Abstract
Synovial chondromatosis is a rare metaplastic disease affecting the joints, including the temporomandibular joint (TMJ). Since its symptoms are similar to those of temporomandibular disorders, a careful differential diagnosis is essential. A 50-year-old male patient was referred with the chief complaint of pain and radiopaque masses around the left TMJ on panoramic radiography. Clinically, pre-auricular swelling and resting pain was found, without limitation of mouth opening. On cone-beam computed tomographic images, multiple calcified nodules adjacent to the TMJ and bone proliferation with sclerosis at the articular fossa and eminence were found. T2-weighted magnetic resonance images showed multiple signal-void nodules with high signal effusion in the superior joint space and thickened cortical bone at the articular fossa and eminence. The calcified nodules were removed by surgical excision, but the hypertrophic articular fossa and eminence remained. A histopathological examination confirmed the diagnosis. The patient was followed up few months later without recurrence.
Synovial chondromatosis of the temporomandibular joint (TMJ) is a rare, benign, metaplastic disease characterized by the formation of numerous cartilaginous nodules within the synovial membranes. These nodules eventually are detached and are seen as loose bodies floating in the joint space in radiographic images.1 The etiology has not yet been clarified.2
The symptoms include pre-auricular pain and swelling, limitations of mouth opening and condylar movement, joint sound and pain,3 myalgia of the masticatory muscles, and malocclusion,45 which are quite similar to those of temporomandibular disorder (TMD), making the clinical differential diagnosis difficult.6 Therefore, the diagnosis is made based mostly on images, including plain radiography, cone-beam computed tomography (CBCT), and magnetic resonance (MR) imaging,27 supplemented by an assessment of the clinical symptoms. The radiographic image findings are numerous calcified loose bodies surrounding the mandibular condyle,235678910 degenerative changes of the condyle,38 sclerosis of the glenoid fossa and condyle,7 and rarely, extension into the middle cranial fossa due to excessive bone resorption at the glenoid fossa.78 In MR images, loose bodies with a low and heterogeneous signal within high-signal articular space effusion and expansion in T2-weighted images are characteristic findings.237811
The loose bodies and metaplastic synovial membrane tissue are usually removed by surgical excision.27 Arthroscopy can be used for visualization and minimally invasive interventions.59 The recurrence rate is very low,2 according to Liu et al.,7 who reported only 3 instances of recurrence out of 119 total cases.
This report presents the various imaging features of synovial chondromatosis of the TMJ with abundant loose bodies, as well as hypertrophy and sclerosis of the temporal bone, which is an uncommon feature that few reports have described.710
A 50-year-old male patient was referred to the Department of Oral and Maxillofacial Surgery at Dankook University Dental Hospital from a private dental clinic, with the chief complaint of pain at his left TMJ and numerous radiopaque masses around the left TMJ on panoramic radiography. The patient showed spontaneous and opening pain and swelling at the left TMJ, but showed no tenderness or limitation of mouth opening.
On panoramic imaging (Fig. 1), large, abundant loose bodies around the left TMJ were observed, and flat hypertrophy of the articular eminence was suspected. CBCT (Alphard VEGA, Asahi Roentgen Ind. Co., Kyoto, Japan) was performed, and the resulting images (Figs. 2,3,4) revealed numerous radiopaque loose bodies of various shapes and sizes surrounding the left condyle. The shape of the condyle was within normal limits, but hypertrophy with sclerotic changes was observed on the anterior and lateral sides of the temporal bone, the articular eminence, and the articular fossa.
For further confirmation of the imaging diagnosis, MR imaging (Ingenia 3.0T, Philips Healthcare, Amsterdam, Netherlands) was performed. On the T1-weighted MR images (Fig. 5), the small and large loose bodies showed low signal intensity in the superior joint space around the left condyle. On T1-weighted fat-suppressed MR images with contrast enhancement (Fig. 6), enhancement of the peripheral wall was observed, indicating hypertrophy of the synovial membrane. Moreover, the T2-weighted MR images (Fig. 7) showed low-signal loose bodies within high-signal synovial effusion. On the sagittal MR images mentioned above, hypertrophy of the articular eminence and loose bodies were observed as low-signal-intensity masses, especially on the T2-weighted MR images (Fig. 7A). Considering the above image findings, the impression of synovial chondromatosis was made.
The loose bodies were removed through surgical excision under general anesthesia, and approximately 120 pieces were removed. The diagnosis of synovial chondromatosis was confirmed by a histopathologic examination. On the low-magnification images, many small ovoid loose bodies with focal calcifications were found (Fig. 8A). Higher magnification of a loose body showed vague lobules of hyaline cartilage enclosed by a thin layer of attenuated synovial cells (Fig. 8B).
A postoperative panoramic image was taken and remaining flat hypertrophy of the articular eminence was observed, without any loose bodies (Fig. 9). The patient's symptoms were relieved, and no signs of recurrence were observed at 1-month and 3-month follow-up visits.
The typically reported radiographic image findings of synovial chondromatosis are calcified loose bodies around the mandibular condyle and degenerative changes of the condyle.235678910 Some previous studies reported several pathologic changes in the temporal bone associated with synovial chondromatosis. Yu et al.10 reported bone resorption at the glenoid fossa and articular eminence, as well as sclerosis of the articular eminence. Liu et al.7 reported sclerosis and hyperplasia of the condyle and glenoid fossa. In this report, the sclerosis and hyperplasia of the articular eminence were more extensive and prominent, along with an excessive number of loose bodies. The hyperplastic mass at the articular eminence was more planar with a distinct outer border. It could be speculated that cartilaginous loose bodies might have stuck to the articular eminence, but its composition is unknown because the mass was not excised, and therefore no histopathologic examination was performed.
Synovial chondromatosis and degenerative joint disease of the TMJ share many clinical symptoms, such as joint sounds and pain, myalgia in the masticatory muscles, and malocclusion.456 Therefore, the differential diagnosis between these 2 diseases is made based on imaging features. Synovial chondromatosis arises more often at the superior joint cavity,26 usually involves rounder loose bodies, and often shows a mandibular condyle with normal shape, as well as expansion and effusion of the joint cavity.2348 In contrast, degenerative joint disease arises more often at the inferior joint cavity, involves angular loose bodies, and often shows obvious degenerative changes of the mandibular condyle, sometimes with osteophytes in the anterior portion. The reason why the loose bodies formed in synovial chondromatosis and degenerative joint disease have different shapes lies in their sources. While the loose bodies in the former condition occur due to metaplastic changes of the synovial membrane, those in the latter condition result from detached sharp osteophytes due to degenerative changes of the mandibular condyle. The usual modalities for the differential diagnosis are plain radiographs, CBCT, and MR imaging.2 However, detection of loose bodies without calcification can hardly be done with routine imaging. For indirect visualization of non- or less-calcified loose bodies, Matsumoto et al.6 suggested arthrography
Although the etiology of synovial chondromatosis has not yet been elucidated, researchers have suggested subdividing the disease into primary and secondary synovial chondromatosis.2312 Primary chondromatosis has been reported to be caused by metaplastic changes and cartilaginous foci formation in the synovial membrane and calcification of the cartilaginous bodies. In contrast, secondary chondromatosis, as suggested by the name, develops following trauma or arthropathies, including degenerative changes. Fragments dislodged from the joint move freely within the synovial fluid and are nourished by it. Thus, some histologic findings differ between the 2 types of synovial chondromatosis. While primary synovial chondromatosis involves a patchy and diffuse pattern of calcification, secondary synovial chondromatosis shows ring-like calcifications.12
Many imaging features of synovial chondromatosis have been reported. However, no reports have described extensive sclerosis and hyperplasia of the temporal bone, as observed in this case. Clinicians should acknowledge the various imaging features of synovial chondromatosis in order to make an accurate diagnosis and to provide timely and adequate treatment.
Figures and Tables
 | Fig. 1Preoperative panoramic image shows loose bodies of various shapes and sizes around the left mandibular condyle, leading to the suspicion of flat hypertrophy of the articular eminence. |
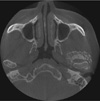 | Fig. 2An axial cone-beam computed tomographic image shows numerous, pebble-like loose bodies surrounding the condyle in all directions except for the medial-posterior side. A large, crescent-shaped, loose body is also seen anterior to the condyle. |
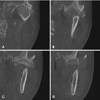 | Fig. 3Coronal oblique cone-beam computed tomographic (CBCT) images. A. Loose bodies are seen on the superior and lateral sides of the condyle. Sclerosis and hypertrophy of the glenoid fossa are also seen. B–D. CBCT images anterior to the condyle. B. Loose bodies are seen on the medial and lateral sides. Sclerosis and hypertrophy of the articular eminence are also prominent on the lateral side. C. A large, elliptical loose body among several small loose bodies is seen on the medial and lateral sides. Sclerosis and hypertrophy of the articular eminence are also prominent on both the medial and lateral sides. D. The hypertrophic mass of the articular eminence is seen to be partially detached and sclerosis of the articular eminence is still evident. Small loose bodies are seen inferior to the mass. |
 | Fig. 4Sagittal cone-beam computed tomographic (CBCT) images. A. A partially detached hypertrophic mass is seen at the anterior slope of the articular eminence. A large loose body is also seen at the posterior side of the condyle, among several small loose bodies. B and C. A large loose body is seen on the anterior side of the condyle. The hypertrophic mass is still seen at the anterior slope of the articular eminence. D. A CBCT image lateral to the condyle shows the partially detached hypertrophic mass at the articular eminence and loose bodies inferior to the mass. |
 | Fig. 5T1-weighted magnetic resonance images in the closed position. A. A sagittal image at the medial half of the condyle shows loose bodies and the hypertrophic mass as low-signal intensity masses anterior to the condyle and the articular eminence, respectively. B. A coronal image at the anterior side of the condyle shows loose bodies as low-signal intensity masses inferior to the temporal bone and the zygomatic bone, spread across the medial and lateral sides. |
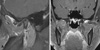 | Fig. 6T1-weighted, fat-suppressed magnetic resonance images with contrast enhancement in the closed position. A. A sagittal image at the medial half of the condyle shows the low-signal intensity hypertrophic mass at the anterior slope of the articular eminence, as well as loose bodies surrounded by a high-signal-intensity peripheral wall, corresponding to the synovial membrane. B. A coronal image at the anterior side of the condyle shows low-signal-intensity loose bodies inferior to the temporal bone and the zygomatic bone, surrounded by a high-signal-intensity peripheral wall. |
 | Fig. 7T2-weighted magnetic resonance images in the closed position. A. A sagittal image at the medial half of the condyle prominently shows a low-signal-intensity hypertrophic mass at the anterior slope of the articular eminence, as well as loose bodies in the high-signal-intensity effusion. B. A coronal image at the anterior side of the condyle shows low-signal-intensity loose bodies inferior to the temporal bone and the zygomatic bone, in the high-signal-intensity effusion. |
 | Fig. 8A. A low-power view exhibits many small ovoid loose bodies with focal calcification (H&E stain, original magnification ×12.5). B. Higher magnification of the loose body showing vague lobules of hyaline cartilage enclosed by a thin layer of attenuated synovial cells (H&E stain, original magnification ×100). |
References
1. Schulte WC, Rhyne RR. Synovial chondromatosis of temporomandibular joint. Report of a case. Oral Surg Oral Med Oral Pathol. 1969; 28:906–913.
2. Tamimi D, Hatcher D. Specialty imaging. Temporomandibular joint. Philadelphia, PA: Elsevier;2016. p. 530–533.
3. Testaverde L, Perrone A, Caporali L, Ermini A, Izzo L, D'Angeli I, et al. CT and MR findings in synovial chondromatosis of the temporo-mandibular joint: our experience and review of literature. Eur J Radiol. 2011; 78:414–418.

4. Ida M, Yoshitake H, Okoch K, Tetsumura A, Ohbayashi N, Amagasa T, et al. An investigation of magnetic resonance imaging features in 14 patients with synovial chondromatosis of the temporomandibular joint. Dentomaxillofac Radiol. 2008; 37:213–219.

5. von Lindern JJ, Theuerkauf I, Niederhagen B, Bergé S, Appel T, Reich RH. Synovial chondromatosis of the temporomandibular joint: clinical, diagnostic, and histomorphologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:31–38.

6. Matsumoto K, Sato T, Iwanari S, Kameoka S, Oki H, Komiyama K, et al. The use of arthrography in the diagnosis of temporomandibular joint synovial chondromatosis. Dentomaxillofac Radiol. 2013; 42:15388284.

7. Liu X, Huang Z, Zhu W, Liang P, Tao Q. Clinical and imaging findings of temporomandibular joint synovial chondromatosis: an analysis of 10 cases and literature review. J Oral Maxillofac Surg. 2016; 74:2159–2168.

8. Meng J, Guo C, Yi B, Zhao Y, Luo H, Ma X. Clinical and radiologic findings of synovial chondromatosis affecting the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:441–448.

9. Lim SW, Jeon SJ, Choi SS, Choi KH. Synovial chondromatosis in the temporomandibular joint: a case with typical imaging features and pathological findings. Br J Radiol. 2011; 84:e213–e216.

10. Yu Q, Yang J, Wang P, Shi H, Luo J. CT features of synovial chondromatosis in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:524–528.

11. Wang P, Tian Z, Yang J, Yu Q. Synovial chondromatosis of the temporomandibular joint: MRI findings with pathological comparison. Dentomaxillofac Radiol. 2012; 41:110–116.

12. Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol. 1979; 10:439–451.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download