INTRODUCTION
Plasma cell cheilitis (PCC) is a rare, idiopathic, inflammatory disease that occurs on the lip, with histological findings characteristically showing dense infiltration of plasma cells in the papillary dermis of the mucosa
123. It is also considered as a lower categorical entity that belongs to plasma cell mucositis (PCM), which involves the mucous membrane of the oral cavity and upper aerodigestive tract
45. PCC clinically presents as minutely prominent erythema or a dark-red or brownish patch or plaque with relatively clear margins, mainly in the lower lip of elderly people
126. This condition can be accompanied by erosion, ulceration, fissures, bleeding, or crusts. Spontaneous resolution of PCC is extremely rare and is known to respond poorly to traditional topical steroid treatment
7. Besides, systemic steroid ingestion, intralesional steroid injection, systemic griseofulvin administration, and local application of immunomodulatory agents such as tacrolimus and pimecrolimus, are examples of various treatments that are being attempted
68910111213.
Most of the cases of PCM have included involvement of the oral cavity and upper aerodigestive tract; therefore, several published studies have been reported in the otolaryngology and oro-maxillofacial surgery literature
4514. Otherwise, limited case series on the clinical and histopathological findings of PCC have been reported in the dermatology literature, with only a few showing immunohistochemical analysis
715. Furthermore, no guidelines were established for the management and clinical outcome prediction of PCC owing to the lack of sufficient case studies. In the present study, we described a case series of PCC, with clinicopathological features and immunohistochemical study along with a literature review.
Go to :

MATERIALS AND METHODS
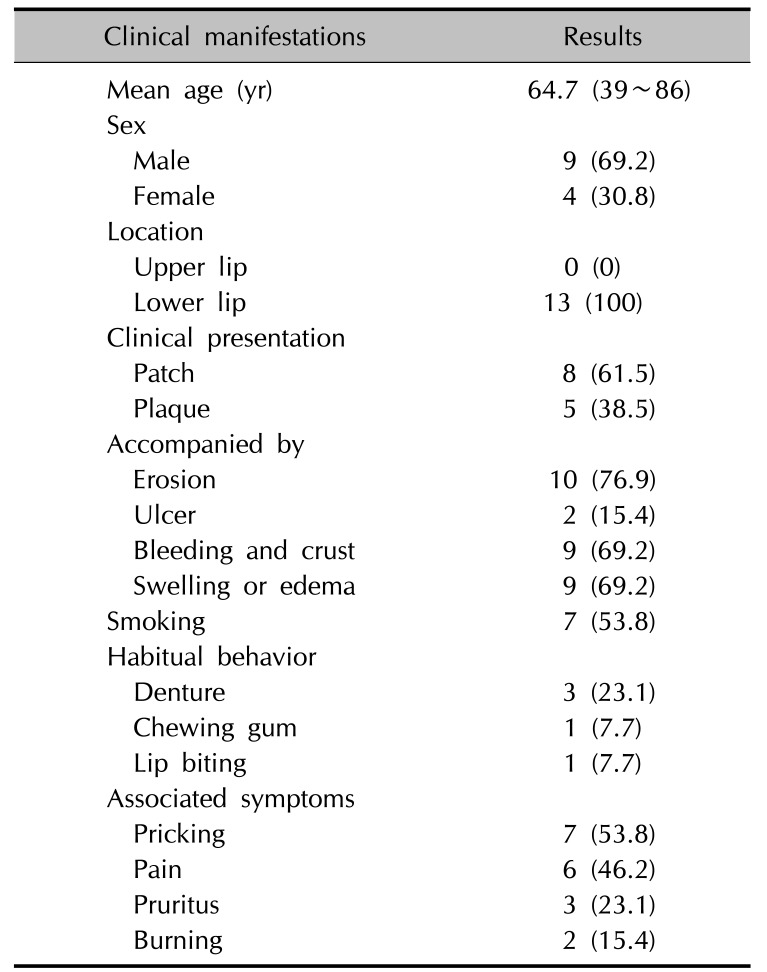
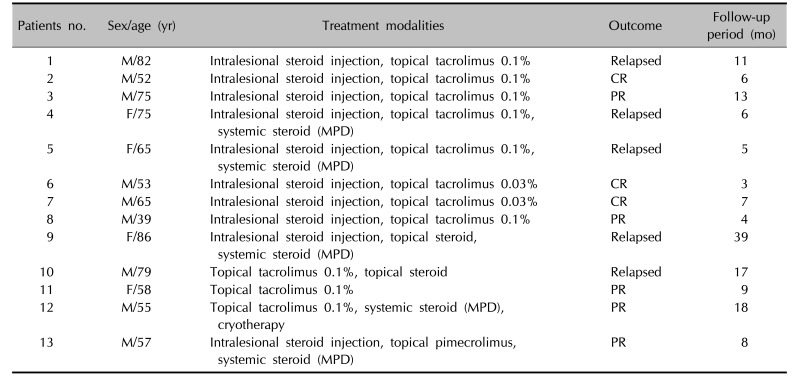
A total of 13 cases of patients diagnosed with PCC at Kangdong Sacred Heart Hospital and Hallym University Sacred Heart Hospital were retrospectively reviewed over a 6-year period from 2011 to 2016. The following clinical manifestations, including gender, age, location, presence of erosion or bleeding, smoking habit, accompanying symptoms, habitual behavior, treatment modalities, clinical outcome, and follow-up period were collected from electronic medical record and interview.
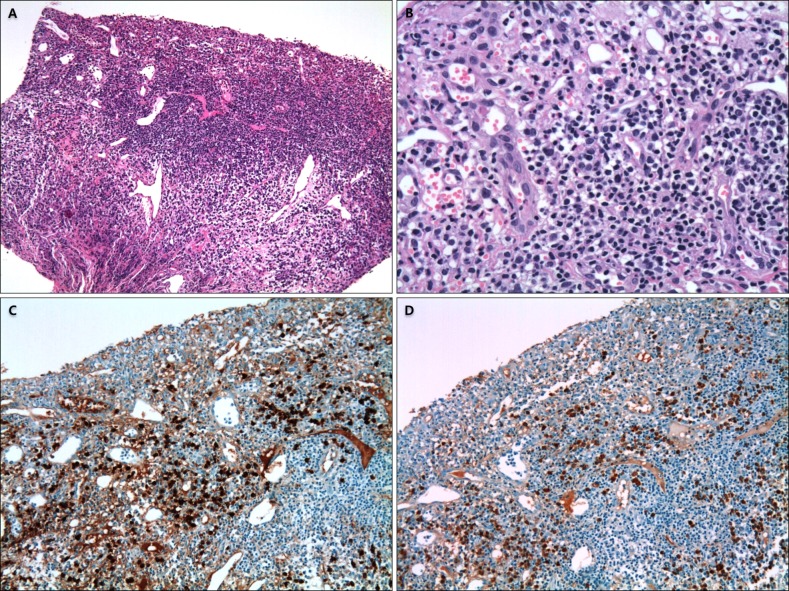
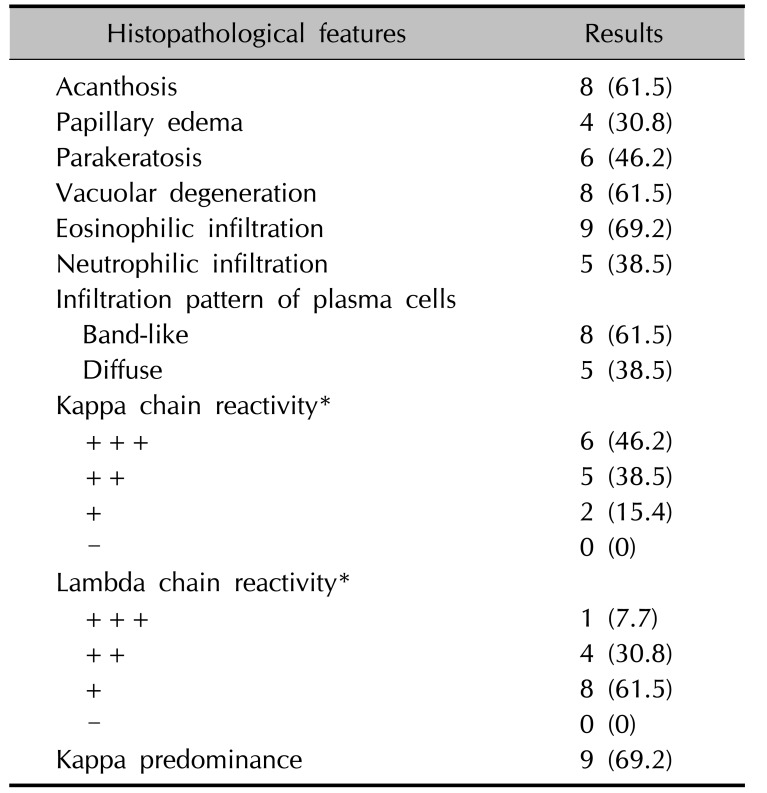
Biopsy specimens of all the enrolled patients were retrieved from the Department of Pathology and investigated independently by the three experienced dermatologists. All specimens were formalin fixed, paraffin embedded, and stained; hematoxylin and eosin (H&E) staining and immunohistochemistry analysis of kappa and lambda light chains using the Dako Autostainer (Dako, Carpinteria, CA, USA) were used based on the manufacturer and established laboratory protocols. Immunoglobulin (Ig) heavy chain gene rearrangement via polymerase chain reaction analysis was performed only in selected patients to confirm clonality of Ig heavy chain. Each slide was reviewed for the presence or absence of the following histopathological findings: acanthosis, papillary edema, parakeratosis, vacuolar degeneration or melanin incontinence, infiltration of mononuclear inflammatory cells, such as eosino phils or neutrophils, and infiltrative pattern of plasma cells.
The reactivity levels of kappa and lambda light chains based on the starting intensity were graded as follows: − (negative, no positive cells), + (weak positive, ≤25% positive cells), ++ (moderately positive, 26%~50% positive cells), and +++ (strongly positive, >50% positive cells).
Go to :

DISCUSSION
PCC is a relatively rare inflammatory disorder of the lip, characterized histologically by dense infiltration of plasma cells in the upper dermis, wherein its pathogenesis remains elusive. It is known as an oral counterpart of plasma cell balanitis (Zoon's balanitis), which was first described by Zoon
16 in 1952 as an inflammatory disorder of the glans penis, showing characteristic band-like infiltrate of plasma cells in the upper dermis. Based on White et al.
17, PCC was observed as a clinically and histopathologically identical disease developing in several orificial surfaces, such as the vulva, buccal mucosa, palate, lip, tongue, epiglottis, and larynx, and collectively known as plasma cell orificial mucositis. In addition, immunohistochemical analysis of one case in their study showed plasma cell production of both kappa and lambda chains.
Histopathologically, hyperkeratosis, dyskeratosis, intercellular edema, epidermal erosion, and vacuolar or liquefactive degeneration due to inflammatory cell infiltration in the dermo-epidermal junction can be seen in PCC
15. Many plasma cells are infiltrated in a band-like shape in the upper dermis or densely infiltrated throughout the entire dermis
123. This plasma cell infiltration in the dermis is a characteristic finding of PCC that is rarely seen in common inflammatory dermatosis. Although the pathogenesis for the plasma cell infiltration remains unknown, B-cell growth and differentiation in the mucosa and skin are suggested to be affected by T cells and macrophages
167. In the present study, majority of the cases of infiltrated plasma cells in the dermis showed polyclonality of the kappa and lambda chains in immunohistochemical stains. In accordance with previous literatures, they were also composed of cells primarily the kappa chain instead of the lambda chain
47. Aiba and Tagami
7 also demonstrated that plasma cell infiltrates in PCC were composed of IgG- and IgA-producing cells, and those are in accordance with the pattern observed in certain skin diseases, including actinic keratosis, Bowen's disease, squamous cell carcinoma, pemphigus vulgaris, and syringocystadenoma papilliferum. Interestingly, almost 70% of patients in the present study were revealed to have large amounts of admixed eosinophils with lymphoplasmohistiocytic infiltrates, which is significantly higher than those in the study by Choe et al.
15 who reported only 2 of 8 cases showing mild eosinophilic infiltration.
The etiology and pathogenesis of PCC have not been clarified yet. However, some cases reported until today were believed to be associated with frequent exposures to candy, gum, toothpaste, other foreign substances, and underlying disease, such as hypertension and metabolic abnormalities
15181920. Other cases were reported to be induced by mechanical irritation or accumulated solar damage. Choe et al.
15 particularly suggested that solar damage accumulating in the lower lip, which is a major exposed area of sunlight, could be considered as the causative agent in all observed cases. All patients in the present study also developed PCC in the lower lip; therefore, solar damage due to chronic sun exposure is speculated as an important cause such as in actinic cheilitis. Moreover, 2 of our patients had habitual behaviors, such as chewing gum and lip biting, and 3 of our elderly patients consistently used dentures, which can play an uncertain mechanical role in the development of PCC.
To date, PCC is regarded as a type of PCM. Solomon et al.
4 summarized 22 studies of PCM, which encompass the plasma cell-rich condition occurring on all locations of the upper aerodigestive tract, including the lips, mouth, tongue, gingiva, palate, larynx, pharynx, and even the bronchial tree. The mean age of those patients was 56.6 years, which is slightly younger than that of our patients. They also described that majority of PCM cases are associated with a synchronous or metachronous autoimmune or immunologically mediated disease; however, none of our patients were diagnosed with immune disorders. The classic clinical presentation of PCM is known to be various morphologies, such as papillomatous, cobblestone, nodular, or velvety, which are different from PCC, which usually shows patches and plaques with swelling rather than warty or lobulated surface contour. It might result from the different mucosal characteristics located in the inner or outer sites of the body. However, distinct clinical features of PCC as a subordinate disease of PCM should be investigated further.
The clinical course of PCC can be quite prolonged. Moreover epidermal neoplasm, which is composed of plasma cell infiltrates because mononuclear inflammatory cells, may affect the production of factors that induce the peculiar polyclonal plasma cell infiltration
7. Although PCC is considered a benign disorder with long stability and hardly progresses to malignancy, the treatment is often challenging
4. Some authors have shown that topical and intralesionally administered steroids and topical immunomodulatory agents, such as tacrolimus and pimecrolimus, were effective for the clearing the lesions, whereas others have found that most of the topical therapies were ineffective in their patients and have recommended alternatives, such as surgical excision, radiation therapy, laser therapy, electrocauterization, and cryosurgery
69101112132122. In the present study, majority of the patients were treated by a combination of intralesional steroid injection and topical tacrolimus, with multi-sessions at an interval of 2 weeks. Intralesional steroid injection is known to have an anti-inflammatory property as well as to increase the effects of topical agents by bypassing the epidermal barrier zone
12. Topical tacrolimus preparations, which are being used to treat inflammatory dermatosis, inhibit the signal transduction of the T lymphocytes
91011. However, some patients in the present study responded poorly to those treatment modalities because of the unclear etiology or resistant factor, such as acanthosis/hyperkeratosis, depth and heaviness of the infiltrates, and accompanying underlying disease. Therefore, well-designed studies on the affecting triggers to manage the clinical course of PCC with long-term follow-up periods are required. Additional investigative analysis to identify accurate functional pathogenesis on the plasma cells should be warranted.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download