1. Wilson VJ, Jones GM. Mammalian vestibular physiology. New York: Plenum press;1979.
2. Yates BJ. Vestibular influences on the sympathetic nervous system. Brain Res Brain Res Rev. 1992; 17:51–59. PMID:
1638275.

3. Doba N, Reis DJ. Role of the cerebellum and the vestibular apparatus in regulation of orthostatic reflexes in the cat. Circ Res. 1974; 34:9–18. PMID:
4543723.

4. Yates BJ, Siniaia MS, Miller AD. Descending pathways necessary for vestibular influences on sympathetic and inspiratory outflow. Am J Physiol. 1995; 268:R1381–R1385. PMID:
7611512.

5. Park BR, Kim MS, Lee MY, Kim YK, Choi SC, Nah YH. Effects of galvanic stimulation of the mastoid process on the gastric motility induced by caloric stimulation. Auris Nasus Larynx. 1999; 26:263–268. PMID:
10419033.

6. Graybiel A, Miller EF 2nd, Newsom BD, Kennedy RS. The effect of water immersion on perception of the oculogravic illusion in normal and labyrinthine-defective subjects. Acta Otolaryngol. 1968; 65:599–610. PMID:
5706030.

7. Kennedy RS, Graybiel A, McDonough RC, Beckwith FD. Symptomatology under storm conditions in the North Atlantic in control subjects and in persons with bilateral labyrinthine defects. Acta Otolaryngol. 1968; 66:533–540. PMID:
5732654.

8. Kolev OI, Tibbling L. Vestibular and cardiac reactions to open-sea exposure. J Vestib Res. 1992; 2:153–157. PMID:
1342389.
9. Normand H, Etard O, Denise P. Otolithic and tonic neck receptors control of limb blood flow in humans. J Appl Physiol (1985). 1997; 82:1734–1738. PMID:
9173934.
10. Convertino VA. Interaction of semicircular canal stimulation with carotid baroreceptor reflex control of heart rate. J Vestib Res. 1998; 8:43–49. PMID:
9416588.

11. Yates BJ, Aoki M, Burchill P, Bronstein AM, Gresty MA. Cardiovascular responses elicited by linear acceleration in humans. Exp Brain Res. 1999; 125:476–484. PMID:
10323294.

12. Yates BJ, Miller AD. Properties of sympathetic reflexes elicited by natural vestibular stimulation: implications for cardiovascular control. J Neurophysiol. 1994; 71:2087–2092. PMID:
7931504.

13. Gotoh TM, Fujiki N, Matsuda T, Gao S, Morita H. Roles of baroreflex and vestibulosympathetic reflex in controlling arterial blood pressure during gravitational stress in conscious rats. Am J Physiol Regul Integr Comp Physiol. 2004; 286:R25–R30. PMID:
14500268.

14. Pemberton J. Does constitutional hypotension exist? BMJ. 1989; 298:660–662. PMID:
2496798.

15. Ohashi N, Imamura J, Nakagawa H, Mizukoshi K. Blood pressure abnormalities as background roles for vertigo, dizziness and disequilibrium. ORL J Otorhinolaryngol Relat Spec. 1990; 52:355–359. PMID:
2274319.

16. Yang CS, Young YH. Clinical investigation on hypotensive patients with vertigo. Eur Arch Otorhinolaryngol. 2006; 263:804–808. PMID:
16816934.

17. Park BR, Kim MS, Kim JH, Jin YZ. Effects of acute hypotension on neuronal activity in the medial vestibular nuclei of rats. Neuroreport. 2001; 12:3821–3824. PMID:
11726802.

18. Kim MS, Hyo Kim J, Kry D, Ae Choi M, Ok Choi D, Gon Cho B, Jin YZ, Ho Lee S, Park BR. Effects of acute hypotension on expression of cFos-like protein in the vestibular nuclei of rats. Brain Res. 2003; 962:111–121. PMID:
12543461.

19. Lee JO, Park SH, Kim HJ, Kim MS, Park BR, Kim JS. Vulnerability of the vestibular organs to transient ischemia: implications for isolated vascular vertigo. Neurosci Lett. 2014; 558:180–185. PMID:
24269984.

20. Jiang X, Li LW, Lan Y, Yang YZ, Jin GS, Kim MS, Park BR, Jin YZ. Comparative analysis of vestibular receptor and baroreceptor inputs to the nucleus tra rats. Neurosci Lett. 2014; 563:70–74. PMID:
24486893.
21. Bünemann L, Jensen KA, Riisager S, Thomsen LJ. Cerebral blood flow and metabolism during hypotension induced with sodium nitroprusside and metoprolol. Eur J Anaesthesiol. 1991; 8:197–201. PMID:
1874217.
22. Hamaguchi M, Ishibashi T, Katsumata N, Mitomi A, Imai S. Effects of sodium nitroprusside (MR7S1) and nitroglycerin on the systemic, renal, cerebral, and coronary circulation of dogs anesthetized with enflurane. Cardiovasc Drugs Ther. 1992; 6:611–622. PMID:
1292581.

23. Hasegawa M, Yokoyama K, Kobayashi N, Okamoto A, Tamura T, Watanabe I. Blood pressure and cochlear blood flow in the guinea pig. Acta Otolaryngol. 1989; 107:413–416. PMID:
2756833.

24. Preckel MP, Dégoute CS, Dubreuil C, Boulud B, Tassard AM, Banssillon V. Effects of buflomedil and naftidrofuryl on the human cochlear microcirculation measured by laser-Doppler. Rev Laryngol Otol Rhinol (Bord). 1995; 116:69–72. PMID:
7644852.
25. Angelborg C, Larsen HC. Blood flow in the peripheral vestibular system. J Otolaryngol. 1985; 14:41–43. PMID:
3877816.
26. Pujol R, Puel JL, Gervais d'Aldin C, Eybalin M. Pathophysiology of the glutamatergic synapses in the cochlea. Acta Otolaryngol. 1993; 113:330–334. PMID:
8100108.

27. Yamamoto K, Kubo T, Matsunaga T. Effects of asymmetric vertebral blood flow upon the vestibulo-ocular reflex of the rabbit. Arch Otorhinolaryngol. 1985; 241:195–202. PMID:
3872117.

28. Badoer E, McKinley MJ, Oldfield BJ, McAllen RM. Distribution of hypothalamic, medullary and lamina terminalis neurons expressing Fos after hemorrhage in conscious rats. Brain Res. 1992; 582:323–328. PMID:
1393554.

29. Krukoff TL, MacTavish D, Harris KH, Jhamandas JH. Changes in blood volume and pressure induce c-fos expression in brainstem neurons that project to the paraventricular nucleus of the hypothalamus. Brain Res Mol Brain Res. 1995; 34:99–108. PMID:
8750865.

30. Kim MS, Choi DO, Choi MA, Kim JH, Kim KY, Lee MY, Rhee JK, Chun SW, Park BR. Immunohistochemical detection of phosphorylated form of extracellular signal-regulated kinase 1/2 in rat vestibular nuclei following hemorrhagic hypotension. Neurosci Lett. 2004; 360:49–52. PMID:
15082176.

31. Li H, Godfrey DA, Rubin AM. Quantitative distribution of amino acids in the rat vestibular nuclei. J Vestib Res. 1994; 4:437–452. PMID:
7850040.

32. Smith PF, de Waele C, Vidal PP, Darlington CL. Excitatory amino acid receptors in normal and abnormal vestibular function. Mol Neurobiol. 1991; 5:369–387. PMID:
1668393.

33. Smith PF, Darlington CL, Hubbard JI. Evidence for inhibitory amino acid receptors on guinea pig medial vestibular nucleus neurons in vitro. Neurosci Lett. 1991; 121:244–246. PMID:
1850504.

34. Schousboe A, Pasantes-Morales H. Potassium-stimulated release of [3H]taurine from cultured GABAergic and glutamatergic neurons. J Neurochem. 1989; 53:1309–1315. PMID:
2769270.
35. Li XL, An Y, Jin QH, Kim MS, Park BR, Jin YZ. Changes of some amino acid concentrations in the medial vestibular nucleus of conscious rats following acute hypotension. Neurosci Lett. 2010; 477:11–14. PMID:
20399837.

36. Li XL, Nian B, Jin Y, Li LW, Jin GS, Kim MS, Park BR, Jin YZ. Mechanism of glutamate receptor for excitation of medial vestibular nucleus induced by acute hypotension. Brain Res. 2012; 1443:27–33. PMID:
22305141.

37. Choi MA, Lee JH, Hwang JH, Choi SJ, Kim MS, Park BR. Signaling pathway of glutamate in the vestibular nuclei following acute hypotension in rats. Brain Res. 2008; 1229:111–117. PMID:
18639534.

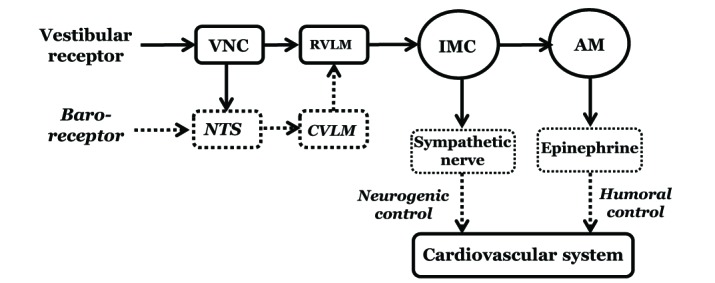
38. Lan Y, Lu HJ, Jiang X, Li LW, Yang YZ, Jin GS, Park JY, Kim MS, Park BR, Jin YZ. Analysis of the baroreceptor and vestibular receptor inputs in the rostral ventrolateral medulla following hypotension in conscious rats. Korean J Physiol Pharmacol. 2015; 19:159–165. PMID:
25729278.

39. Kumagai H, Oshima N, Matsuura T, Iigaya K, Imai M, Onimaru H, Sakata K, Osaka M, Onami T, Takimoto C, Kamayachi T, Itoh H, Saruta T. Importance of rostral ventrolateral medulla neurons in determining efferent sympathetic nerve activity and blood pressure. Hypertens Res. 2012; 35:132–141. PMID:
22170390.

40. Spyer KM. Neural organisation and control of the baroreceptor reflex. Rev Physiol Biochem Pharmacol. 1981; 88:24–124. PMID:
7010509.

41. Balaban CD, Beryozkin G. Vestibular nucleus projections to nucleus tractus solitarius and the dorsal motor nucleus of the vagus nerve: potential substrates for vestibulo-autonomic interactions. Exp Brain Res. 1994; 98:200–212. PMID:
8050507.

42. Holstein GR, Friedrich VL Jr, Kang T, Kukielka E, Martinelli GP. Direct projections from the caudal vestibular nuclei to the ventrolateral medulla in the rat. Neuroscience. 2011; 175:104–117. PMID:
21163335.

43. Kalia M, Mesulam MM. Brain stem projections of sensory and motor components of the vagus complex in the cat: II. Laryngeal, tracheobronchial, pulmonary, cardiac, and gastrointestinal branches. J Comp Neurol. 1980; 193:467–508. PMID:
7440778.

44. Yates BJ, Grélot L, Kerman IA, Balaban CD, Jakus J, Miller AD. Organization of vestibular inputs to nucleus tractus solitarius and adjacent structures in cat brain stem. Am J Physiol. 1994; 267:R974–R983. PMID:
7524372.

45. Jiang X, Lan Y, Jin YZ, Park JY, Park BG, Ameer AN, Park BR. Effect of vestibulosympathetic reflex and baroreflex on expression of pERK in the aucleus tractus solitarius following acute hypotension in conscious rats. Korean J Physiol Pharmacol. 2014; 18:353–358. PMID:
25177169.
46. Li LW, Jin GS, Yang YZ, Ameer AN, Kim MS, Park BR, Jin YZ. Effect of glutamate on the vestibulo-solitary projection after sodium nitroprusside-induced hypotension in conscious rats. Korean J Physiol Pharmacol. 2015; 19:275–281. PMID:
25954134.

47. Kerman IA, McAllen RM, Yates BJ. Patterning of sympathetic nerve activity in response to vestibular stimulation. Brain Res Bull. 2000; 53:11–16. PMID:
11033203.

48. Kerman IA, Yates BJ, McAllen RM. Anatomic patterning in the expression of vestibulosympathetic reflexes. Am J Physiol Regul Integr Comp Physiol. 2000; 279:R109–R117. PMID:
10896871.

49. Ray CA, Carter JR. Vestibular activation of sympathetic nerve activity. Acta Physiol Scand. 2003; 177:313–319. PMID:
12609001.

50. Radtke A, Popov K, Bronstein AM, Gresty MA. Evidence for a vestibulo-cardiac reflex in man. Lancet. 2000; 356:736–737. PMID:
11085696.

51. Guyenet PG, Haselton JR, Sun MK. Sympathoexcitatory neurons of the rostroventrolateral medulla and the origin of the sympathetic vasomotor tone. Prog Brain Res. 1989; 81:105–116. PMID:
2616776.
52. Lan Y, Yang YZ, Jiang X, Li LW, Jin GS, Kim MS, Park BR, Jin YZ. Additive role of the vestibular end organ and baroreceptors on the regulation of blood pressure in rats. Korean J Physiol Pharmacol. 2013; 17:367–373. PMID:
23946697.

53. Lu HJ, Li MH, Li MZ, Park SE, Kim MS, Jin YZ, Park BR. Functional connections of the vestibulo-spino-adrenal axis in the control of blood pressure via the vestibulosympathetic reflex in conscious rats. Korean J Physiol Pharmacol. 2015; 19:427–434. PMID:
26330755.

54. Park SE, Jin YZ, Park BR. Dual control of the vestibulosympathetic reflex following hypotension in rats. Korean J Physiol Pharmacol. 2017; 21:675–686. PMID:
29200911.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download