Abstract
Purpose
The present study aimed to evaluate which of the following imaging methods best assessed misfit at the tooth-restoration interface: (1) bitewing radiographs, both conventional and digital, performed using a photostimulable phosphor plate (PSP) and a charge-coupled device (CCD) system; (2) panoramic radiographs, both conventional and digital; and (3) cone-beam computed tomography (CBCT).
Materials and Methods
Forty healthy human molars with class I cavities were selected and divided into 4 groups according to the restoration that was applied: composite resin, composite resin with liner material to simulate misfit, dental amalgam, and dental amalgam with liner material to simulate misfit. Radiography and tomography were performed using the various imaging methods, and the resulting images were analyzed by 2 calibrated radiologists. The true presence or absence of misfit corresponding to an area of radiolucency in regions subjacent to the esthetic and metal restorations was validated with microscopy. The data were analyzed using a receiver operating characteristic (ROC) curve, and the scores were compared using the Cohen kappa coefficient.
Results
For bitewing images, the digital systems (CCD and PSP) showed a higher area under the ROC curve (AUROC) for the evaluation of resin restorations, while the conventional images exhibited a larger AUROC for the evaluation of amalgam restorations. Conventional and digital panoramic radiographs did not yield good results for the evaluation of resin and amalgam restorations (P<.05). CBCT images exhibited good results for resin restorations (P>.05), but showed no discriminatory ability for amalgam restorations (P<.05).
Radiographic examinations are an important tool for diagnosing caries and developing treatment plans, as well as a highly effective method for evaluating the quality of treatment and its outcomes over the course of follow-up, thereby avoiding unnecessary restorative interventions.12 Misfit between dental hard tissue and the margins of restorations results in leakage or microleakage, which may cause secondary or recurrent caries, crestal bone loss, or periapical lesions.345 Misfit between the tooth and restoration can be detected using radiographic images.45
The radiopacity of restorative materials is considered to be highly relevant for X-ray diagnoses.6 Esthetic materials, such as composite resin and glass ionomer cement, exhibit radiopacity similar to that of dental structures (enamel and dentin), which can hinder detection of the marginal adaptation of the restorative material and the identification of recurrent carious lesions on X-ray examinations. Conversely, metal materials have high radiopacity on digital X-ray images, which often results in a high contrast with adjacent structures; thus, they tend to create image artifacts that may result in false-positive diagnoses of a lack of marginal adaptation or the presence of carious lesions.
Digital radiology exhibits numerous advantages compared with conventional radiology. However, some characteristics of image acquisition are similar, especially in terms of geometric factors, such as the classical errors of the technique, including improper positioning of the patient and/or of the X-ray tube, displacement of the equipment and/or the patient, and incorrect vertical and horizontal angles, among others, all of which interfere directly with the X-ray results. A peculiar feature of digital radiography is that it generates image noise, an artifact that can mask or simulate a clinical feature (e.g., dental materials, abnormalities, and pathological conditions).7
Digital dental radiographs are considered to be as accurate as conventional radiographs; however, the interpretation of the images is different, since digital systems provide numerous resources that allow the user to manipulate the acquired data.1 Nevertheless, a digital resource that aids in the diagnosis of one condition might not necessarily be useful for another condition and may even compromise the diagnosis. Thus, additional care must be taken when interpreting digital images to avoid potential false-positive or false-negative diagnoses.
The use of cone-beam computed tomography (CBCT) to detect carious lesions has already been investigated. CBCT provides a 3-dimensional image containing detailed information about the teeth and their supporting structures. Its use is recommended in several fields of dentistry, especially implant dentistry, dental surgery, and endodontics. According to some researchers, CBCT is excellent for detecting proximal carious lesions.8910
Previous studies have assessed the tooth-restoration interface with X-ray technology and with CBCT; however, most such studies evaluated teeth without metal restorations.91112 The present study aimed to compare digital and conventional X-ray images (bitewing and panoramic radiography) and CBCT images of tooth-restoration interfaces with metal and esthetic restorative materials, in order to evaluate which imaging method best assessed the quality of restoration treatments in a way that enabled detection of misfit at the tooth-restoration interface.
This study began after receiving approval from the local Human Research Ethics Committee (C.A.A.E. 0357. 0.213.000-11). The experimental group consisted of 40 healthy human molars that were examined under a ×4 magnifying glass to determine whether fracture lines, cracks, or carious lesions that could eventually affect the X-ray images were present. Teeth exhibiting any of the above features were discarded.
A section of the occlusal third of the crown was obtained from each selected tooth using double-faced diamond discs (KG#7020, KG Sorensen, Cotia, SP, Brazil) under refrigeration to remove the cusp tips for standardization purposes, since the thickness of the enamel along this surface varies among teeth, which can interfere with the images. Class I cavity preparations were made with dimensions of 4.5 mm in the medial-distal direction, 3.5 mm in the lingual direction, and 2.5 mm of depth in each of the 40 teeth (Fig. 1).
The prepared teeth were randomly divided into 4 groups according to the chosen restoration process (R1 and R2 for the resin group, and A1 and A2 for the amalgam group). Only two groups received a glass ionomer liner on the pulpal wall to simulate tooth-restoration misfit (the R2 and A2 groups). The R1 group was composed of 10 teeth that were restored with Filtek 350XT composite resin (3M ESPE Dental Products Division, St. Paul, MN, USA), while the R2 group was composed of 10 teeth that were restored with composite resin using the method described for the R1 group; however, the pulpal wall was pre-sealed with Vitrebond glass ionomer liner (3M ESPE Dental Products Division, St. Paul, MN, USA) according to the manufacturer's recommendations (with a thickness of approximately 0.5 mm). The A1 group was composed of 10 teeth that were restored with Dispersalloy amalgam (Dentsply Limited, Surrey, England). The A2 group was composed of 10 teeth that were restored with dental amalgam using the method described for the A1 group; however, the pulpal wall was presealed with Vitrebond glass ionomer liner (with a thickness of approximately 0.5 mm).
The teeth were inserted into an articulated dental manikin, with soft pink gingivae, in the place of the first and second molars in order to facilitate bitewing radiographic exams and to provide adequate positioning for the panoramic radiographs and CBCT images. The manikins were positioned with the aid of an acrylic box with corresponding marks to ensure adequate positioning. A 15-mm-thick acrylic plate was placed between the radiation source and the manikin to attenuate the radiation beam, simulating the patient's soft tissue (Fig. 2).121314
The Kodak 2200 Intraoral X-Ray System (Eastman Kodak Company, Rochester, NY, USA) was used for the intraoral radiographs. Kodak Insight X-ray film (Eastman Kodak, Rochester, NY, USA), size 2, was used for conventional imaging (Fig. 3A). The Kodak RVG 5100 digital sensor (Eastman Kodak Company, Rochester, NY, USA) was used for the digital charge-coupled device (CCD) system (Fig. 3B), and the Scan-X Duo system (Air Techniques, Melville, NY, USA) was used for the digital photostimulable phosphor plate (PSP) system (Fig. 3C). The manikins were positioned in a way that allowed standardized X-ray image acquisition and a source-detector distance of 40 cm was maintained. The vertical and horizontal angulations of the X-ray tube head were adjusted by 8° and 90°, respectively. The exposure conditions used were 60 kV and 7 mA, and the exposure time was chosen according to the manufacturer's recommendations for each method: 0.454 seconds for the conventional method, 0.238 seconds for the digital PSP method, and 0.143 seconds for the digital CCD method.
An Orthophos 3C X-ray device (Sirona Dental Systems, Bensheim, Germany) and Kodak T-MAT G/RA extraoral X-ray film (Eastman Kodak, Rochester, NY, USA) were used for conventional panoramic radiography (Fig. 3D), while the Kodak 9000C 3D X-ray device (Eastman Kodak, Rochester, NY, USA) was used for digital panoramic radiography (Fig. 3E) and CBCT (Fig. 3F). The manikins were positioned with the aid of an acrylic box to ensure adequate positioning in the focal trough for panoramic radiography and within the field of vision (FOV) for CBCT. The exposure conditions were 60 kV and 10 mA for the conventional method, 60 kV and 2 mA for the digital method, and 60 kV and 10 mA for CBCT, with an exposure time of 10.8 seconds, scanning at a collimation (FOV) of 5.0 cm×3.7 cm and an isotropic voxel thickness of 76×76×76 µm.
Two oral radiologists, after having been duly trained and calibrated, independently and blindly evaluated all the X-ray and tomographic images.
An LED negatoscope was used for the interpretation of conventional radiographs. The interpretation of digital and tomographic images was performed directly in the Kodak Dental Imaging Software (KDIS; Kodak Dental Systems, Rochester, NY, USA). The radiographic images and CBCT images (Fig. 4) were interpreted randomly at 2 different times. The classification was performed on a 5-grade scale: 1, definitely exhibits misfit; 2, probably exhibits misfit; 3, uncertain; 4, probably does not exhibit misfit; 5, definitely does not exhibit misfit.
To validate the X-ray diagnosis (the true absence or presence of glass ionomer liner corresponding to a radiolucent area in regions subjacent to the esthetic and metal restorations), the teeth were sectioned along their axis in the mesial-distal direction with a steel disc. Images were captured under a Zeiss Axio Imager A1 light microscope (Carl Zeiss Ltd., Göttingen, Germany) with a coupled camera, using no dyes, at ×50 magnification (Fig. 5).
The Cohen kappa (linear weighted kappa values) was calculated to assess the levels of intraexaminer and interexaminer agreement.15 The area under the receiver operating characteristic (ROC) curve (AUROC) was calculated using BioEstat 5.0 software (Instituto de Desenvolvimento Sustentável Mamirauá, Belém, Brazil) for each type of image, and the results were compared using the Cochran Q test at a significance level of P<.05. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated for each imaging method. A score of 1 or 2 was considered positive.
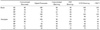
Table 1 summarizes the results of intraexaminer and interexaminer agreement for the methods assessed in this study. A moderate level of intraexaminer agreement was obtained for 1 examiner's analysis of the CBCT results. Excellent and good levels of intraexaminer agreement were obtained for the conventional and digital panoramic and bitewing radiographs. Notably, moderate interexaminer agreement was obtained for the digital panoramic radiographs, whereas the other 5 imaging methods exhibited good levels of agreement.
The AUROC values of each X-ray image acquisition modality for metal and esthetic restorative materials are shown in Figures 6 and 7, as well as in Table 2. The digital systems (CCD and PSP bitewing) had a higher AUROC for the evaluation of resin restorations than the conventional bitewing images. However, the conventional bitewing images exhibited a higher AUROC for assessing amalgam restorations. The digital CCD bitewing images exhibited a rightward-shifted curve in the evaluation of the amalgam restorations in comparison to the conventional and digital PSP bitewing images, although the curve reached high values (high false-positive rates). The 3 bitewing imaging methods (conventional, CCD, and PSP) demonstrated no statistically significant difference from the real condition (P>.05).
A comparison of conventional and digital panoramic radiographs did not yield good results for the evaluation of resin and amalgam restorations. For the resin restorations, both imaging methods exhibited curves that were strongly rightward-shifted despite having high values (high sensitivity and low specificity; i.e., high false-positive rates). For the amalgam restorations, the conventional panoramic radiographs exhibited a higher AUROC, whereas the AUROC of the digital panoramic radiographs was null, meaning that the extraoral method possessed no discriminatory ability for detecting the quality of the tooth-restoration interface (Fig. 6).
The CBCT images showed good results for resin restorations, with a ROC curve that reached very high values and was shifted leftward. However, CBCT showed no discriminatory ability for the evaluation of amalgam restorations (Fig. 7).
Table 2 presents a comparative analysis of the imaging methods. The images obtained by panoramic radiography (conventional and digital) and CBCT exhibited a statistically significant difference from the real condition (P<.05) for resin and/or amalgam restorations. This result shows that panoramic radiography (conventional and digital) provided insufficient information for the evaluation of regions subjacent to the esthetic (resin) and metal (amalgam) restorations. The tomographic imaging systems provided insufficient information only for the evaluation of regions subjacent to metal (amalgam) restorations (P<.05).
To better understand these results, several performance parameters were calculated (sensitivity, specificity, positive predictive value, negative predictive value, and accuracy) for the evaluations of resin and amalgam restorations using the tested imaging methods (Table 3). The best results for evaluating the resin restorations were obtained with CBCT, and the best results for evaluating the amalgam restorations were obtained with conventional bitewing radiography.
The radiographic detection of restoration interfaces is important in order to avoid secondary caries, crestal bone loss, or periapical lesions due to leakage or microleakage.345 Previous studies have assessed the quality of the tooth-restoration interface with conventional and digital X-ray technology, with intraoral and extraoral examinations, and with CBCT; however, most of those studies evaluated teeth without metal restorations.91112 Therefore, the present study tested and compared which dental X-ray imaging method better assessed misfit of the tooth-restoration interface in teeth with resin and metal restorations, with the ultimate goal of avoiding tooth damage.
The advent of digital radiology revolutionized the field of radiology by enabling digital sensors to be used instead of conventional X-ray film. The main advantages of digital X-ray technology are the reduction in the radiation dose and the increased image quality. However, a peculiar feature of digital radiography is the generation of noise in the image, which refers to an artifact that can mask or simulate a clinical factor (e.g., dental materials, abnormalities, and pathological conditions),7 and awareness of patterns of noise generation is essential for adequate X-ray diagnosis.1617 An artifact known as the halation or Uber-schwinger artifact is formed when there are great differences in the density of adjacent structures, and it appears as a radiolucent band parallel to the higher-density interface.17 This artifact may also simulate carious lesions, making it a challenge when developing a differential diagnosis.
The results obtained in the present study are in agreement with those of previous studies regarding intraoral radiographs.891218 Although the intraoral methods that those authors used differed from the method used in the present study, it can be said that, in vitro, the results of periapical radiography were the same as the results of the bitewing radiographs used in the present study. More specifically, the principle of image generation is the same; that is, the image detector and the objects are parallel to each other, and the central radiation beam is perpendicular to them.8 As Table 2 shows, the AUROC values for the evaluations of bitewing radiographs (conventional, PSP, and CCD) exhibited no statistically significant differences from the real condition; therefore, this technique can be considered adequate.
Some studies evaluated the diagnosis of dental caries using CBCT images and found equivalent diagnostic performance to conventional and digital radiography.89121819 However, the results obtained with CBCT in the present study disagree with those findings. Most previous studies validated CBCT using only teeth that were free of restorative materials (generally healthy teeth or teeth with small cavities or caries), unlike the present study. According to Hassan et al.,20 tomographic examinations are more sensitive than periapical radiographs for detecting fractures because of the 3-dimensional nature of CBCT. However, CBCT has a lower specificity, since hyperdense materials can create sunbeam-like artifacts on CBCT that imitate fracture lines, thus limiting its diagnostic ability. Similarly, this study showed that the formation of artifacts inherent to the CBCT technique varied according to the density of the restorative material, since CBCT exhibited good results in the evaluation of composite resin but a high number of false positives in the evaluation of the tooth-restoration interface in metal restorations, thus indicating its poor accuracy. The higher radiation dose of CBCT than that of intraoral and panoramic radiography is another limiting factor.2122
The same trend could be observed in the results from panoramic radiographs, as observed in Figure 4. More specifically, digital panoramic radiography exhibited a null AUROC for the metal restorations, whereas the ROC curve for the resin restorations presented a strong rightward shift despite having high values (i.e., it exhibited high sensitivity and low specificity). This result agrees with that of Kamburoğlu et al.,21 who compared the accuracy of intraoral and extraoral bitewing radiographs and panoramic radiographs and concluded that the intraoral bitewing radiographs presented the best results. Furthermore, neither digital nor conventional panoramic radiographs provide the necessary sharpness, most likely due to the detector-object distance and the negative angle in relation to the object of radiographic interest.
Conventional bitewing radiographs had the highest AUROC value, followed by digital PSP bitewing and digital CCD bitewing radiographs (Table 2). This finding is probably due to the fact that conventional bitewing radiographs generate no artifact with respect to contrast between structures with different densities. Moreover, the digital images showed visible artifact reduction when compared to the panoramic radiographs, most likely because of the proximity of the detector to the radiographed object, as well as the high spatial resolution of the tested systems. CCD has a spatial resolution of 14 line pairs per millimeter (lp/mm) and PSP has a resolution of 7 lp/mm, whereas conventional X-ray film exhibits the highest spatial resolution (≥20 lp/mm).232425
In conclusion, panoramic (conventional and digital) radiographs exhibited a statistically significant difference from the real condition for the amalgam and resin restorations, while CBCT images exhibited a statistically significant difference from the real condition only for amalgam restorations, indicating that these imaging systems provided insufficient information to assess the regions subjacent to esthetic and/or metal restorations. Furthermore, CBCT is not a viable method because of its radiation dose. To summarize, the best results for evaluating misfit in both esthetic and metal dental restorations were obtained with conventional, digital PSP, and digital CCD bitewing radiographs. This finding indicates that bitewing radiographs (conventional or digital) should be the method of choice to detect misfit at the tooth-restoration (metal or resin) interface and for subsequent follow-up.
Figures and Tables
Fig. 1
Tooth preparation. A. Selected tooth. B. Coronal section. C. Occlusal surface flattening. D. Finished class I cavity. E. Composite resin restoration. F. Amalgam restoration.

Fig. 2
A and B. Manikin positioned in an acrylic box, with a 15-mm-thick acrylic plate put in place in order to simulate the soft tissue.

Fig. 3
Image acquisition with different imaging methods. A. Conventional bitewing. B. Digital charge-coupled device (CCD) bitewing. C. Digital photostimulable phosphor plate (PSP), interproximal radiograph. D. Conventional panoramic radiograph. E. Digital panoramic radiograph. F. Cone-beam computed tomograph (CBCT).

Fig. 4
X-ray and tomographic images. A. Digital charge-coupled device (CCD) bitewing. B. Digital photostimulable phosphor plate (PSP) bitewing. C. Conventional bitewing. D. Conventional panoramic radiograph. E. Digital panoramic radiograph. F. Cone-beam computed tomography (CBCT).

Fig. 5
Histological sections. A. Tooth from the R1 group (composite resin restoration). B. Tooth from the R2 group (composite resin restoration with liner material). C. Tooth from the A1 group (dental amalgam restoration). D. Tooth from the A2 group (dental amalgam restoration with liner material).

Fig. 6
The receiver operating characteristic (ROC) curves for the evaluation of resin and amalgam restoration images obtained using various imaging methods. A. Conventional bitewing. B. digital photostimulable phosphor plate (PSP) bitewing. C. digital charge-coupled device (CCD) bitewing. D. Digital panoramic radiography. E. Conventional panoramic radiography.

Fig. 7
Receiver operating characteristic (ROC) curve of cone-beam computed tomography (CBCT) images for the evaluation of resin (A) and amalgam (B) restorations.

Table 1
Intra- and inter-examiner agreement values obtained for imaging methods using weighted Kappa coefficients.

Table 2
Comparative analysis of imaging methods for resin and amalgam restorations using receiver operating characteristic (ROC) curve areas.

References
1. Schweitzer DM, Berg RW. A digital radiographic artifact: a clinical report. J Prosthet Dent. 2010; 103:326–329.

2. Mitropoulos P, Rahiotis C, Stamatakis H, Kakaboura A. Diagnostic performance of the visual caries classification system ICDAS II versus radiography and micro-computed tomography for proximal caries detection: an in vitro study. J Dent. 2010; 38:859–867.

3. Papageorgiou SN, Papadelli AP, Koidis PT, Petridis HP. The effect of prosthetic margin location on caries susceptibility. A systematic review and meta-analysis. Br Dent J. 2013; 214:617–624.

4. Liedke GS, Spin-Neto R, Vizzotto MB, Da Silveira PF, Silveira HE, Wenzel A. Diagnostic accuracy of conventional and digital radiography for detecting misfit between the tooth and restoration in metal-restored teeth. J Prosthet Dent. 2015; 113:39–47.
5. Liedke GS, Spin-Neto R, da Silveira HE, Wenzel A. Radiographic diagnosis of dental restoration misfit: a systematic review. J Oral Rehabil. 2014; 41:957–967.

6. Salzedas LM, Louzada MJ, de Oliveira Filho AB. Radiopacity of restorative materials using digital images. J Appl Oral Sci. 2006; 14:147–152.

7. Olsson L, Nilsson M, Svenson B, Hellén-Halme K. The effect of anatomical noise on perception of low contrast in intra-oral radiographs: an in vitro study. Dentomaxillofac Radiol. 2016; 45:20150402.
8. Belém MD, Tabchoury CP, Ferreira-Santos RI, Groppo FC, Haiter-Neto F. Performance of a photostimulable storage phosphor digital system with or without the sharpen filter and cone beam CT for detecting approximal enamel subsurface demineralization. Dentomaxillofac Radiol. 2013; 42:20120313.

9. Kamburoğlu K, Kurt H, Kolsuz E, Öztaş B, Tatar I, Çelik HH. Occlusal caries depth measurements obtained by five different imaging modalities. J Digit Imaging. 2011; 24:804–813.

10. Wenzel A, Hirsch E, Christensen J, Matzen LH, Scaf G, Frydenberg M. Detection of cavitated approximal surfaces using cone beam CT and intraoral receptors. Dentomaxillofac Radiol. 2013; 42:39458105.

11. Liedke GS, Spin-Neto R, Vizzotto MB, da Silveira PF, Wenzel A, da Silveira HE. Diagnostic accuracy of cone beam computed tomography sections with various thicknesses for detecting misfit between the tooth and restoration in metal-restored teeth. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 120:e131–e137.

12. Valizadeh S, Tavakkoli MA, Karimi Vasigh H, Azizi Z, Zarrabian T. Evaluation of cone beam computed tomography (CBCT) system: comparison with intraoral periapical radiography in proximal caries detection. J Dent Res Dent Clin Dent Prospects. 2012; 6:1–5.
13. Soğur E, Baksi BG, Gröndahl HG. Imaging of root canal fillings: a comparison of subjective image quality between limited cone-beam CT, storage phosphor and film radiography. Int Endod J. 2007; 40:179–185.

14. Caldas Mde P, Ramos-Perez FM, de Almeida SM, Haiter-Neto F. Comparative evaluation among different materials to replace soft tissue in oral radiology studies. J Appl Oral Sci. 2010; 18:264–267.
15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.

16. Solomon SL, Jost RG, Glazer HS, Sagel SS, Anderson DJ, Molina PL. Artifacts in computed radiography. AJR Am J Roentgenol. 1991; 157:181–185.

17. Tan TH, Boothroyd AE. Uberschwinger artefact in computed radiographs. Br J Radiol. 1997; 70:431.

18. Haiter-Neto F, dos Anjos Pontual A, Frydenberg M, Wenzel A. Detection of non-cavitated approximal caries lesions in digital images from seven solid-state receptors with particular focus on task-specific enhancement filters. An ex vivo study in human teeth. Clin Oral Investig. 2008; 12:217–223.

19. Murat S, Kamburoğlu K, Isayev A, Kurşun S, Yüksel S. Visibility of artificial buccal recurrent caries under restorations using different radiographic techniques. Oper Dent. 2013; 38:197–207.

20. Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009; 35:719–722.

21. Kamburoğlu K, Kolsuz E, Murat S, Yüksel S, Özen T. Proximal caries detection accuracy using intraoral bitewing radiography, extraoral bitewing radiography and panoramic radiography. Dentomaxillofac Radiol. 2012; 41:450–459.

22. Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006; 35:219–226.

23. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 6th ed. St. Louis: Mosby;2009.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download