasive due to the length of the tracks of the trocars and a long access approach.
Thanks to developments in technology and robotic surgery da Vinci Xi surgical system can also be used in thyroid surgery. The da Vinci Xi surgical system provides a clear magnified 3-dimensional view of the surgical field and has wristed instruments to aid mobility in limited space (15). The TORT approach sought to overcome many of the limitations of endoscopic surgery such as non-wristed instrumentation, 2-dimensional visualization, and difficulty of manipulating the endoscopic camera during dissection (16).
Since the robotic system is strong, the teeth can break and the lip can be torn. It is important to wear a protective gear for the teeth as there is a risk of pressure and fructure during operation. Supportive sutures may be required to protect the rim.
On the contrary to other endoscopic approaches, the transoral approach provides a midline exposure and equivalent access to both the right and left thyroid lobes. Since the transoral approach is similar in appearance to the traditional open approach which is well known to experienced thyroid surgeons, the learning curve is much easier (17).
TORT can be performed safely in select patients by an experienced surgeon, scarless and provides equal access to both central necks as opposed to other remote-access approaches. With the need for larger patient numbers and longer follow-up times, TORT is may be more widely perfromed in the future and a valid alternative to conventional thyroid surgery.
References
1. McGreevy PS, Miller FA. Biography of Theodor Kocher. Surgery. 1969; 65:990–999.
2. Song CM, Tae K. Robotic thyroidectomy: evolution and outcomes. Hanyang Med Rev. 2016; 36:205–210.

3. Shimizu K, Akira S, Jasmi AY, Kitamura Y, Kitagawa W, Akasu H, et al. Video-assisted neck surgery: endoscopic resection of thyroid tumors with a very minimal neck wound. J Am Coll Surg. 1999; 188:697–703.

4. Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000; 10:1–4.

5. Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J. Endoscopic thyroidectomy by the axillary approach. Surg Endosc. 2001; 15:1362–1364.

6. Kang SW, Jeong JJ, Nam KH, Chang HS, Chung WY, Park CS. Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg. 2009; 209:e1–e7.

7. Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech. 2009; 19:e71–e75.
8. Byeon HK, Holsinger FC, Tufano RP, Chung HJ, Kim WS, Koh YW, et al. Robotic total thyroidectomy with modified radical neck dissection via unilateral retroauricular approach. Ann Surg Oncol. 2014; 21:3872–3875.

9. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871–1875.

10. Wilhelm T, Harlaar JJ, Kerver A, Kleinrensink GJ, Benhidjeb T. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol. 2010; 267:1285–1290.

11. Karakas E, Steinfeldt T, Gockel A, Westermann R, Kiefer A, Bartsch DK. Transoral thyroid and parathyroid surgery. Surg Endosc. 2010; 24:1261–1267.

12. Richmon JD, Pattani KM, Benhidjeb T, Tufano RP. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck. 2011; 33:330–333.

13. Adam MA, Speicher P, Pura J, Dinan MA, Reed SD, Roman SA, et al. Robotic thyroidectomy for cancer in the US: patterns of use and short-term outcomes. Ann Surg Oncol. 2014; 21:3859–3864.

14. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; 83:875.

15. Clark JH, Kim HY, Richmon JD. Transoral robotic thyroid surgery. Gland Surg. 2015; 4:429–434.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download