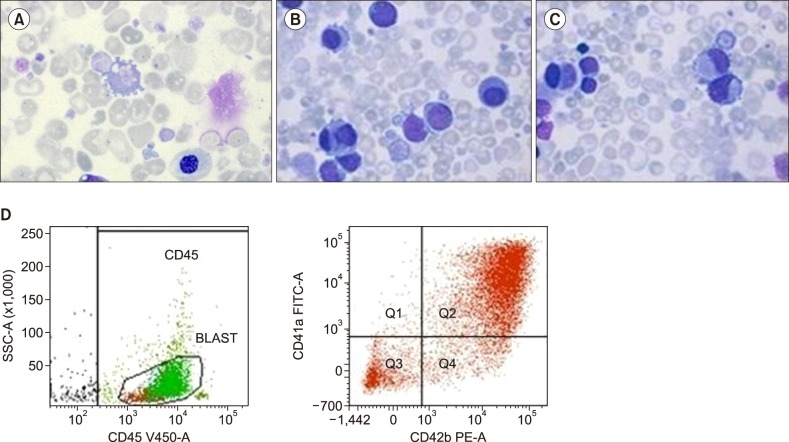
A small-for-gestational age male infant was born at 32 weeks of gestation, with Down syndrome, congenital heart disease, and hydrops. The total blood cell count results revealed 172.6×109/L leukocytes, anemia (hemoglobin of 97 g/L), and normal platelet count. The microscopic review of peripheral blood showed extremely high leukocyte count and most of the cells were blasts (90.5%). In particular, nucleated red blood cells, with abnormal platelet size and content, were found: (A) blasts had fine chromatin pattern with small distinct nucleoli (one or more), early platelet-type granulation of the cytoplasm and basophilic cytoplasm, and one binucleated micromegakaryocyte (B); some blasts also had cytoplasmic blebs (megakaryoblast), because their cytoplasm was remodeled into proplatelet protrusions (C) and micromegakaryocytes were found. A flow cytometric analysis of the peripheral blood showed that the expression of megakaryocytic markers (CD41a, CD42b) (D) was similar with that of megakaryoblastic acute leukemia (AML-M7), a rare type of acute myelogenous leukemia commonly found in children with Down syndrome. This syndrome is often preceded by transient abnormal myelopoiesis, a form of transient leukemia that is peculiar in newborns. The treatment option included chemotherapy with cytosine arabinoside. The patient died 10 days after birth due to sepsis caused by coagulase-negative Staphylococcus.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download