Abstract
Background
There have been few studies of treatment adherence in Asian patients with psoriasis and understanding of the factors is important to improve outcomes.
Objective
To provide an overview of treatment adherence among Korean patients with psoriasis and to understand how the perceptions of patients and physicians affect topical treatment adherence.
Methods
A cross-sectional questionnaire survey was conducted to determine the views and opinions of dermatologists and psoriasis patients on topical treatment adherence. The survey items were developed in collaboration with psoriasis experts.
Results
Twenty-six dermatologists and fifty patients completed their questionnaire. In the physician survey, more than half of dermatologists only inquired about adherence up to 20% of the time. Most dermatologists generally thought that their patients had high expectations of treatment. Nearly 40% of dermatologists reported that more than 60% of their patients adhered to the prescribed topical treatment. In the patient survey, more than 15% of patients reported that they did not receive enough information about the drug. Around one-fifth of the patients also complained about the physical properties of the products. The majority of patients were confident with the current topical treatments and expected fast improvement, within a couple of weeks. The most common reason for low adherence was forgetfulness. Inconvenience and concerns about side effects were common reasons for topical treatment discontinuation.
Adherence to (or compliance with) treatment is generally defined as the extent to which patients' treatment-related behaviors agree with a health professional's advice. The word “adherence” is preferred by many health care providers, because “compliance” suggests that the patient is passively following the doctor's orders and that the treatment plan is not based on a therapeutic alliance or contract established between the patient and the physician1. The turning point that separates “adherence” from “non-adherence” can be defined as anything in the natural history of a disease that makes the desired therapeutic outcome likely (adherence) or unlikely (non-adherence) to occur2. Adherence rates for patients with chronic diseases, including psoriasis and atopic dermatitis, have been shown to decrease over time, and non-adherence leads to suboptimal health outcomes, lower quality of life, and eventually, increased health care costs. It is estimated that more than one-third of psoriasis patients do not adhere to their prescribed medications34. Various reasons have been suggested to explain the low adherence of patients with psoriasis. In a previous study, the most common reasons patients cited for non-adherence to topical treatment were low efficacy, time consumption, and poor cosmetic characteristics of topical agents5. Studies have shown that physician communication styles that address patients' conditions are related to better treatment adherence. Additionally, the scheduling behavior of physicians is associated with adherence among patients with chronic dermatologic diseases6. A recent multinational survey of patients with psoriasis reported that low adherence was related to a mixture of patient-, physician- and treatment-related factors rather than to a single factor7.
Until recently, there have been few studies on treatment adherence in Asian patients with psoriasis, although understanding the factors that affect medication adherence is an essential step toward obtaining successful outcomes. Therefore, we conducted a survey to assess various factors that may affect adherence. This is the first survey to provide an overview of treatment adherence among Korean patients with psoriasis. The objective of our study was to determine how the perceptions of patients and physicians affect topical treatment adherence.
A cross-sectional questionnaire survey was conducted from March to June 2013 in Korea to examine the views and opinions of dermatologists and psoriasis patients on topical treatment adherence. Web-based surveys were circulated among dermatologists who specialized in psoriasis, and printed questionnaires were distributed to psoriasis patients visiting an outpatient psoriasis clinic. Patients who were at least 18 years of age who were diagnosed with psoriasis by a dermatologist and who were receiving a topical therapy were eligible to participate, and participants who did not completely respond to the survey were excluded. The study protocol was approved by the institutional review board of Seoul National University Bundang Hospital (IRB no. B-1303/196-304) and conducted according to the principles of the Declaration of Helsinki.
The survey items were developed in collaboration with a psoriasis expert group, the Asia Adherence Study Group. The Asia Adherence Study Group comprised expert dermatologists, including S. W. Youn, experienced in the management of psoriatic patients from six different Asian countries. Physicians were asked 9 questions about the average time spent during first consultations, the factors they considered to be most important for patient adherence, the proportion of patients who understood instructions on how to use their medications correctly, patient expectations of treatment, the proportion of the time they asked patients about treatment adherence during follow-up visits, their estimate of the average adherence of patients, reasons for non-adherence, and ways to improve the adherence.
Patients were asked 18 questions about the duration of first and follow-up consultations and their satisfaction with the length of consultations, their knowledge and understanding of the prescribed treatment, their feelings about treatment (confidence, convenience, pleasantness, costs, and concerns about side effects), their adherence with treatment instructions, their expectations of treatment, and how treatment efficacy affected their willingness to continue treatment.
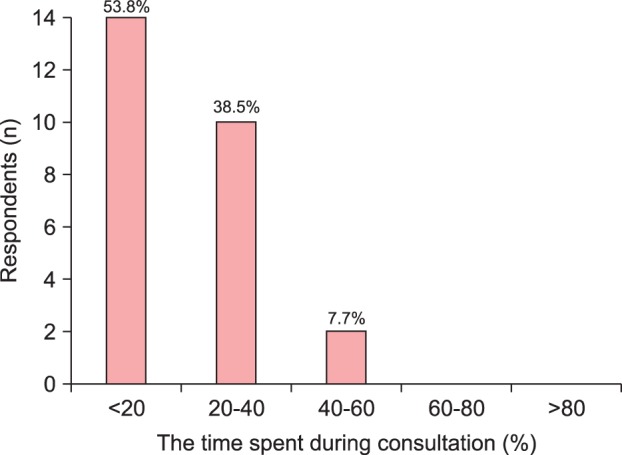
In the first part of the questionnaire, dermatologists were asked how much time they usually spent with patients during first consultations. The majority of dermatologists (61.5%) reported spending 5∼10 minutes in the initial consultation. No physician spent longer than 20 minutes. During the follow-up visit, more than half of dermatologists (53.8%) only inquired about adherence up to 20% of the time (Fig. 1).
At initial diagnosis, half of dermatologists (50.0%) reported that more than half of their patients expected to become totally cured of the disease. More than 90% of physicians indicated that more than half of their patients expected complete clearance of skin lesions. Overall, most dermatologists generally thought that their patients had high expectations of treatment.
The majority of physicians (76.9%) perceived that matching treatment to disease severity was the most important factor influencing patients' treatment adherence. The remaining 23.1% indicated safety as the most important factor affecting adherence. Regarding physician perception of patient adherence, 38.5% of dermatologists reported that more than 60% of their patients adhered to prescribed topical treatments (Fig. 2). As shown in Table 1, dermatologists indicated that treatment-related factors (73.1%), patient-related factors (69.2%), and communication (50.0%) appeared to influence non-adherence in the majority of their patients (>60%). In particular, about half of respondents indicated a lack of efficacy (53.8%) and inconvenience of use (46.2%) as common treatment-related factors for poor adherence in the majority of their patients. To help patients achieve good adherence, most physicians ranked patient support groups and education as the most influential factors to be improved. Improving physician's education skills and reducing treatment costs were identified as other important factors for good adherence.
More than half of patients (54.0%) responded that physicians spent 5∼10 minutes with them during their first visit; 92% of the respondents were satisfied with the length of the first and follow-up visits, and the remaining 8%, who were dissatisfied, indicated that consultations lasting 15∼30 minutes would be preferable.
About one-third of respondents expressed a lot of confidence in their treatment, and a further 52% of respondents were moderately confident with the current treatment. Up to 30% of patients expected to see improvement within 1∼2 weeks, and a further 20% expected to see faster improvement (within 1 week) when prescribed a new topical drug. Most patients (90%) were willing to continue topical treatment for the prescribed duration even if there was no improvement within the expected time period. Paradoxically, more than 90% of patients also reported that they would be willing to switch to different topical drugs if no clinical improvement was evident.
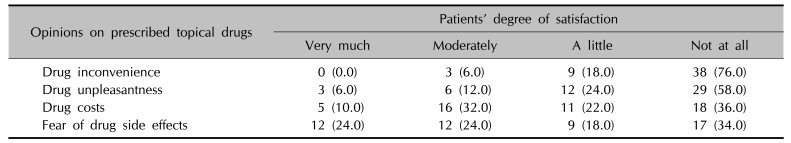
The majority of patients (68%) understood how the treatments worked, although the remaining 32% poorly understood or did not understand how their treatment worked. More than 15% of patients indicated that they considered the prescribed treatment complicated to a certain degree and were not sure about how to apply the drugs correctly. Table 2 describes how patients felt about their prescribed topical treatment for psoriasis. Six percent of respondents reported that the prescribed drugs were moderately inconvenient to use. Nearly 20% of patients (18%) expressed that the topical treatment was moderately or very unpleasant because of cosmetic characteristics, such as odor and texture. Up to 40% considered their treatment to be costly. More than 40% of patients were moderately or very concerned about adverse effects of topical treatment. However, the majority of patients (86%) were willing to continue using their topical medications for extended periods of time.
Over 20% of patients (22%) did not apply the topical agents exactly as prescribed with regard to the amount and frequency. The reasons for low adherence were forgetfulness (81.8%) and unclear instructions (18.2%). In addition, 10% of patients did not use the drugs for as long as prescribed and reported that inconvenience and concerns about side effects were the reasons for discontinuation. To cope better with psoriasis, almost half of respondents (44%) ranked a patient forum as a number one priority (Fig. 3).
Psoriasis is a chronic inflammatory skin disease that can affect up to 0.3% of the Asian population8,9,10. Recent studies have highlighted poor adherence to treatment in patients with chronic skin diseases, such as atopic dermatitis, urticaria, acne, and psoriasis11,12,13,14. Poor adherence to treatment can prevent patients from achieving disease control, so patients' high adherence to topical medication is indispensable for the management of chronic skin diseases, including psoriasis.
Although topical agents are the mainstay of treatment for mild to moderate psoriasis, psoriatic patients consistently report that topical treatment is one of the most negative aspects of the disease15. Among this study's respondents, 40% reported not using the recommended treatments as prescribed, and the true rate of poor adherence is probably much higher3,16. Factors influencing intentional non-adherence, including dissatisfaction with efficacy, inconvenience, and fear of side effects, are the most important patient-identified barriers to appropriate use of topical agents in psoriasis3. Interactions with the physician and the physician-patient relationship also affect medication adherence and indirectly influence treatment outcomes. Physicians who use understandable language, encourage open provider-patient exchange, foster patient participation in their own medical care, and create a friendly and efficient environment should increase the likelihood of adherence17,18. Overall, topical treatment adherence in psoriasis is a complex and multifaceted issue, as our study physicians indicated (Table 1).
In our survey, about half of physicians asked about treatment adherence less than 20% of the time, indicating that they did not actively follow-up with patients regarding adherence. Although the majority of patients were satisfied with the length of consultations, more than 15% of patients reported that they did not get enough information about the drug. Around one-fifth of patients also complained about the topical nature of the drugs. Regimens often are inconvenient and complex due to the characteristics of topical products and the need for frequent application to different body sites with multiple drugs. In this respect, the key outcome is not only the giving of information or information exchange, but also the achievement of understanding by the patient. This understanding should include awareness of particular outcomes of treatments and their characteristics, including benefits, possible harms, and the seriousness of the potential harms. If a drug formulation is not aesthetically acceptable to the patient, allowing the patient to choose the medication modality may improve adherence to treatment. Fear of side effects is also common, as in our physician and patient survey, and could be overcome by providing understandable information about the product. Because personal characteristics, climate, and even cultural context are related to topical treatment adherence, dermatologists should focus on determining each patient's individual adherence barriers19.
Our study showed that patients were confident with the current topical treatments and had high expectations of prescribed treatments, particularly with regard to quick clinical responses. Half of responding physicians reported that a significant proportion of their patients had unrealistic pre-treatment expectations. The majority of patients had strong beliefs in the benefits of medication and were willing to continue applying the medication for the prescribed duration even if there was no clinical improvement within the expected time frame. These strong beliefs and positive attitudes might be helpful immediately after commencing topical treatments. However, if final clinical outcomes do not meet patients' expectations, their faith in treatments and rapport with doctors could be seriously damaged in proportion to their high expectations. Therefore, physicians and patients should establish a common ground regarding the clinical outcomes of the treatments, which would eventually improve patient satisfaction with treatment. One such method includes helping patients to have a better understanding of the medicine. In this study, one-third of patients did not receive sufficient information on how treatments work. Thus, if physicians were to focus more on providing patients with an understanding of treatment mechanisms, patient satisfaction might improve. Satisfaction with a particular topical drug results in better adherence with an ultimate trend toward improved health-related quality of life20,21.
In this study, the majority of patients reported that forgetfulness was the most common reason for low adherence, including irregularly applying the topical agents. This lack of adherence might be related to improvements in the patients' skin conditions due to the topical treatments. Improvements in symptoms increase the likelihood of missing medication and discontinuing treatment. Therefore, advising patients to continue topical treatment regularly, even after they think the lesions have disappeared, is necessary in order to control subclinical inflammation and prevent recurrence. Physicians can also schedule more frequent follow-up visits to improve treatment adherence for a certain period of time6,22.
In the survey, almost half of patients ranked a patient forum as a top priority to help them to cope better with psoriasis. This result is in alignment with the physician survey results, which indicates the importance of developing patient support programs and education systems. Because of the chronic and incurable nature of the disease, psoriatic patients become frustrated when they experience tachyphylaxis or adaptation to topical treatment effects and eventually discontinue the topical medication. Thus, patient support groups that include medical professionals may be required for the management of psoriasis.
To the best of our knowledge, this is the first report providing information on topical treatment adherence in Korean patients with psoriasis. Patient adherence to topical therapy is a difficult challenge in dermatology, particularly for skin diseases like psoriasis that require long-term treatment with topical medications. The success of topical therapy in psoriasis depends on a high level of patient motivation and cooperation. Therefore, dermatologists should actively encourage patients to be involved in their own care and communicate well with them. In addition, pharmaceutical companies must make every effort to develop vehicles that are more patient-friendly in order to improve adherence.
ACKNOWLEDGMENT
Leo Pharma Korea, Ltd. financially supported this study and partially participated in questionnaire development and data analysis. The developers of the survey items, the members of the Asia Adherence Study Group, are Dr. Asawanonda P, Dr. Frez ML, Dr. Theng C, Dr. Youn SW, and Dr. Zheng M.
References
1. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005; 353:487–497. PMID: 16079372.

2. Sabaté E. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization;2003.
3. Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006; 55:607–613. PMID: 17010739.

4. Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005; 19(Suppl 3):2–6. PMID: 16274404.
5. Devaux S, Castela A, Archier E, Gallini A, Joly P, Misery L, et al. Adherence to topical treatment in psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012; 26(Suppl 3):61–67. PMID: 22512682.

6. Davis SA, Lin HC, Yu CH, Balkrishnan R, Feldman SR. Underuse of early follow-up visits: a missed opportunity to improve patients' adherence. J Drugs Dermatol. 2014; 13:833–836. PMID: 25007367.
7. Bewley A, Burrage DM, Ersser SJ, Hansen M, Ward C. Identifying individual psychosocial and adherence support needs in patients with psoriasis: a multinational two-stage qualitative and quantitative study. J Eur Acad Dermatol Venereol. 2014; 28:763–770. PMID: 23663069.

8. Chang YT, Chen TJ, Liu PC, Chen YC, Chen YJ, Huang YL, et al. Epidemiological study of psoriasis in the national health insurance database in Taiwan. Acta Derm Venereol. 2009; 89:262–266. PMID: 19479122.

9. Tsai TF, Wang TS, Hung ST, Tsai PI, Schenkel B, Zhang M, et al. Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan. J Dermatol Sci. 2011; 63:40–46. PMID: 21543188.

10. Yip SY. The prevalence of psoriasis in the Mongoloid race. J Am Acad Dermatol. 1984; 10:965–968. PMID: 6736341.

11. Torrelo A, Ortiz J, Alomar A, Ros S, Pedrosa E, Cuervo J. Health-related quality of life, patient satisfaction, and adherence to treatment in patients with moderate or severe atopic dermatitis on maintenance therapy: the CONDA-SAT study. Actas Dermosifiliogr. 2013; 104:409–417. PMID: 23665434.

12. Conlon NP, Edgar JD. Adherence to best practice guidelines in chronic spontaneous urticaria (CSU) improves patient outcome. Eur J Dermatol. 2014; 24:385–386. PMID: 24682625.

13. Snyder S, Crandell I, Davis SA, Feldman SR. Medical adherence to acne therapy: a systematic review. Am J Clin Dermatol. 2014; 15:87–94. PMID: 24481999.

14. Zschocke I, Mrowietz U, Karakasili E, Reich K. Non-adherence and measures to improve adherence in the topical treatment of psoriasis. J Eur Acad Dermatol Venereol. 2014; 28(Suppl 2):4–9. PMID: 24684738.

15. Rapp SR, Exum ML, Reboussin DM, Feldman SR, Fleischer A, Clark A. The physical, psychological and social impact of psoriasis. J Health Psychol. 1997; 2:525–537. PMID: 22013093.

16. Richards HL, Fortune DG, O'Sullivan TM, Main CJ, Griffiths CE. Patients with psoriasis and their compliance with medication. J Am Acad Dermatol. 1999; 41:581–583. PMID: 10495380.

17. Lee JY, Her Y, Kim CW, Kim SS. Topical corticosteroid phobia among parents of children with atopic eczema in Korea. Ann Dermatol. 2015; 27:499–506. PMID: 26512163.

18. Charman CR, Morris AD, Williams HC. Topical corticosteroid phobia in patients with atopic eczema. Br J Dermatol. 2000; 142:931–936. PMID: 10809850.

19. Feldman SR, Horn EJ, Balkrishnan R, Basra MK, Finlay AY, McCoy D, et al. Psoriasis: improving adherence to topical therapy. J Am Acad Dermatol. 2008; 59:1009–1016. PMID: 18835062.

20. Poyner TF, Menday AP, Williams ZV. Patient attitudes to topical antipsoriatic treatment with calcipotriol and dithranol. J Eur Acad Dermatol Venereol. 2000; 14:153–158. PMID: 11032056.

21. Renzi C, Picardi A, Abeni D, Agostini E, Baliva G, Pasquini P, et al. Association of dissatisfaction with care and psychiatric morbidity with poor treatment compliance. Arch Dermatol. 2002; 138:337–342. PMID: 11902984.

22. Feldman SR, Camacho FT, Krejci-Manwaring J, Carroll CL, Balkrishnan R. Adherence to topical therapy increases around the time of office visits. J Am Acad Dermatol. 2007; 57:81–83. PMID: 17498841.

Fig. 2
Distribution of respondents according to the percentage of patients who were adherent to treatment based on follow-up consultation.
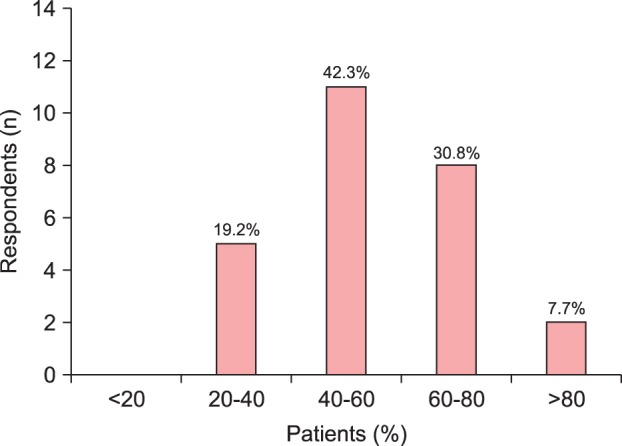
Fig. 3
Distribution of respondents according to the most useful option for improving psoriasis management from the patient's perspective.
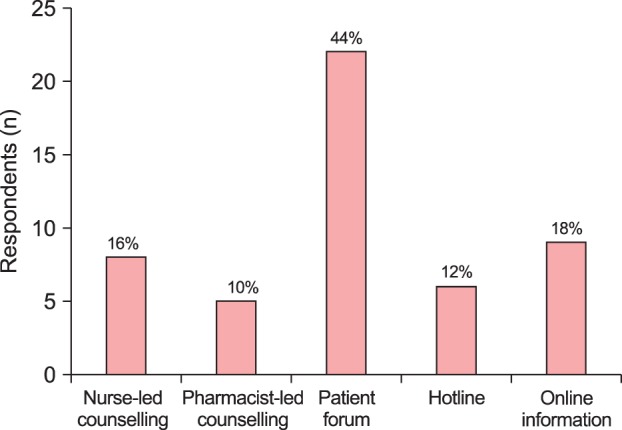
Table 1
Distribution of respondents (physicians) according to percentage of patients due to factors influencing topical treatment adherence (n=26)
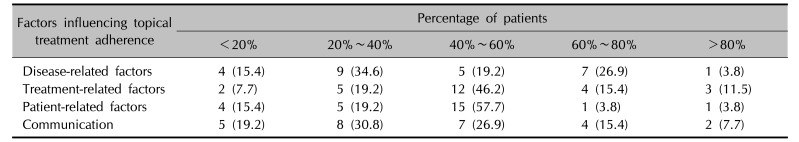
Table 2
Distribution of respondents (patients) according to patients' degree of satisfaction with prescribed topical drugs (n=50)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download