Abstract
Background
The recurrence rate of rosacea was not known very well, but has been reported as 60% in 6 months after withdrawal of the drug. It is not known which treatment can reduce relapses of rosacea effectively.
Objective
The objective was to identify whether 595 nm-pulsed dye laser (PDL) treatment reduced recurrence rate among rosacea patients who were treated with oral minocycline.
Methods
One hundred and seven Korean patients with rosacea who started treatment with oral minocycline (100 mg/d) with or without PDL (2∼4 sessions) were evaluated retrospectively. The recurrence rate was estimated using the Kaplan-Meier method, and difference was evaluated using the log-rank test. Cox proportional hazards model was used to estimate hazard ratios and 95% confidence intervals (CIs) of risk factors for the recurrence of rosacea.
Results
The recurrence-free survival analysis revealed that the group with oral minocycline plus PDL was significantly different compared with the group with oral minocycline alone (p=0.011). Cox proportional hazards model showed that the combined use of PDL with oral minocycline appeared to be a significant protective factor for the hazard of recurrence of rosacea (hazard ratio, 0.492; 95% CI, 0.257∼0.941; p=0.032).
Rosacea is a chronic inflammatory disorder with facial telangiectasia, flushing, inflammatory papules and pustules being the most commonly characterized features1. According to the National Rosacea Society Expert Committee, rosacea is categorized into 4 subtypes: erythematotelangiectatic (ETR), papulopustular (PPR), phymatous, and ocular1. ETR is characterized by nontransient episodic flushing and persistent central facial erythema1. Patients with PPR experience transient papules or pustules in addition to the characteristics seen in patients with ETR1.
There are many treatment options available for patients with rosacea. Most widely used are systemic agents like tetracycline (250∼1,000 mg per day), doxycycline (100∼200 mg per day or 20∼40 mg per day), and minocycline (100∼200 mg per day)2. The second generation tetracyclines like minocycline and doxycycline are more commonly used due to their longer half-life and better bioavailability than first generation tetracycline and their effectiveness at sub-antimicrobial but anti-inflammatory dose34. Tetracycline has been shown to reduce the level of reactive oxygen species and expression of matrix metalloproteinase and downregulate inflammatory cytokines, which has been suggested as the main mechanism of its anti-inflammatory action5.
Pulsed dye laser (PDL) has been suggested to be used adjunctively with oral and topical rosacea regimens for more complete symptom resolution6. PDL shows a therapeutic effect by photo-thermolysis targeting oxyhemoglobins within cutaneous vasculature78. PDL is effective for erythema, flushing, telangiectasia and even inflammatory lesions in patients with rosacea678. Biopsy specimens which were taken from patients with rosacea 3 months after PDL therapy showed that nerve fiber density and number of substance P immunoreactive nerve fibers were decreased910. However, exact relationship between this and the therapeutic effect of PDL has not been demonstrated yet.
Rosacea usually undergoes a chronic relapsing course7. It impacts on patients' quality of life and the impact is significantly influenced by their previous treatment11. This highlights the necessity of preventing recurrence, as well as relieving the symptoms when treating rosacea. There is ongoing debate over which therapy, or which combination of therapies, is the most beneficial for the patients with rosacea. Despite its frequent relapses, there are only few studies which estimate the recurrence rate of treatment modalities for rosacea. To the best of our knowledge, only one study evaluated the relapse rate of rosacea as the primary objective and there are no studies that demonstrate the recurrence rate according to the treatment modalities12.
The objective of this study was to evaluate the role of 595 nm-PDL on reducing relapses among patients with rosacea who were treated with oral minocycline.
This study was designed as a retrospective follow-up study. The study was approved by the Inha University Institutional Review Board (INHAUH 2015-03-004).
Records of all patients diagnosed with rosacea without other cutaneous disorders between January 1, 2013 and May 31, 2015 were retrieved from our electronic record system. Among them, Korean patients with rosacea who started treatment with oral minocycline with or without 595 nm-PDL by 1 dermatologist at the Inha University Hospital were evaluated retrospectively. Those who were treated with other oral therapy and light-based physical modalities or who had treatment history within 30 days of baseline (6 months in case of isotretinoin) were excluded, as were those with other health problem which could affect the skin disorder. But we didn't consider the use of skin care products.
Patients were categorized into 2 groups according to the treatment modality:
– Group 1: Oral minocycline (100 mg per day) alone
– Group 2: Oral minocycline (100 mg per day) plus 595 nm-PDL (total 2∼4 sessions)
The PDL (595 nm, VBeam; Candela/Syneron, Wayland, MA, USA) settings were: fluence, 10.0 J/cm2; spot size, 7 mm; pulse duration, 10 milliseconds; and passes, 2 with 10% overlap of treatment spots. The settings were standard subpurpuragenic settings, including published guidelines and company-recommended ones at the time of the study7.
The medical charts were reviewed. The follow-up period was 1 year from the end of the treatment. We collected the following patient information: age, sex, rosacea type, treatment modalities including oral agents, light-based physical modalities and topical agents, the treatment duration with oral minocycline, and the number of laser sessions. We didn't evaluate the severity of rosacea before and after the treatment. Treatment termination was defined as successful clearance of skin lesions and symptom with patient's agreement. Patients who did not show successful clearance were not included in this study. Recurrence was regarded as the first re-visit for the re-treatment after the treatment termination. Treatment termination and recurrence was evaluated and described on the medical chart by the dermatologist. We got the information from those who were lost to follow-up via telephone. Otherwise, they were regarded as censored observations.
Patient characteristics were compared between groups with the Mann-Whitney test or chi-square test. Time to recurrence was measured from the date of the treatment termination to first re-visit or to last follow-up. The recurrence rate was estimated using the Kaplan-Meier method, and difference of the recurrence rates between two groups was compared using the log-rank test1314. Each variable which showed a significant difference between two groups was evaluated in the simple Cox proportional hazards model. We estimated hazard ratios (HRs) and 95% confidence intervals (CIs) of risk factors for the recurrence of rosacea in the multiple Cox proportional hazards model for the variables that showed statistical significance in the simple Cox proportional hazards model. p-value less than 0.05 was deemed statistically significant. All analyses were performed using IBM SPSS Statistics ver. 19.00 (IBM Co., Armonk, NY, USA).
A total of 107 patients were included. Fifty-eight patients (50 women, 86.2%) were treated with oral minocycline alone (group 1) and forty-nine (34 women, 69.4%) were treated with oral minocycline plus PDL (group 2). A total of 43 patients among group 1 and 47 patients among group 2 were treated with oral minocycline for more than 4 weeks. Patient characteristics are shown in Table 1. There were significant differences between the groups with respect to sex (p=0.035), age (p=0.007), and the treatment duration with oral minocycline (p=0.002). There were no significant difference between the groups with respect to topical agents (p=0.625), and rosacea type (p=0.084).
A total of 45 of the 107 patients (42.1%) reported recurrence of rosacea. A total of 28 of the 58 patients (48.3%) among group 1 (the group with oral minocycline alone) and a total of 17 of the 49 patients (34.7%) among group 2 (the group with oral minocycline plus PDL) reported recurrence within 1 year. The Kaplan-Meier curve (Fig. 1) shows recurrence-free survival for the patients. The overall recurrence-free survival analysis revealed that the group with oral minocycline plus PDL was significantly different compared with the group with oral minocycline alone (p=0.011). The 1 month-recurrence free rate after oral minocycline alone was 82.8% (standard error [SE]=6.4) and 96.8% (SE=3.2) after oral minocycline with PDL, respectively. The 6 month-recurrence free rate after oral minocycline alone was 33.2% (SE=8.5) and 51.8% (SE=10.2) after oral minocycline with PDL, respectively. However, these recurrence free rates at 1 month or 6 month were not significantly different between two groups (p=0.050, 0.161 each).
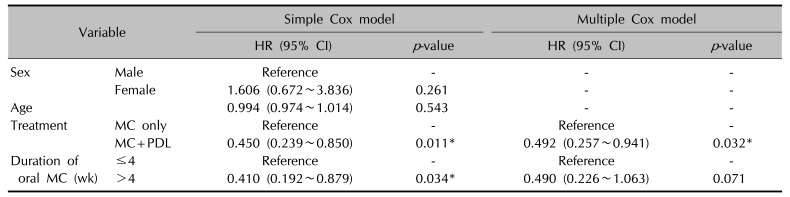
We first performed the simple Cox proportional hazards model analyses for a treatment group variable and the variables which were significantly different between group 1 and 2, such as sex, age, and treatment duration with oral minocycline (Table 1). Estimated hazards of a treatment group and duration of oral minocycline for recurrence of rosacea were statistically significant, therefore those two variables were analyzed in the multiple Cox proportional hazards model (Table 2). The multiple Cox proportional hazards model showed that PDL treatment added to oral minocycline was an important protective factor for a hazard of the recurrence of rosacea (HR, 0.492; 95% CI, 0.257∼0.941; p=0.032). The treatment duration with oral minocycline was not a significant prognostic factor for the recurrence of rosacea (p>0.05).
Although rosacea undergoes recurrent exacerbation, the relapse rate for rosacea is not well known. These frequent recurrences of rosacea affect patient compliance and make it difficult to evaluate the relapse rate for rosacea. In 1975, Knight and Vickers12 reported that relapses occurred in 24% of rosacea patients after 1 month, 60% after 6 months, 69% after 4 years off oral tetracycline (500 mg daily). There are only few studies about relapses of rosacea. This study showed that the 1 month-recurrence rate after oral minocycline alone was 17.2% and the 6 month-recurrence rate was 66.8%, which is similar to the results of previous report.
PDL treatment for rosacea improves facial flushing, redness and telangiectasia1516. A recent systemic review stated that PDL appears to be an effective treatment for acne vulgaris with high level of evidence8. This implies that PDL may be an effective treatment for rosacea patients with inflammatory lesions as well as erythema and telangiectasia. It is not established how long the treatment effect of PDL lasts. Togsverd-Bo et al.17 reported that the treatment effect of 595 nm-PDL therapy (7.5 J/cm2, 10 ms, 10 mm spot size, 2 passes) persisted for less than 3 months. In the present study, the 1 month-recurrence rate was 3.2% and the 6 month-recurrence rate was 49.2% after PDL in combination with oral minocycline therapy.
Rosacea patients usually require long-term therapy, but ideal treatment duration with oral medication for maximal treatment effect and the lowest relapse rate has not been established yet. In order to achieve substantial improvement with oral tetracycline, it has been reported that a three- or four- week treatment duration is required and 3∼5 months of treatment may sometimes be needed to clear the skin lesions318. Long-term therapy with oral antibiotics may lead to the development of antibiotic-resistant organisms. In this study, PDL used in combination with oral minocycline reduced the hazards for recurrence of rosacea. Therefore, PDL may be helpful to prevent the complications of long-term therapy with oral minocycline. Generally, two to four laser treatments are required to achieve best outcomes for rosacea6. Patients with total 2∼4 sessions of PDL were only included in this study. When we evaluated data including patients with a single session of PDL, the recurrence rates between groups were not significantly different (data not shown). It means a single laser session is not enough to see the therapeutic effect.
Topical metronidazole or calcineurin inhibitors were used to treat rosacea2; however, it is not known yet that the topical medicines can protect against recurrence of rosacea. Patients with topical medicines were also included in this study. However, the use of topical medicine turned out not to be a significant protective factor for the hazard of recurrence of rosacea (p=0.099).
To our knowledge, this is the first study to explore the relapse rate for rosacea using recurrence free survival analysis. However, there are limitations to this study. First, disease severity which may be a potential risk factor for relapses was not assessed because this was a retrospective observation study. Second, more rosacea patients with telangiectasia might have been enrolled in the PDL group. But there was no statistically significant difference of rosacea type between two groups. Therefore, our study findings should be validated according to treatment modalities for rosacea with a larger sample in future studies.
The main implication from this study is that PDL can be used added to oral minocycline to reduce relapses among rosacea patients who are undergoing minocycline treatment. This study encourages more research evaluating the relapse rates for rosacea.
References
1. Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015; 72:749–758. PMID: 25890455.
2. Korting HC, Schöllmann C. Current topical and systemic approaches to treatment of rosacea. J Eur Acad Dermatol Venereol. 2009; 23:876–882. PMID: 19508315.

3. Jackson JM, Kircik LH, Lorenz DJ. Efficacy of extended-release 45 mg oral minocycline and extended-release 45 mg oral minocycline plus 15% azelaic acid in the treatment of acne rosacea. J Drugs Dermatol. 2013; 12:292–298. PMID: 23545911.
4. Del Rosso JQ, Webster GF, Jackson M, Rendon M, Rich P, Torok H, et al. Two randomized phase III clinical trials evaluating anti-inflammatory dose doxycycline (40-mg doxycycline, USP capsules) administered once daily for treatment of rosacea. J Am Acad Dermatol. 2007; 56:791–802. PMID: 17367893.

5. Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part II. Topical and systemic therapies in the treatment of rosacea. J Am Acad Dermatol. 2015; 72:761–770. PMID: 25890456.
6. Pelle MT. Rosacea. In : Goldsmith L, Katz S, Gilchrest B, Paller A, Leffell D, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 918–924.
7. Kim TG, Roh HJ, Cho SB, Lee JH, Lee SJ, Oh SH. Enhancing effect of pretreatment with topical niacin in the treatment of rosacea-associated erythema by 585-nm pulsed dye laser in Koreans: a randomized, prospective, split-face trial. Br J Dermatol. 2011; 164:573–579. PMID: 21143465.

8. Erceg A, de Jong EM, van de Kerkhof PC, Seyger MM. The efficacy of pulsed dye laser treatment for inflammatory skin diseases: a systematic review. J Am Acad Dermatol. 2013; 69:609–615.e8. PMID: 23711766.

9. Lonne-Rahm S, Nordlind K, Edström DW, Ros AM, Berg M. Laser treatment of rosacea: a pathoetiological study. Arch Dermatol. 2004; 140:1345–1349. PMID: 15545543.
10. Salem SA, Abdel Fattah NS, Tantawy SM, El-Badawy NM, Abd El-Aziz YA. Neodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea: comparison of clinical efficacy and effect on cutaneous substance (P) expression. J Cosmet Dermatol. 2013; 12:187–194. PMID: 23992160.

11. Aksoy B, Altaykan-Hapa A, Egemen D, Karagöz F, Atakan N. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities. Br J Dermatol. 2010; 163:719–725. PMID: 20545683.

12. Knight AG, Vickers CF. A follow-up of tetracycline-treated rosacea. With special reference to rosacea keratitis. Br J Dermatol. 1975; 93:577–580. PMID: 128376.
13. Mikkelsen PR, Dufour DN, Zarchi K, Jemec GB. Recurrence rate and patient satisfaction of CO2 laser evaporation of lesions in patients with hidradenitis suppurativa: a retrospective study. Dermatol Surg. 2015; 41:255–260. PMID: 25654196.
14. Roland CL, Boland GM, Demicco EG, Lusby K, Ingram D, May CD, et al. Clinical observations and molecular variables of primary vascular leiomyosarcoma. JAMA Surg. 2016; 151:347–354. PMID: 26629783.

15. Tan ST, Bialostocki A, Armstrong JR. Pulsed dye laser therapy for rosacea. Br J Plast Surg. 2004; 57:303–310. PMID: 15145732.

16. Bernstein EF, Kligman A. Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med. 2008; 40:233–239. PMID: 18412227.

17. Togsverd-Bo K, Wiegell SR, Wulf HC, Haedersdal M. Short and limited effect of long-pulsed dye laser alone and in combination with photodynamic therapy for inflammatory rosacea. J Eur Acad Dermatol Venereol. 2009; 23:200–201. PMID: 18452529.

18. Wereide K. Long-term treatment of rosacea with oral tetracycline. Acta Derm Venereol. 1969; 49:176–179. PMID: 4184565.
Fig. 1
The Kaplan-Meier curve showing recurrence for all patients. The overall recurrence-free survival analysis revealed that group 1 was significantly different compared with group 2 (p=0.011). MC: minocycline, PDL: pulsed dye laser, Group 1: oral minocycline (100 mg per day) alone, Group 2: oral minocycline (100 mg per day) plus 595 nm-PDL (total 2∼4 sessions). *p<0.05.
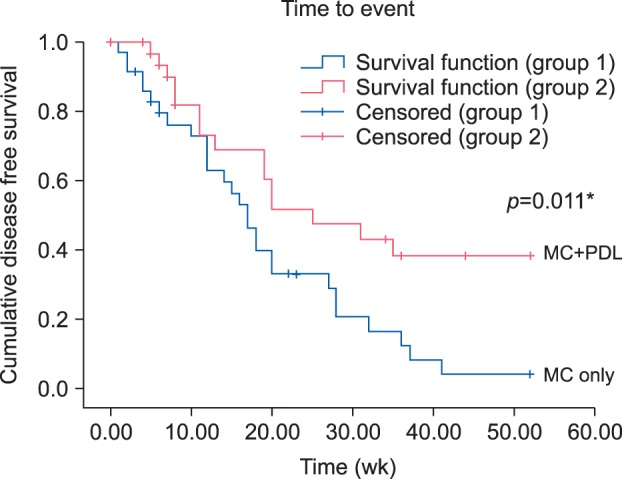
Table 1
Patient demographic characteristics
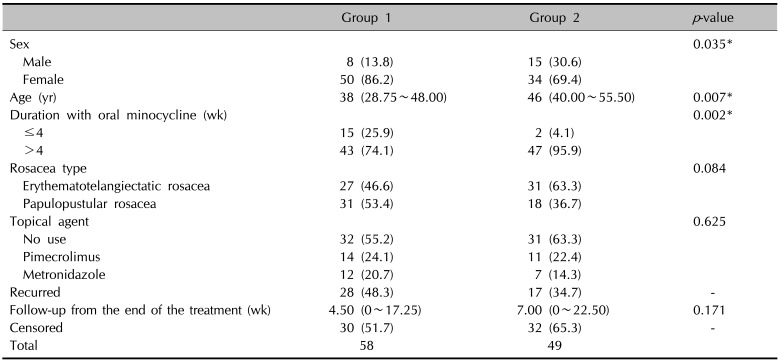
Values are presented as number (%), median (interquartile range), or number only. Group 1: oral minocycline (100 mg per day) alone, Group 2: oral minocycline (100 mg per day) plus 595 nm-pulsed dye laser (total 2∼4 sessions). p-value was obtained by chi-square test for categorical variables and Mann-Whitney test for continuous variables, as appropriate. *p<0.05.
Table 2
HRs for recurrence, estimated in Cox proportional hazards model




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download