INTRODUCTION
The thyroid gland is an endocrine gland that synthesizes and secretes thyroid hormones, which play crucial roles in the control of energy homeostasis and thermogenesis [
12]. Thyroid nodule is the most common thyroid disease. The incidence of thyroid nodules has been increasing worldwide in recent years, mainly caused by the widespread use of high-resolution neck ultrasonography (USG) and computed tomography [
34567]. Hypothyroidism is a pathological condition of deficient thyroid hormone, whereas hyperthyroidism is a disorder in which excess thyroid hormone is present [
12]. Understanding the current distribution of thyroid dysfunction in the population is important, because it is a potential risk factor for hypercholesterolemia, cardiovascular disease, osteoporosis, arrhythmia, and neuropsychiatric disease [
8].
The prevalence of thyroid nodules was found to be 14% to 29% among men and 28% to 42% among women in previous studies of subjects who underwent health checkups in Korea [
491011]. However, no studies have investigated the prevalence and annual incidence of thyroid nodules in the entire Korean population. The prevalence and incidence of thyroid dysfunction vary across populations and can be influenced by several factors such as age, sex, ethnicity, and iodine status [
121213]. The prevalence of hypothyroidism in the general population has been reported to be from 0.3% to 3.7% in the United States and from 0.2% to 5.3% in European countries [
181415]. When subclinical hypothyroidism is also included, the overall prevalence is as high as 15% [
1216]. The prevalence of overt hyperthyroidism has been reported as 0.5% to 0.8% in Europe and 0.5% in the United States [
814]. Although several studies have reported the prevalence and incidence of thyroid dysfunction in Korea, some studies were not able to take recent changes into account, and other studies did not reveal the current status of patients receiving treatment [
16171819].
This study aimed to investigate the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in the entire Korean population using the National Health Information (NHI) database after excluding subjects with thyroid cancer.
DISCUSSION
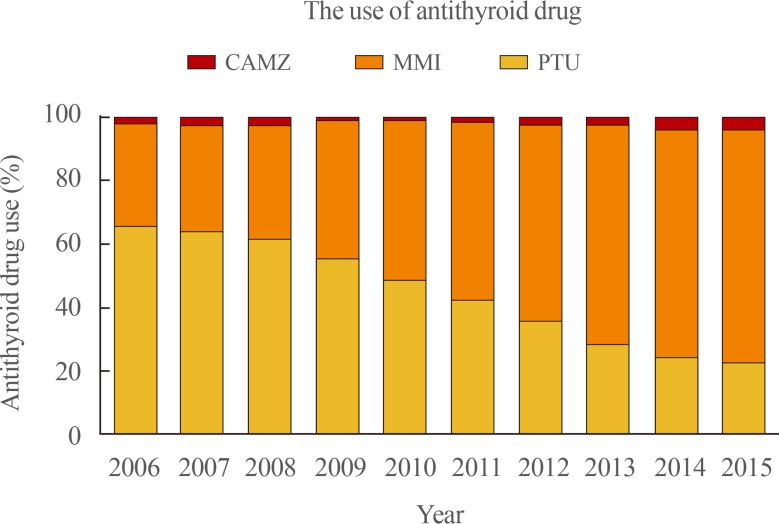
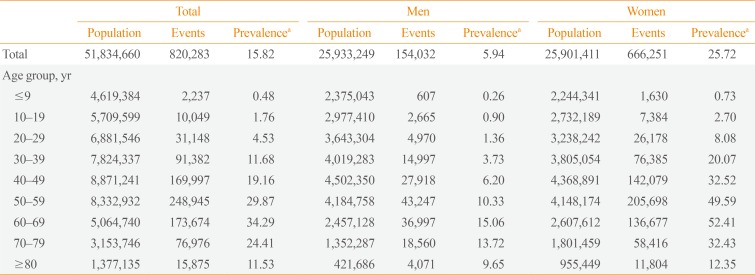
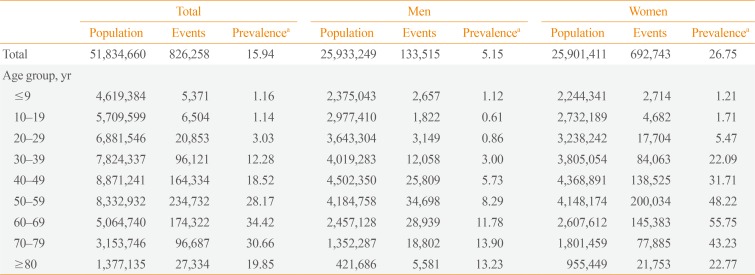
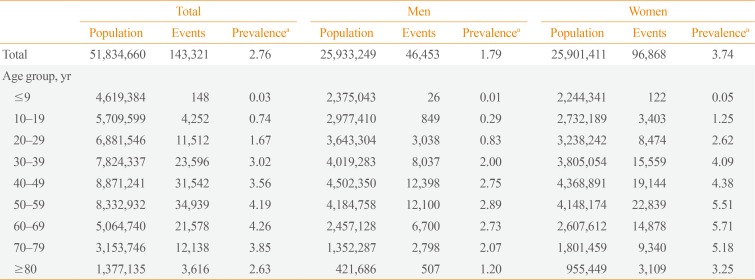
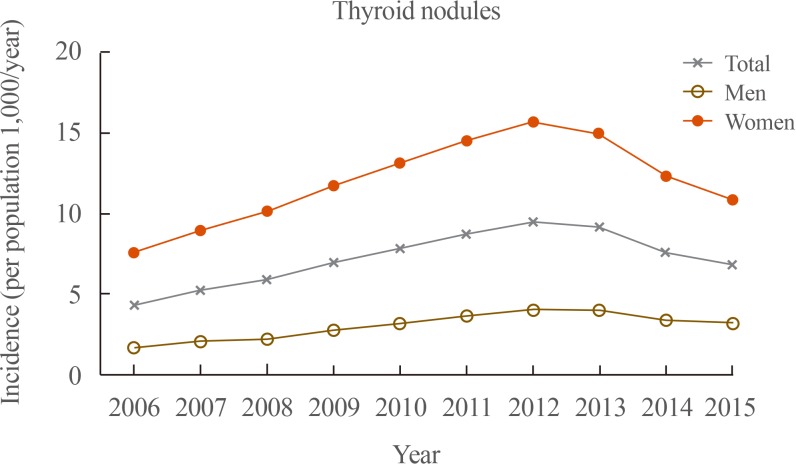
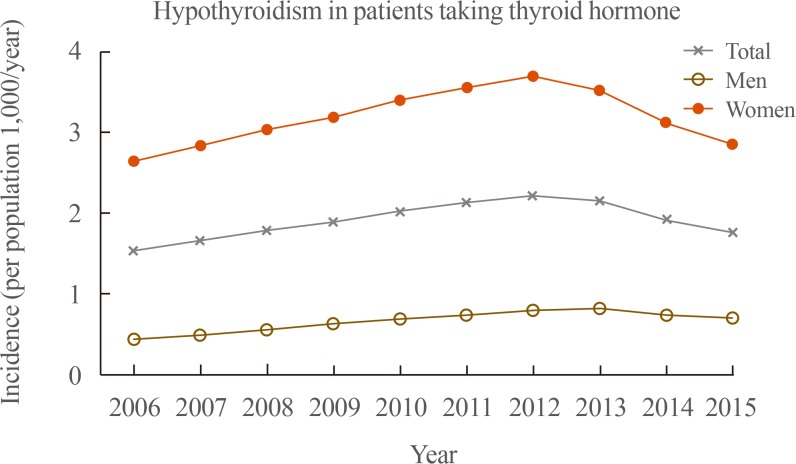
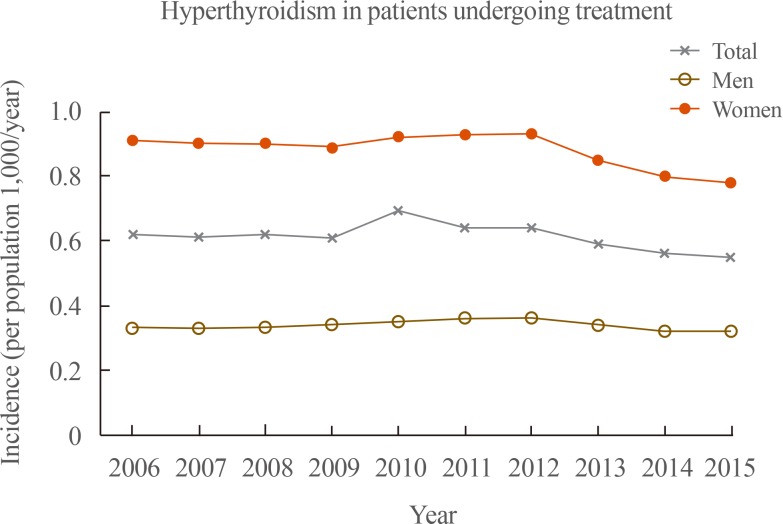
This nation-wide cross-sectional study investigated the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in Korea using the NHI database after excluding of subjects with thyroid cancer. The prevalence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population in Korea in 2015, respectively. All these diseases were more prevalent among women than among men. In total, the number of incident cases of these three thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population in Korea in 2015. The use of MMI continuously increased from 33% of total antithyroid drug prescriptions in 2006 to 74.4% in 2015, and it became the most frequently prescribed antithyroid drug in Korea, while the use of PTU continuously decreased.
Several studies of Korean subjects with thyroid nodules who underwent health checkups have been reported [
491011]. The prevalence of thyroid nodules was 14% to 29% among men and 28% to 42% among women [
491011]. However, those studies could not reflect the current state of the population and clinical practice, because the examinees of health checkup might be unusually interested in their health and have a relatively high prevalence of thyroid nodules. In the current study, the prevalence of thyroid nodules among men and women was 5.94/1,000 population and 25.72/1,000 population in 2015, respectively. The prevalence of thyroid nodules was the greatest in the 60 to 69 years age group among both men (15.06/1,000 population) and women (52.41/1,000 population).
In the current study, 5.15/1,000 population among men and 26.75/1,000 population among women took thyroid hormone due to hypothyroidism. Several studies have investigated the prevalence and incidence of hypothyroidism in Korea [
161719]. A previous study using claims data provided by the Health Insurance Review and Assessment Service (HIRA) reported that the prevalence of hypothyroidism was 14.28/1,000 population in Korea in 2015 [
17]. Another cohort study reported that the prevalence of subclinical hypothyroidism in the Ansung cohort and Korean Longitudinal Study on Health and Aging Study was 11.7% and 17.3%, respectively [
19]. Recently, a study investigated the prevalence of hypothyroidism and hyperthyroidism using the Korea National Health and Nutrition Examination Survey VI (KNHANES VI, 2013 to 2015) by applying the reference interval of serum thyroid stimulating hormone in the Korean reference population [
16]. The study reported that the prevalence of overt and subclinical hypothyroidism was 0.73% and 3.10%, respectively [
16]. However, the study could not reflect the actual clinical prevalence of the disease, because the authors evaluated the prevalence of the disease after excluding patients with a prior history of thyroid disease or taking medicine that could influence thyroid function [
16].
The prevalence of hyperthyroidism in patients undergoing treatment was 1.79/1,000 population among men and 3.74/1,000 population among women in this study. The prevalence of hyperthyroidism reported by previous studies from Korea was similar to that of other countries [
814]. In a previous study published in 2013 using the HIRA database, the prevalence of hyperthyroidism was 3.40/1,000 population (2.09 among men and 4.70 among women), and the incidence of hyperthyroidism was 0.72/1,000 population (0.40 among men and 1.03 among women) [
18]. The study using the KNHANES VI reported that the prevalence of overt and subclinical hyperthyroidism in the disease-free population was 0.54% and 2.98%, respectively [
16].
The number of incident cases of thyroid nodules, hypothyroidism, and hyperthyroidism steadily increased from 2006 to 2012, and then decreased to 2015. In 2010, the Korean Thyroid Association (KTA) presented revised guidelines for the diagnosis and management of thyroid nodules and cancer and size criteria of thyroid nodules for applying fine-needle aspiration cytology (FNAC) based on the risk factors for thyroid cancer [
21]. They recommended that FNAC should be performed in nodules larger than 5 mm, even if in patients at a high risk for thyroid cancer or with malignant features on neck USG [
21]. For these reasons, physicians might have started to perform examinations less frequently, not only for thyroid nodules and cancer, but also for thyroid dysfunction. Ahn and Welch [
22] reported that the number of operations for thyroid cancer decreased after screening for thyroid cancer with USG was discouraged in March 2014. However, the current study showed that the incidence of thyroid nodules, hypothyroidism, and hyperthyroidism decreased starting in 2013.
Recently, MMI became the most frequently prescribed antithyroid drug among the three types of antithyroid drugs (PTU, MMI, and CAMZ). PTU was the most commonly used drug for patients with hyperthyroidism before 2009, but MMI overtook PTU in 2010. The U.S. Food and Drug Administration added a new boxed warning to the label for PTU about severe liver injury in 2010, because PTU can lead to potentially fatal fulminant hepatic necrosis [
232425]. The American Thyroid Association and American Association of Clinical Endocrinologists guidelines, as well as the KTA guidelines, recommended using MMI to treat hyperthyroidism, except within the first trimester of pregnancy and in patients experiencing thyrotoxic crisis [
2526]. For these reasons, the trends in physician's prescriptions changed and MMI became the most frequently prescribed antithyroid drug in 2015.
This retrospective cohort study has several limitations. Because of its population-based design, this study could be subject to several biases, including coding bias, selection bias, and the effects of confounding factors. A possible discrepancy existed between the actual diagnosis and claim data because the NHIS database depends on the diagnostic code and prescription submitted on the physician's claim. In addition, the NHIS database does not contain information about prescriptions not covered through insurance. Data from thyroid function tests were not available in this study. We were not able to include subjects who had hypothyroidism and did not receive medication or those with hyperthyroidism who did not receive treatment. We could not evaluate the causative disease of hypothyroidism and hyperthyroidism. We excluded subjects diagnosed with thyroid cancer, even if they had been treated for thyroid dysfunction or had thyroid nodules. This could have led us to underestimate the prevalence and incidence of these thyroid diseases. Nevertheless, this was the first study of the prevalence and annual incidence of thyroid nodules in the entire Korean population. We investigated the prevalence and annual incidence of hypothyroidism and hyperthyroidism, taking into account recent changes and including the current status of patients receiving treatment.
In conclusion, the prevalence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population, respectively, in Korea in 2015 using the NHI database after excluding subjects with thyroid cancer. All these diseases were more prevalent among women than among men. The number of incident cases of these thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population in Korea in 2015. MMI is now the most frequently prescribed antithyroid drug in Korea.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download