1. Kim BJ, Kim JS. Ischemic stroke subtype classification: an asian viewpoint. J Stroke. 2014; 16:8–17.

2. Sanak D, Hutyra M, Kral M, et al. Paroxysmal atrial fibrillation in young cryptogenic ischemic stroke: A 3-week ECG Holter monitoring study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015; 159:283–287.

3. Mozaffarian D, Benjamin EJ, Go AS, American Heart Association Statistics Committee and Stroke Statistics Subcommittee, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015; 131:e29–e322.
4. Tsang TS, Petty GW, Barnes ME, et al. The prevalence of atrial fibrillation in incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decades. J Am Coll Cardiol. 2003; 42:93–100.
5. Grau AJ, Weimar C, Buggle F, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001; 32:2559–2566.

6. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001; 285:2864–2870.

7. European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010; 31:2369–2429.
8. Khawaja O, Bartz TM, Ix JH, et al. Plasma free fatty acids and risk of atrial fibrillation (from the Cardiovascular Health Study). Am J Cardiol. 2012; 110:212–216.

9. Djoussé L, Benkeser D, Arnold A, et al. Plasma free fatty acids and risk of heart failure: the Cardiovascular Health Study. Circ Heart Fail. 2013; 6:964–969.
10. Al Chekakie MO, Welles CC, Metoyer R, et al. Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol. 2010; 56:784–788.

11. Ouchi N. Obesity: Progress in diagnosis and treatment; Topics, IV. Recent topics; 3. Obesity and new secretory factors; 2) Sfrp 5 acts as a novel adipocytokine that affects metabolic function. Nihon Naika Gakkai Zasshi. 2011; 100:1002–1007.
12. Chhabra L, Spodick DH. Role of epicardial fat in atrial fibrillation after coronary artery bypass surgery. Am J Cardiol. 2014; 113:2090.

13. Hendrickson SC, St Louis JD, Lowe JE, Abdel-aleem S. Free fatty acid metabolism during myocardial ischemia and reperfusion. Mol Cell Biochem. 1997; 166:85–94.
14. Mazzali G, Fantin F, Zoico E, et al. Heart fat infiltration in subjects with and without coronary artery disease. J Clin Endocrinol Metab. 2015; 100:3364–3371.

15. Pantanowitz L. Fat infiltration in the heart. Heart. 2001; 85:253.

16. Lin YK, Chen YC, Chen JH, Chen SA, Chen YJ. Adipocytes modulate the electrophysiology of atrial myocytes: implications in obesity-induced atrial fibrillation. Basic Res Cardiol. 2012; 107:293.

17. Abed HS, Samuel CS, Lau DH, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm. 2013; 10:90–100.

18. Hirata Y, Yamada H, Kusunose K, et al. Clinical utility of measuring epicardial adipose tissue thickness with echocardiography using a high-frequency linear probe in patients with coronary artery disease. J Am Soc Echocardiogr. 2015; 28:1240–1246.e1.

19. Tok D, Çağli K, Kadife I, et al. Impaired coronary flow reserve is associated with increased echocardiographic epicardial fat thickness in metabolic syndrome patients. Coron Artery Dis. 2013; 24:191–195.

20. Kim BJ, Kim BS, Kang JH. Echocardiographic epicardial fat thickness is associated with arterial stiffness. Int J Cardiol. 2013; 167:2234–2238.

21. Kim BJ, Kim BS, Kang JH. Echocardiographic epicardial fat thickness is associated with coronary artery calcification - results from the CAESAR study. Circ J. 2015; 79:818–824.
22. Sengul C, Cevik C, Ozveren O, et al. Echocardiographic epicardial fat thickness is associated with carotid intima-media thickness in patients with metabolic syndrome. Echocardiography. 2011; 28:853–858.

23. Stojanovska J, Kazerooni EA, Sinno M, et al. Increased epicardial fat is independently associated with the presence and chronicity of atrial fibrillation and radiofrequency ablation outcome. Eur Radiol. 2015; 25:2298–2309.

24. Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.

25. Oh MS, Yu KH, Lee JH, et al. Validity and reliability of a Korean version of the national institutes of health stroke scale. J Clin Neurol. 2012; 8:177–183.

26. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988; 19:1497–1500.

27. Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987; 59:956–960.

28. Shim IK, Cho KI, Kim HS, Heo JH, Cha TJ. Impact of gender on the association of epicardial fat thickness, obesity, and circadian blood pressure pattern in hypertensive patients. J Diabetes Res. 2015; 2015:924539.

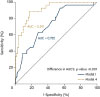
29. Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982; 247:2543–2546.

30. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.

31. Acet H, Ertaş F, Akıl MA, et al. New inflammatory predictors for non-valvular atrial fibrillation: echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Int J Cardiovasc Imaging. 2014; 30:81–89.

32. Soeki T, Sata M. Role of epicardial adipose tissue in atrial fibrillation. Circ J. 2012; 76:2738–2739.

33. Spence JD. Free fatty acids and stroke from atrial fibrillation. Can J Neurol Sci. 2011; 38:803.

34. Jickling GC, Spence JD. Free fatty acids to predict recurrent ischemic stroke. Neurology. 2014; 82:1110–1111.

35. Seo WK, Kim J, Kim YH, et al. Elevated free fatty acid is associated with cardioembolic stroke subtype. Can J Neurol Sci. 2011; 38:874–879.

36. Choi JY, Jung JM, Kwon DY, et al. Free fatty acid as an outcome predictor of atrial fibrillation-associated stroke. Ann Neurol. 2016; 79:317–325.

37. Koutsari C, Dumesic DA, Patterson BW, Votruba SB, Jensen MD. Plasma free fatty acid storage in subcutaneous and visceral adipose tissue in postabsorptive women. Diabetes. 2008; 57:1186–1194.

38. O'Connell RP, Musa H, Gomez MS, et al. Free fatty acid effects on the atrial myocardium: membrane ionic currents are remodeled by the disruption of T-tubular architecture. PLoS One. 2015; 10:e0133052.
39. Petrovičová A, Kurča E, Brozman M, et al. Detection of occult paroxysmal atrial fibrilation by implantable long-term electrocardiographic monitoring in cryptogenic stroke and transient ischemic attack population: a study protocol for prospective matched cohort study. BMC Cardiovasc Disord. 2015; 15:160.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download