Abstract
Background
Alopecia areata is the most common cause of localized, nonscarring alopecia. Unfortunately, there are few data regarding clinical features and epidemiology of alopecia areata in Korean patients, and its clinical course and treatment response rates are unpredictable.
Objective
This study strived to investigate the differences in clinical profiles according to disease severity and to determine risk factors for severe alopecia areata.
Methods
A total of 1,137 patients from 2006 to 2015 were analyzed retrospectively. Patients were subdivided into two groups: mild-to-moderate and severe alopecia areata. The groups were compared on the basis of age of onset, duration, sex, family history, comorbid disorders including autoimmune diseases, nail changes, and laboratory test results.
Results
Eight hundred eighty-three patients were in the mild-to-moderate alopecia areata group and 254 patients were in the severe group. Average onset age was 30.77±17.66 years and 30.60±16.75 years in the mild-to-moderate and severe groups, respectively. Disease duration was statistically longer in the severe group. Male sex, nail changes, and thyroid diseases were more common in the severe group. Hypertension, diabetes mellitus, dyslipidemia, atopic dermatitis, and family history did not differ between groups. Of the serologic values, only alkaline phosphatase was considerably differing between groups. Male sex, presence of nail changes, and disease duration greater than one year were identified as significant risk factors for severe alopecia areata.
Alopecia areata (AA) is a common disease that directly relates to nonscarring hair loss1. The typical clinical aspects are variable sized, well-circumscribed, oval or round bald patches. In most cases, spontaneous regrowth of hair occurs and the treatment response is good. However, some patients show chronicity and rapid progression, resulting in the entire loss of scalp and body hair2. As the course of the disease is variable, it is very difficult to predict the prognosis and treatment response on clinical examination. The exact pathogenesis remains unclear, but it is assumed that AA is an organ-specific autoimmune disease, mediated by autoreactive CD8+ T cells, which affects hair follicles13. Consequently, atopic dermatitis, autoimmune diseases including vitiligo, and thyroid disease are associated with AA45. Reports on serologic findings are diverse, but patients with AA tend to show autoantibodies at a higher rate than the general population6.
There are few reports concerning the clinical characteristics, epidemiology, and prognosis of Korean patients with AA. Therefore, we investigated the differences in clinical profiles based on disease severity that have relevance to prognosis and risk for severe AA.
All subjects with AA who were examined at Chonnam National University Hospital (Gwangju, Korea) from January 2006 to December 2015 were enrolled in this study. The study protocol was approved by the institutional review board of Chonnam National University Hospital (IRB no. CNUH 2017-259).
This study retrospectively analyzed the medical records and clinical photographs. Patients were divided into two groups based on the extent of AA at their first medical examination: less than 50% involvement of the entire scalp was considered mild-to-moderate AA, and greater than 50% involvement of the entire scalp, alopecia totalis, and alopecia universalis were considered severe AA. Patients with acute diffuse and total alopecia or rapidly progressive AA were identified based on clinical history and disease progression, and were excluded from the analysis. Demographic data on age, sex, duration, age of onset, family history, nail changes, and associated diagnoses including autoimmune diseases were obtained for all patients. We investigated the presence of thyroid diseases including thyroid cancer, Grave's disease, Hashimoto thyroiditis, simple goiter, and autoimmune diseases including autoimmune thyroid disease (Grave's disease, Hashimoto thyroiditis), systemic lupus erythematosus, vitiligo, rheumatoid arthritis, adult-onset Still's disease, ulcerative colitis, Sjogren's syndrome, and others. We also compared and analyzed hematologic laboratory results, serum iron concentration, the presence of autoimmune antibodies, and thyroid function tests.
The results are expressed as mean±standard deviation. Pearson's chi-square test and Fisher's exact test were used to compare the sex ratio, nail changes, family history, and comorbidities, including autoimmune diseases, between the mild-to-moderate and severe AA groups. Comparison of age of onset, disease duration, and hematologic results between the two groups were performed using the independent t-test, and risk factors for severe AA were determined by logistic regression analysis. The analysis was performed using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA). A p-value <0.05 was considered statistically significant.
A total of 1,137 individuals with AA were included: 583 male and 554 female. Average age was 32.63±17.40 years and average duration was 19.86±43.83 months. Mild-to-moderate AA was present in 883 patients (77.7%) and severe AA in 254 patients (22.3%) (Table 1). The average of onset was 30.77±17.66 years and 30.60±16.75 years in the mild-to-moderate and severe groups, respectively, and average disease duration was 15.89±34.70 months and 33.68±64.66 months, respectively. Duration was longer in the severe AA group than in the mild-to-moderate AA group (p<0.001). The male-to-female ratio was 429:454 in the mild-to-moderate group and 154:100 in the severe group; thus male patients had more severe disease (p=0.001). Family history and early onset (AA before 13 years old) were not significantly different between the two groups, but nail changes were more common in the severe group (p<0.001, Table 2).
There was no significant difference in the frequencies of hypertension (p=0.982), diabetes mellitus (p=0.732), dyslipidemia (p=0.160), atopic dermatitis (p=0.849), or vitiligo (p=0.129) between the two groups. Thyrid diseases (p=0.002) and autoimmune diseases (p=0.036) were more common in the severe group.
Of the 1,137 total patients, 853 patients had laboratory blood test results: 639 in the mild-to-moderate group and 214 in the severe group. The level of alkaline phosphatase (ALP) was lower in the severe group (p=0.028). All other results, including serum iron and thyroid function, were not significantly different between groups (Table 3). Antinuclear antibody (ANA) was positive in 16.7% of the mild-to-moderate group and 11.7% of the severe group. Antithyroglobulin antibody was positive in 15.7% and 15.2% of the mild-to-moderate and severe groups, respectively (Table 3).
To determine the risk factors of severe AA, the statistically significant factors of severe AA were analyzed by logistic regression analysis (Table 4). In multivariable logistic regression analysis, male sex (p<0.001; odds ratio [OR], 1.726; 95% confidence interval [CI], 1.282~2.325), presence of nail changes (p<0.001; OR, 4.104; 95% CI, 2.357~7.146), and disease duration greater than 1 year (p<0.001; OR, 2.405; 95% CI, 1.791~3.229) were associated with an increased risk of severe AA (Table 4).
AA presents with variable-sized, demarcated, oval or round patches of hair loss; the estimated lifetime risk among the general population is 1.7%7. Disease severity can be classified as follows: S1 (<25% scalp involvement), S2 (26%~50%), S3 (51%~75%), S4 (76%~99%), and S5 (100%, alopecia totalis) based on guidelines of the American National Alopecia Areata Foundation8. However, owing to the variable size of lesions and the waxing and waning property of alopecia patches, several publications concerning treatment divide AA patients into two groups: mild-to-moderate (less than 50% scalp involvement; localized) and severe (greater than 50% scalp involvement; extensive). Severity of AA at the time of treatment initiation is known to be the most important prognostic factor, as reported by several other authors910. Hence, we compared the clinical profiles of mild-to-moderate and severe AA patient groups at first medical examination to investigate risk factors associated with severe AA.
Mean age of onset was similar between groups, but male sex was more common in the severe group (p=0.001). Studies in India11 and China12 found that males had more severe AA, while female patients were more likely to have severe disease in a report from Singapore13. The association of sex with AA severity is unclear, and additional study is needed.
According to previous reports, prognosis and treatment response is poor in patients with severe AA (particularly in cases of alopecia totalis and alopecia universalis)91415, nail changes16, a history of atopic dermatitis or other autoimmune disease16, and longer period from symptom development to start of treatment initiation414.
Our data shows that family history and early age of onset was not significantly different between the two groups. On the other hand, longer disease duration (p<0.001) and nail changes (p<0.001) were more common in severe AA. Early onset AA is alopecia that develops before adolescence. Disease severity and symptom development before 13 years of age had no significant association in our study (p=0.401). p-values for the association of AA severity and age of onset were 0.305 before 10 years of age, 0.055 before 9 years, 0.055 before 8 years, 0.099 before 7 years, and 0.256 before 6 years. These results are quite different from those reported by previous studies1617.
Nail changes in AA can present as trachonychia, pitted nail, or longitudinal ridges; the frequency of nail changes increases with disease severity111819. We did not subdivide patients based on nail changes, but nail changes were more frequent in the severe AA group (p<0.001). This is thought to be due to the action of inflammatory cells targeting hair follicles acting on nails, as their growth structure resemble that of hair follicles20.
Disease duration was 15.89±34.70 months and 33.68±64.66 months in the mild-to-moderate and severe groups, respectively; thus the severe group showed disease duration twice that of the mild-to-moderate group (p<0.001). The mild-to-moderate and severe AA groups had disease duration of greater than 1 year in 27.4% and 49.2% of patients (p<0.001). This finding is consistent with previous reports that prognosis is improved with early treatment initiation1421.
The associations between AA and atopic dermatitis, vitiligo, autoimmune diseases, and thyroid diseases are well known45. However, we found no association between severity and atopic dermatitis (p=0.849). In the present investigation, 9.6% of patients had autoimmune disease. Thyroid diseases (p=0.002) were associated with severe AA, but vitiligo (p=0.129) was not. Additionally, autoimmune diseases were more common in the severe group (p=0.036). Based on these results, despite the unclear etiology of AA, an immune pathogenesis seems to play an important role222324. Normal anagen hair is an immune privileged site. However, the loss of immune privilege allows for the progression of the inflammatory process, with infiltration of CD4+ and CD8+ T cells in AA24.
Although they were in normal range, ALP was significantly lower in the severe group (p=0.028). ALP is a zinc-metallo enzyme that is highly expressed in actively proliferating cells or cells with a high metabolic rate25. By immunohistochemical staining, ALP activity is prominent in normal pilosebaceous units, and there are several reports of decreased ALP activities in hair follicles of patients with AA and mouse models of AA252627. ALP concentration in hair follicles can correlate with serum levels, and it is speculated that decreased serum ALP is due to diminished functioning follicles in chronic, severe AA.
On the other hand, iron levels and thyroid function test were not significantly different between groups. Although there is controversy concerning the association of iron deficiency and AA28, our result is in agreement with previous research showing no correlation between iron deficiency and disease severity282930. In our study, ANA was positive in 16.7% of patients in the mild-to-moderate group and 11.7% of patients in the severe group. Antithyroglobulin antibody was positive in 15.7% and 15.2%, respectively, with no statistically significant difference.
In logistic regression analysis, risk factors associated with increased disease severity were male sex (p<0.001), nail changes (p<0.001), and disease duration greater than 1 year (p<0.001). These results are similar to previous reports concerning AA prognosis. However, additional nationwide, ethnic studies should be performed in order to further investigate the correlation between sex and disease severity and to determine differences in other countries.
This study is limitfved because it is a retrospective, single-center study based on review of patients' medical record. Thus, the data is subject to recall bias and selection bias. Since blood tests were not performed on all patients, it is difficult to generalize and interpret the data carefully. In addition, we only evaluated for the presence or absence of thyroid disease, and did not classify the diagnoses in details. Since we evaluated for the presence of ANA and antithyroglobulin antibody only, there is a possibility that the combined effects of multiple different autoimmune antibodies are underestimated. Additionally, we compared only the clinical profiles between two severity groups but we did not analyze the effect of different treatment modalities or prognostic factors.
Despite these limitations, this is the study on the largest scale of Korean patients with AA thus far. In conclusion, this study analyzed clinical profiles of patients with AA according to severity and evaluated risk factors associated with severe AA. We found that male sex, nail changes, and duration greater than 1 year are risk factors for severe disease. Other demographic and clinical parameters, such as a history of atopic dermatitis, vitiligo, and early AA onset were not associated with disease severity. Serum ALP level was significantly lower in the severe AA group, and represents a potentially useful predictor of prognosis and treatment response. However, further long-term and prospective studies are needed to clarify these issues.
Figures and Tables
Table 1
Patient demographics and clinical data of the whole cohort (n=1,137)
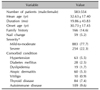
Table 2
Characteristics of patients with AA according to severity

Table 3
Laboratory findings and autoantibodies in patients with AA

Values are presented as mean±standard deviation or number (%). AA: alopecia areata, Hgb: hemoglobin, WBC: white blood cells, Plt: platelets, ALP: alkaline phosphatase, AST: aspartate transminase, ALT: alanine transaminase, BUN: blood urea nitrogen, Cr: creatinine, TIBC: total iron binding capacity, TSH: thyroid-stimulating hormone, ANA: antinuclear antibody. *p-value <0.05 was considered statistically significant. †Independent samples t-test was used. ‡Chi-square test or Fishers exact test was used.
Table 4
Risk factors for severe alopecia areata

References
1. Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part I. Clinical picture, histopathology, and pathogenesis. J Am Acad Dermatol. 2010; 62:177–188.
2. Assouly P, Reygagne P, Jouanique C, Matard B, Marechal E, Reynert P, et al. Intravenous pulse methylprednisolone therapy for severe alopecia areata: an open study of 66 patients. Ann Dermatol Venereol. 2003; 130:326–330.
4. Kakourou T, Karachristou K, Chrousos G. A case series of alopecia areata in children: impact of personal and family history of stress and autoimmunity. J Eur Acad Dermatol Venereol. 2007; 21:356–359.

5. Chu SY, Chen YJ, Tseng WC, Lin MW, Chen TJ, Hwang CY, et al. Comorbidity profiles among patients with alopecia areata: the importance of onset age, a nationwide populationbased study. J Am Acad Dermatol. 2011; 65:949–956.

7. Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton LJ 3rd. Incidence of alopecia areata in Olmsted County, Minnesota, 1975 through 1989. Mayo Clin Proc. 1995; 70:628–633.

8. Olsen E, Hordinsky M, McDonald-Hull S, Price V, Roberts J, Shapiro J, et al. Alopecia areata investigational assessment guidelines. National Alopecia Areata Foundation. J Am Acad Dermatol. 1999; 40:242–246.
9. Tosti A, Bellavista S, Iorizzo M. Alopecia areata: a long term follow-up study of 191 patients. J Am Acad Dermatol. 2006; 55:438–441.

10. van der Steen PH, van Baar HM, Happle R, Boezeman JB, Perret CM. Prognostic factors in the treatment of alopecia areata with diphenylcyclopropenone. J Am Acad Dermatol. 1991; 24:227–230.

11. Sharma VK, Dawn G, Kumar B. Profile of alopecia areata in Northern India. Int J Dermatol. 1996; 35:22–27.

12. Xiao FL, Yang S, Liu JB, He PP, Yang J, Cui Y, et al. The epidemiology of childhood alopecia areata in China: a study of 226 patients. Pediatr Dermatol. 2006; 23:13–18.

13. Tan E, Tay YK, Giam YC. A clinical study of childhood alopecia areata in Singapore. Pediatr Dermatol. 2002; 19:298–301.

14. Park MS, Piao YJ, Park YO, Seo YJ, Suhr KB, Lee JH, et al. Analysis the prognostic factors of alopecia areata. Korean J Dermatol. 2004; 42:825–832.
15. Tan E, Tay YK, Goh CL, Chin Giam Y. The pattern and profile of alopecia areata in Singapore--a study of 219 Asians. Int J Dermatol. 2002; 41:748–753.

16. De Waard-van der Spek FB, Oranje AP, De Raeymaecker DM, Peereboom-Wynia JD. Juvenile versus maturity-onset alopecia areata--a comparative retrospective clinical study. Clin Exp Dermatol. 1989; 14:429–433.

17. Lee NR, Kim BK, Yoon NY, Lee SY, Ahn SY, Lee WS. Differences in comorbidity profiles between early-onset and late-onset alopecia areata patients: a retrospective study of 871 Korean patients. Ann Dermatol. 2014; 26:722–726.

18. Muller SA, Winkelmann RK. Alopecia areata. An evaluation of 736 patients. Arch Dermatol. 1963; 88:290–297.
19. Sharma VK, Dawn G, Muralidhar S, Kumar B. Nail changes in 1000 Indian patients with alopecia areata. J Eur Acad Dermatol Venereol. 1998; 10:189–191.

20. Mustonen T, Pispa J, Mikkola ML, Pummila M, Kangas AT, Pakkasjärvi L, et al. Stimulation of ectodermal organ development by Ectodysplasin-A1. Dev Biol. 2003; 259:123–136.

21. Yang CC, Lee CT, Hsu CK, Lee YP, Wong TW, Chao SC, et al. Early intervention with high-dose steroid pulse therapy prolongs disease-free interval of severe alopecia areata: a retrospective study. Ann Dermatol. 2013; 25:471–474.

22. Bertolini M, Gilhar A, Paus R. Alopecia areata as a model for T cell-dependent autoimmune diseases. Exp Dermatol. 2012; 21:477–479.

23. Alexis AF, Dudda-Subramanya R, Sinha AA. Alopecia areata: autoimmune basis of hair loss. Eur J Dermatol. 2004; 14:364–370.
24. Gilhar A, Paus R, Kalish RS. Lymphocytes, neuropeptides, and genes involved in alopecia areata. J Clin Invest. 2007; 117:2019–2027.

25. Hahnel AC, Rappolee DA, Millan JL, Manes T, Ziomek CA, Theodosiou NG, et al. Two alkaline phosphatase genes are expressed during early development in the mouse embryo. Development. 1990; 110:555–564.

26. Li L, Paus R, Slominski A, Hoffman RM. Skin histoculture assay for studying the hair cycle. In Vitro Cell Dev Biol. 1992; 28A:695–698.

27. Manes T, Glade K, Ziomek CA, Millán JL. Genomic structure and comparison of mouse tissue-specific alkaline phosphatase genes. Genomics. 1990; 8:541–554.

28. White MI, Currie J, Williams MP. A study of the tissue iron status of patients with alopecia areata. Br J Dermatol. 1994; 130:261–263.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download