Abstract
Multiple autoimmune syndrome (MAS) is a rare condition, in which at least three well-defined autoimmune diseases co-occur in a single patient. Although the pathogenesis of MAS remains poorly understood, genetic, immunological, hormonal, and environmental factors may all play a role. Although three classic subtypes of MAS are well known, several cases that could not be placed into any of these three categories have recently been reported. To the best of our knowledge, the co-existence of psoriasis, vitiligo, and Crohn's disease has been reported in only one patient, who had a total of five autoimmune diseases (alopecia areata and oral lichen planus in addition to the three conditions mentioned). We herein describe a rare case of MAS presenting with psoriasis, vitiligo, and Crohn's disease, and suggest that tumor necrosis factor-α may be associated with the pathogenesis of all three conditions.
Multiple autoimmune syndrome (MAS) refers to a combination of at least three autoimmune diseases in the same patient1. Although many investigators have suggested associations among autoimmune diseases, the co-existence of several diseases in a single patient has only occasionally been reported2. Of the several cases of MAS reported to date, the co-existence of psoriasis, vitiligo, and Crohn's disease in a single patient is very rare. We report a case of MAS in a 17-year-old woman presenting with psoriasis, vitiligo, and Crohn's disease. We suggest that this is a unique MAS variant in which the pathogenetic presentations may have genetic susceptibilities and immunological features in common.
A 17-year-old woman presented with hypopigmented skin patches and scaly plaques that initially appeared 10 years prior, but had developed further and coalesced more recently. On physical examination, multiple, well-demarcated depigmented patches were evident on the trunk (Fig. 1A, B) as were scaly hyperkeratotic plaques on the scalp and both elbows (Fig. 1C). She did not report any systemic symptoms during the examination. Six years prior, the patient had presented at our clinic with the same skin problems. At that time, we had biopsied a hyperkeratotic scalp lesion (Fig. 2) and diagnosed psoriasis (Fig. 3). Wood's lamp examination was used to diagnose the hypopigmented trunk patches as vitiligo. However, the patient was lost to follow-up and did not undergo any treatment. Iron deficiency anemia was found on laboratory testing, but all other test results were within the normal ranges. No finding suggestive of any type of connective tissue or rheumatic disease was evident. The patient had no relevant familial history.
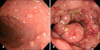
Surprisingly, during her recent visit, the patient reported that she had been newly diagnosed with Crohn's disease the year before and that the psoriasis and vitiligo of her skin had become more severe, and spread, after repeated treatment for Crohn's disease with anti-tumor necrosis factor-α (TNF-α; infliximab). She underwent computed tomography, magnetic resonance imaging (MRI), and endoscopic examination because of long-standing diarrhea, intermittent bloody stools, and abdominal pain. An endoscopic examination revealed several linear aphthous ulcers (Fig. 4A) and a hemorrhagic colonic mucosa with a cobblestone-like appearance (Fig. 4B). Rectal MRI also revealed a peri-anal fistula. The patient is currently undergoing excimer laser therapy to treat her vitiligo and psoriasis and is also receiving treatment for Crohn's disease.
Autoimmune diseases are a heterogeneous group of disorders associated with loss of immunological tolerance to self-antigens, in turn triggering the production of auto-antibodies that inflame or damage target tissues and organs34. It has been reported that patients with a single autoimmune disease are at a higher risk of acquiring other autoimmune diseases than are those lacking any prior autoimmune disease25.
MAS, first described by Humbert and Dupond6 in 1988, is a rare condition, in which at least three well-defined autoimmune diseases co-exist in a single patient3. MAS is usually classified into three subtypes in terms of the nature of the co-occurring diseases12. Type 1 MAS features myasthenia gravis (MG), thymoma, dermatopolymyositis, and/or autoimmune myocarditis. Type 2 MAS features Sjőgren's syndrome (SS), rheumatoid arthritis, primary biliary cirrhosis, systemic sclerosis, and/or autoimmune thyroid disease (AITD). Type 3 MAS features AITD, MG, thymoma, SS, pernicious anemia, idiopathic thrombocytopenic purpura, Addison's disease, type 1 diabetes, vitiligo, autoimmune hemolytic anemia, and/or systemic lupus erythematosus. However, several cases that did not fit into any of these three categories have been reported recently278. Most such patients had at least one dermatological autoimmune disease, such as vitiligo, pemphigus vulgaris, bullous pemphigoid, and/or scleroderma.
Although the pathogenesis of MAS remains poorly understood, genetic, immunological, hormonal, and environmental factors may all play a role89. Many reports have suggested that environmental factors, such as tobacco use, Epstein-Barr virus, and cytomegalovirus may trigger certain clinical autoimmune phenotypes in genetically susceptible patients5710. Several polymorphic genes, including human leukocyte antigen-D related B1, TNF, and protein tyrosine phosphatase, non-receptor type 22, and certain other alleles, have recently been reported to play roles in the acquisition of autoimmune diseases511. In addition, certain chromosomal loci that may bear genes relevant to MAS have been identified3. However, no common pathogenesis is yet apparent and not all patients with autoimmune diseases share identical genetic susceptibilities.
Our current case had psoriasis, vitiligo and Crohn's disease. To the best of our knowledge, the co-existence of these three autoimmune diseases has previously been reported in only one patient with vitiligo, alopecia areata, Crohn's disease, psoriasis vulgaris, and oral lichen planus12. Although our patient lacked any recognized subtype of MAS, it is interesting to note that the three diseases are known to be interconnected in certain ways. A relationship between inflammatory bowel disease (IBD) and psoriasis has frequently been suggested. The conditions share certain pathogenic features, including T-helper (Th)1/Th17 cell-mediated inflammatory reactions and the production of cytokines, including TNF-α, interleukin (IL)-23, and IL-1713. In addition, patients with these conditions have been reported to share a genetic susceptibility associated with an IL-23 receptor gene polymorphism1415. However, any association between IBD and vitiligo remains controversial, although two cases of vitiligo have been reported in IBD patients treated with a TNF-α inhibitor; this suggests that the diseases may share a pathogenic mechanism involving TNF-α-associated inflammation1617. In terms of the relationship between vitiligo and psoriasis, the diseases are considered to share a pathogenetic feature, i.e., enhanced TNF-α levels in skin lesions, although the general relationship between the diseases remains poorly understood1819. Interestingly, several cases of psoriasis, as well as vitiligo induced or exacerbated by TNF-α inhibitors, have been reported917. Although the pathogenetic mechanisms of these paradoxical phenomena have not been fully determined, increased levels of interferon-α, which also plays a role in both psoriasis and vitiligo, was assumed to be involved as interferon-α is known to be negatively regulated by TNF9.
Herein, we report a rare case of MAS who presented with psoriasis, vitiligo, and Crohn's disease. We could not find any definite interrelationship among these diseases. However, it is possible that TNF-α plays a role in the pathogenesis of all three conditions. In addition, our patient complained that psoriasis and vitiligo of her skin became more severe and diffuse after treatment for Crohn's disease with anti-TNF-α (infliximab), further suggesting that TNF-α may be associated with all three diseases. However, patients with multiple autoimmune conditions tend to develop additional autoimmune diseases and thus require continuing surveillance. Therefore, whether these diseases share a common pathogenesis, and whether there are common genetic susceptibilities or precipitating factors, should be studied further.
Figures and Tables
Fig. 1
(A) Multiple hypopigmented patches on the chest that developed gradually but had recently coalesced. (B) A newly developed, well-demarcated hypopigmented patch on the abdomen. (C) Hyperkeratotic plaques on both elbows.

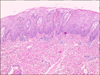
Fig. 3
A scalp skin biopsy revealed parakeratosis and regular acanthosis, with elongated and clubbed rete ridges. Suprapapillary thinning of the epidermis, and dilation of the capillaries of the dermal papillae were observed. Perivascular lymphocyte infiltration in the upper dermis was apparent (H&E, ×100).
References
1. Humbert P, Dupond JL, Vuitton D, Agache P. Dermatological autoimmune diseases and the multiple autoimmune syndromes. Acta Derm Venereol Suppl (Stockh). 1989; 148:1–8.
2. Masood S, Sajid S, Jafferani A, Tabassum S, Ansar S. Multiple autoimmune syndromes associated with psoriasis: a rare clinical presentation. Oman Med J. 2014; 29:130–131.

3. Anaya JM, Castiblanco J, Rojas-Villarraga A, Pineda-Tamayo R, Levy RA, Gómez-Puerta J, et al. The multiple autoimmune syndromes. A clue for the autoimmune tautology. Clin Rev Allergy Immunol. 2012; 43:256–264.

4. Wilson JC, Furlano RI, Jick SS, Meier CR. Inflammatory bowel disease and the risk of autoimmune diseases. J Crohns Colitis. 2016; 10:186–193.

5. Cojocaru M, Cojocaru IM, Silosi I. Multiple autoimmune syndrome. Maedica (Buchar). 2010; 5:132–134.
6. Humbert P, Dupond JL. Multiple autoimmune syndromes. Ann Med Interne (Paris). 1988; 139:159–168.
7. Pasić A, Ljubojević S, Lipozencić J, Marinović B, Loncarić D. Coexistence of psoriasis vulgaris, bullous pemphigoid and vitiligo: a case report. J Eur Acad Dermatol Venereol. 2002; 16:426–427.

8. Topal F, Senel E, Akbulut S, Topal F, Dölek Y. A new combination of multiple autoimmune syndrome? Coexistence of vitiligo, autoimmune thyroid disease and ulcerative colitis. Dermatol Reports. 2011; 3:e19.

9. Barthel C, Biedermann L, Frei P, Vavricka SR, Kündig T, Fried M, et al. Induction or exacerbation of psoriasis in patients with Crohn's disease under treatment with anti-TNF antibodies. Digestion. 2014; 89:209–215.

10. Lee H, Lee MH, Lee DY, Kang HY, Kim KH, Choi GS, et al. Prevalence of vitiligo and associated comorbidities in Korea. Yonsei Med J. 2015; 56:719–725.

11. Al-Mamari F, Al-Shirawi A, Banodkar D, Al-Hashmi S, Al-Yahyaae F, Varghese M, et al. HLA Antigens in Omani Psoriasis Vulgaris Patients. Oman Med J. 2009; 24:27–29.
12. Santos G, Sousa L. Syndrome in question. Multiple autoimmune syndrome. An Bras Dermatol. 2014; 89:361–362.
13. Kim M, Choi KH, Hwang SW, Lee YB, Park HJ, Bae JM. Inflammatory bowel disease is associated with an increased risk of inflammatory skin diseases: a population-based cross-sectional study. J Am Acad Dermatol. 2017; 76:40–48.

14. Smith RL, Warren RB, Eyre S, Ho P, Ke X, Young HS, et al. Polymorphisms in the IL-12beta and IL-23R genes are associated with psoriasis of early onset in a UK cohort. J Invest Dermatol. 2008; 128:1325–1327.

15. Kim SW, Kim ES, Moon CM, Park JJ, Kim TI, Kim WH, et al. Genetic polymorphisms of IL-23R and IL-17A and novel insights into their associations with inflammatory bowel disease. Gut. 2011; 60:1527–1536.

16. Ismail WA, Al-Enzy SA, Alsurayei SA, Ismail AE. Vitiligo in a patient receiving infliximab for refractory ulcerative colitis. Arab J Gastroenterol. 2011; 12:109–111.

17. Posada C, Flórez A, Batalla A, Alcázar JJ, Carpio D. Vitiligo during treatment of Crohn's disease with adalimumab: adverse effect or co-occurrence? Case Rep Dermatol. 2011; 3:28–31.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download