INTRODUCTION
Syphilis is a systemic infection caused by
Treponema pallidum. Clinical manifestations can mimic many other diseases
12. During the past century, syphilis treatment recommendations have advanced and penicillin, which is long acting, has become established as the therapy of choice. However, the standard method for evaluating therapeutic responses continues to be manual serological testing that relies on interpreting nontreponemal antibody test titers, such as the rapid plasma reagin (RPR) test or the venereal disease research laboratory (VDRL) test
23. A previous evaluation of the rates of decline in nontreponemal titers after treatment for primary or secondary syphilis suggested that a 4-fold decline in VDRL titers after three months or an 8-fold decline after six months represent the earliest possible times to ascertain the treatment response
4. Prevention guidelines from the United States Centers for Disease Control state that manual nontreponemal serological tests for syphilis (STS) titers should decline ≥4-fold (2 dilutions) within 3∼6 months after therapy for primary or secondary syphilis, and within 12∼24 months for latent syphilis
2. However, these manually performed tests, commonly regarded as the current gold standard for evaluating therapeutic responses, are time-consuming and have day-to-day variation in performance quality
56.
Recent efforts to overcome these hurdles have included the development of several commercially available automated STS, which are done in a chemistry autoanalyzer
789. The minimal person-to-person variation and simple automated procedures have spurred the rapid use of these automated tests, which have been steadily replacing the conventional manual nontreponemal STS
67. While the specificity of automated nontreponemal STS is high and similar to manual nontreponemal STS
710, to the best of our knowledge, there have been no studies of long-term clinical data nor recommendations for monitoring syphilis treatment responses using automated STS.
This study investigated the serological responses to treatment by human immunodeficiency virus (HIV)-negative patients who were diagnosed with syphilis and treated with benzathine penicillin G. All patients underwent two years of follow-up with titer analyses via automated nontreponemal STS. Our goal for this retrospective study was to suggest new clinical guidelines for monitoring syphilis treatment with automated STS to determine checkpoints and identify cutoff values.
MATERIALS AND METHODS
Study design and patients
After obtaining approval from the Kangbuk Samsung Hospital Institutional Review Board (KBSMC 2014-08-018-003), we reviewed clinico-laboratory data from 234 syphilis cases diagnosed with automated STS and conventional manual STS at Kangbuk Samsung Hospital from March 2007 to June 2014.
The inclusion criteria included being a syphilis patient (except tertiary syphilis patients) who received one or three doses of benzathine penicillin G that began within two weeks after diagnosis and received serological response monitoring with the same automated nontreponemal STS across follow-up. Participants excluded from this study were individuals who were pregnant (n=10), who had tertiary syphilis (n=1), infants with neonatal syphilis (n=1), and patients who were serologically positive for HIV (n=12). To monitor the serological response to treatment, we retrospectively reviewed the medical records of each enrolled cohort. We also excluded any individuals who did not undergo serological response monitoring in at least three-month intervals with the same automated nontreponemal STS.
We defined primary syphilis as cases with one or more chancres, and secondary syphilis as the presence of localized or diffuse mucocutaneous lesions, often with generalized lymphadenopathy, or other signs of secondary infection. We defined latent syphilis as an asymptomatic stage with no clinical findings and the only evidence of infection as positive seroreactivity. Latent syphilis was divided into two subcategories, according to infection duration: early (<1 year) and late (>1 year)
211. Patients who presented with primary, secondary, or early latent syphilis, were classified as having early syphilis.
Serological tests
All patients were initially tested with manual and automated STS, with follow-up via an automated nontreponemal STS at a single laboratory. All specimens were dispensed into aliquots; one was assayed with automated STS and the rest were stored at −70℃ until they were assayed by other tests. Automated STS were performed using the Mediace automated RPR (auto RPR; Sekisui Co., Tokyo, Japan) and the Mediace automated T. pallidum latex agglutination (auto TPLA; Sekisui Co., Tokyo, Japan) turbidimetric immunoassays (Sekisui Chemical Co., Ltd., Osaka, Japan). Both were performed using a Modular P800 automated clinical chemistry analyzer (Roche Diagnostics, Basel, Switzerland). The auto RPR is a nontreponemal immunoassay for quantitative detection of syphilis-related serum antibodies. The auto TPLA is a treponemal immunoassay for the quantitative detection of serum antibodies specific to T. pallidum.
For auto RPR, the autoanalyzer calculated the ratio between each sample's relative light unit and cutoff values. Samples with a ratio <1.0 were regarded as negative. The auto RPR results were expressed as RPR units (RU) based on the results of a collaborative investigation during the International Reference Preparation of Syphilitic Human Serum meeting by the World Health Organization in 1958. The auto TPLA results are expressed as titer units (TU). Samples with a concentration of T. pallidum antibody <10 TU/ml were considered negative. Results from both the auto RPR and the auto TPLA are expressed as continuous variables. For conventional manual STS, fluorescent treponemal antibody absorption testing was performed using commercially available glass slides (Zeus Scientific, Raritan, NJ, USA). All tests were performed according to the manufacturers' instructions.
Data analyses
We defined baseline as the day of treatment. In previous studies that used a conventional manual STS, the endpoint was defined as either a negative nontreponemal STS (i.e., RPR or VDRL) or a ≥4-fold (two dilution) decrease in titer
2. However, according to a previous study comparing automated nontreponemal STS with manual nontreponemal STS, test outcomes between these different methods cannot be converted to equivalent values
6. It has been hypothesized that the continuous values produced by automated nontreponemal STS differed from those from non-continuous titers from conventional manual nontreponemal STS. Thus, we decided that the only meaningful endpoint should be a conversion to negative in nontreponemal STS; we classified such events as seroreversions. Also, patients who did not serorevert during 24 months of follow-up, according to auto RPR tests, were classified into a serofast group.
The ratio of auto RPR values after treatment compared to those at baseline was defined as the auto RPR ratio for the serologic response analysis and cutoff value. To determine the cutoff value for a decrease in RU in a single patient, as a means to predict whether a patient would serorevert, patients who did and did not serorevert were compared using the receiver operating characteristic (ROC) curve on their auto RPR ratios. Also, long-term follow-up of serologic responses to treatment with the auto RPR ratio were analyzed to track response changes.
All analyses were performed using IBM SPSS Statistics ver. 22.0 software (IBM Co., Armonk, NY, USA).
RESULTS
Clinical and serological baseline characteristics
From March 2007 to July 2014, 234 patients in Asia were diagnosed with syphilis under conditions that met our study's inclusion criteria. After excluding patients for reasons explained above, 185 patients were initially enrolled but 96 patients were dropped after failing to meet the two-year follow-up criteria (
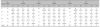
Fig. 1). The baseline characteristics and serological results of the patients we analyzed are summarized in
Table 1. Males were more predominant among the set of participants who had early-stage syphilis. Late-stage syphilis was significantly associated with increased age and higher frequency of reinfection. The prevalence of allergic reactions to penicillin was low (2/183, 1.1%). Both baseline RU and TU were significantly lower (
p<0.001) in late syphilis than in early syphilis. Although the baseline RU was higher among early-stage syphilis cases, baseline RU and TU were statistically indistinguishable among primary, secondary, and early latent syphilis.
Serologic response to treatment with auto RPR
Eighty-seven patients were followed-up for 24 months or until they showed evidence of seroreversion on an auto RPR test. Overall, 89.7% of patients (78/87) eventually seroreverted and 10.3% (9/87) remained in the serofast group. In the seroreversion group, 74.4% of patients (58/78) achieved seroreversion within 12 months after starting treatment and 25.6% (20/78) achieved seroreversion between 12 and 24 months after treatment. After 12 months, half of the remaining patients in the seroreversion group (10/20) achieved seroreversion by their 15-month follow-up appointment.
The serological response to treatment was relatively fast among primary syphilis patients; primary syphilis had completely seroreverted after six months among these patients, while 28.0% (7/25) of secondary and 21.9% (7/32) of early latent syphilis patients had seroreverted. After two years of follow-up, one secondary patient (1/25, 4.0%), three early latent patients (3/32, 9.4%) and five late latent patients (5/15, 33.3%) remained in the serofast group.
Analysis of auto RPR values
In our analyses of changes in auto RPR ratios with comparisons between patients who did and did not serorevert by the two-year follow-up point, 22.2% (18/87) of patients experienced an auto RPR increase (auto RPR ratio ≥1) while variations in the auto RPR ratio were observed during the first six months after treatment, regardless of whether the patient seroreverted. Within six months, the lowest and highest auto RPR ratios among the serofast group were 0.76 at 114 days and 1.54 at 73 days, and the lowest and highest auto RPR ratios among the seroreversion group were 0.00 at 28 days and 1.68 at 32 days. However, six months after treatment, all patients in the seroreversion group showed a decreasing pattern in their auto RPR ratio, in contrast with patients in the serofast group whose auto RPR ratios remained constant or increased.
In an overall comparison of patients who did and did not serorevert after six months of follow-up, the ROC curve for the auto RPR ratios had a sensitivity of 92.3% and a specificity of 100%, with a cutoff value of 0.88 and the area under the ROC curve was 0.991 (95% confidence interval [95% CI], 0.973∼1.000). After nine months of follow-up, the ROC curve for the auto RPR ratios had a sensitivity of 96.2% and a specificity of 100%, with a cutoff value of 0.75 and the area under the ROC curve was 1.000 (95% CI, 1.000∼1.000). After 12 months of follow-up, the ROC curve for the auto RPR ratios had a sensitivity of 91.0% and a specificity of 100%, with a cutoff value of 0.49 and the area under the ROC curve was 1.000 (95% CI, 1.000∼1.000).
Long-term follow-up of serologic responses to treatment based on auto RPR ratio
To track serologic response changes, patients were divided into five groups according to their auto RPR ratio (group A: seronegative, group B: 0<auto RPR ratio<0.50, group C: 0.50≤auto RPR ratio<0.75, group D: 0.75≤auto RPR ratio<1.0, group E: auto RPR ratio≥1.0). We also performed time series analyses (
Table 2).
After six months of treatment, 63.2% (55/87) of patients had not shown evidence of seroreversion, and were divided into four groups according to the following cutoff values: 1) Patients (n=6) who had RUs higher than or equal to their baseline auto RPR value (auto RPR ratio≥1.0) six months after treatment and continued to show positive auto RPR results during their 24 months of follow-up; all were classified into the serofast group. 2) Patients (n=16) who had a positive auto RPR ratio<0.5 six months after treatment and seroreverted by their next three-month follow-up appointment. 3) Patients (n=17) who had an auto RPR ratio in the range of 0.50∼0.75 six months after treatment; only one patient achieved seroreversion nine months after treatment. 4) The other 16 patients who had an auto RPR ratio in the range of 0.75∼1.0 six months after treatment had variable auto RPR ratios across their follow-up appointments (decreased: n=9, stationary: n=5, increased: n=2).
After nine months of treatment, 43.7% (38/87) of patients had not shown evidence of seroreversion and were divided into three groups according to the following cutoff values: 1) Patients (n=13) who had an auto RPR ratio ≥0.75 nine months after treatment; none achieved seroreversion by 15 months after treatment and nine patients (9/13, 69.2%) remained in the serofast group after 24 months of follow-up. 2) Patients (n=12) who had an auto RPR ratio <0.5 nine months after treatment; nine patients (9/12, 75.0%) achieved seroreversion after 12 months of follow-up and all 12 patients achieved seroreversion by the 15-month follow-up point. 3) Patients (n=13) who had an auto RPR ratio in the range of 0.50∼0.75 nine months after treatment; seven patients (7/13, 53.8%) achieved seroreversion after 15 months of follow-up.
After 12 months of treatment, 33.3% (29/87) of patients had not yet seroreverted. In the 12 patients who had an auto RPR ratio <0.5 12 months after treatment, 10 patients (10/12, 83.3%) achieved seroreversion by 15 months of follow-up. However, the other 17 patients who had an auto RPR ratio of ≥0.50 12 months after treatment did not serorevert within 15 months of follow-up, and 9 of 17 patients (52.9%) were finally classified into the serofast group after 24 months of follow-up.
Based on these results, we propose new clinical guidelines for serological responses to syphilis treatment using automated STS (
Fig. 2).
DISCUSSION
To the best of our knowledge, this is the first study to assess clinical guidelines using long-term data from automated nontreponemal STS, with both a long duration of follow-up after syphilis treatment and using cutoff values to assess seroreversion. Although the scale of following patients (group B, C, D, and E in the
Table 2) was quite small, it is reasonable portion of patients to interpret the changes in serologic responses as a subgroup. Due to observe the serologic responses of each subgroup based on auto RPR ratio, we revealed the changes of auto RPR ratio after syphilis treatment. We were not able to observe trends in auto RPR values within the first six months after treatment because variation between patients was very high. We found that the most important primary checkpoint was an increase in RU six months after treatment, and we concluded that the next checkpoint should be nine months after treatment. A 25% reduction in automated STS value nine months after treatment and a 50% reduction 12 months after treatment may be key indicators for predicting seroreversion within one year after treatment for syphilis among HIV-negative individuals.
In a previous, large-scale, prospective study with HIV-negative early syphilis patients, 77.2% of participants had achieved a serological cure six months after starting treatment, including seroreversion rates of 87.0%, 85.8%, and 62.1% in primary, secondary, and early latent syphilis, respectively
12. Seroreversion six months after treatment was similar among primary syphilis patients (100.0%), and generally lower among secondary (20.1%) and early latent (19.2%) syphilis patients compared to previous reports. The seroreversion rate at the final 24-month follow-up checkpoint was 100.0%, 94.4%, 80.8%, and 59.0% in primary, secondary, early latent, and late latent syphilis, respectively. These differences are likely due to different definitions for serological endpoints between this study, which used a negative nontreponemal STS, and a prior study
4, which used a ≥4-fold (two dilution) decrease in titer as a cutoff value.
We found that many cases experienced an increase in auto RPR values within the six months following treatment, regardless of syphilis stage. These results were consistent with a prior report of nontreponemal titer variation in the two weeks following initiation of syphilis treatment
13. Because of the high variation in the first six months following treatment, we concluded that evaluating seroreversion during the first six months following treatment is not necessary.
According to our findings, patients who had auto RPR values higher than or equal to their baseline value (auto RPR ratio≥1.0) six months after treatment were predicted to be treatment failures and remain in the serofast group. In contrast, patients who had auto RPR values lower than their baseline values six months after treatment typically required follow-up analyses to make better recommendations for further treatment. Although the ROC curve for auto RPR ratios at the six-month follow-up point allowed for a first cutoff value of 0.88, we conclude that early screening will reveal which patients are most likely to remain serofast or experience a treatment failure, which is an important indicator for infectious disease control. Also, patients with an auto RPR ratio ≥0.75 at the nine-month follow-up point can be classified into serofast status. In contrast, patients with an auto RPR ratio <0.50 nine months after treatment have a higher likelihood of seroreversion; thus, one more serologic exam to confirm seroreversion should be conducted 12∼15 months after treatment.
When our clinical guidelines were applied, a total of eight patients four patients with an auto RPR ratio ≥0.75 (nine months after treatment) and four patients with an auto RPR ratio ≥0.50 (12 months after treatment) who would be expected to serorevert within 15 to 24 months following therapy were forced to undergo an unnecessary additional syphilis treatment. However, re-treatment of these patients is still recommended because the group that the patients belong to has a high likelihood of treatment failure. In this study, we did not administer additional benzathine penicillin G treatments for the serologic failure group. Therefore, further studies of serologic responses to re-treatment among serofast or non-seroreverted syphilis patients are needed.
Currently, manual nontreponemal STS guidelines are used in accordance with syphilis staging and titer reduction
23. However, the syphilis staging definition according to disease duration relies entirely on patient recall, which is often inaccurate. Also, these manually performed tests, commonly regarded as the current standard for evaluating therapeutic responses, are time-consuming and vary in day-to-day performance. The automated nontreponemal STS that we used in this study does not require syphilis staging and provides data automatically. Thus, we conclude that automated nontreponemal STS has several advantages over manual nontreponemal STS.
This study has several limitations. First, we are concerned about a possible selection bias because 52.5% (96/183) of patients were excluded because they had incomplete clinical or follow-up data. In studies that required 12 months of follow-up after syphilis treatment, 42%∼48% of patients dropped out after one year
1415. Our second limitation concerns the retrospective nature of this study. A prospective analysis with regular short-interval follow-ups is the best way to evaluate syphilis monitoring. Nevertheless, our study may be helpful for predicting serologic responses to syphilis treatment using automated STS. Third, in studies of sexually transmitted diseases, including syphilis, there is always a possibility of reinfection during the follow-up period. Fourth, only a single automated treponemal STS was evaluated. A comparison of the long-term clinical outcomes among various assays might also be necessary. Additionally, because these recommendations do not guarantee the actual loss of infectivity or complete cure, further studies will be needed to estimate the correlation between the cutoff values for predicting serological cures and true immunity or bactericidal status.
In conclusion, this study provides the first definite recommendations for long-term monitoring of serologic responses to treatment using an automated STS. This evidence-based study suggests that the most important primary checkpoint is an increase in RU six months after treatment, and a 25% decrease in RU nine months after treatment and a 50% decrease 12 months after treatment are key indicators for predicting seroreversion after treatment in syphilis patients who are HIV-negative. These recommendations may provide guidance for reducing unnecessary follow-up and re-treatment for syphilis. This study is a good model for similar future studies, and contributes to the suppression of the recent global expansion of syphilis by offering recommendations for effective management.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download