INTRODUCTION
Various radiation dose reduction techniques have been developed and used to minimize computed tomography (CT) radiation dose while maintaining diagnostic image quality which is especially crucial in pediatric CT (
123). Among them, attenuation-based tube current modulation technique is useful to reduce radiation dose without substantial increase in image noise (
4567). To use the technique properly in clinical practice, we should first recognize the unique relationships between image noise and image quality indicators between different tube current modulation techniques (
8). In all systems, a user-determined image quality level is required for CT scanning with tube current modulation. In body size-adapted CT protocols particularly important in children having a great diversity in body size and habitus, the user-determined image quality level should be adjusted by using one of various body size indices, including body weight, body mass index, cross-sectional dimensions, and body attenuation. In this regard, cross-sectional dimensions, such as area and circumference, are superior to body weight in body size-adapted CT radiation dose optimization (
910). On the other hand, patient attenuation as estimated from CT scout image may be used to determine body size, but proper calibration process, no use of edge-enhancing filters, and exact patient centering are required to avoid errors in the size estimation (
111213). Consequently, the axial CT image-based method is easier and straightforward in estimating patient attenuation than the CT scout image-based method (
1213).
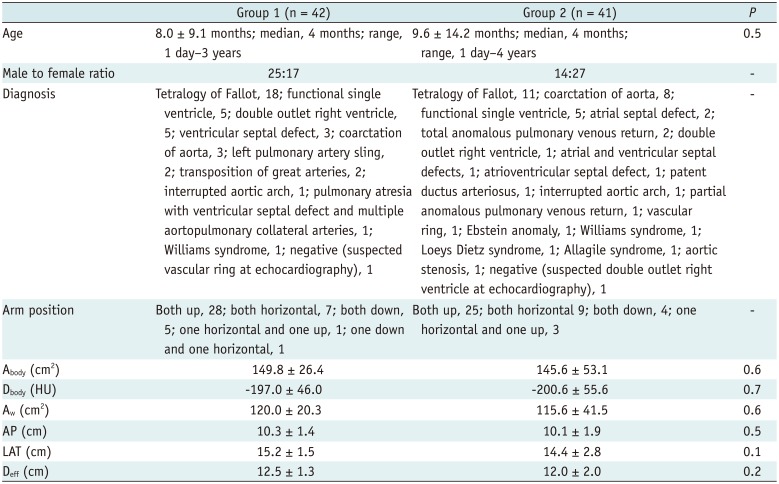
In a prior study (
14), volume CT dose index (CTDI
vol) as the user-determined image quality indicator was individually determined by the cross-sectional area (A
body) and mean body density (D
body), and more uniform image noise of contrast-enhanced pediatric chest CT could be achieved when scanned with a combined tube current modulation. In the study, the user-determined CTDI
vol value was entered after the scan range adjustment (
14). However, it may be more appropriate from the point of view of CT radiation dose optimization if the CTDI
vol value was first entered at the same axial position where the A
body and mean D
body were calculated and the scan range was extended later from the minimum to the full. Therefore, this study was aimed to determine whether the CTDI
vol value based on A
body and mean D
body in pediatric cardiothoracic CT with tube current modulation was better to be entered before or after scan range adjustment for CT radiation dose optimization.
Go to :

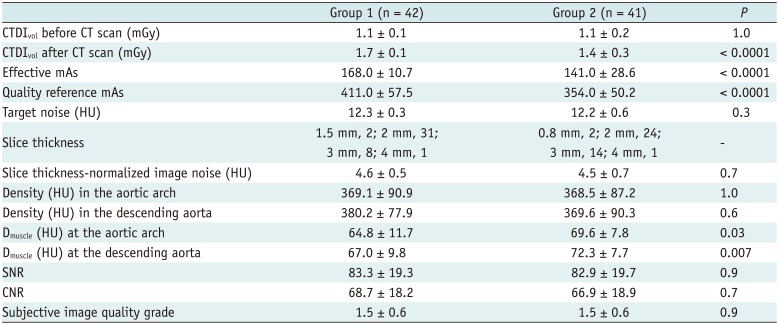
DISCUSSION
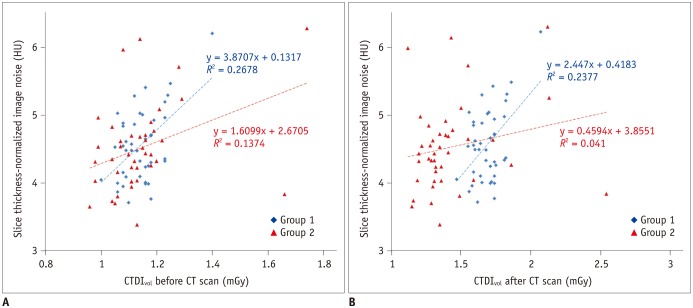
This study demonstrated that an additional reduction of radiation dose with comparable image noise could be achieved simply by changing the input steps of a user-determined radiation dose level in pediatric cardiothoracic CT with tube current modulation. This improved CT radiation dose optimization is attributable to a better adaptation of radiation dose to individual patient size and body habitus by using tube current modulation function more effectively in the new method (group 2). In the previous method (group 1), the CTDI
vol determined by a single axial CT image was used for the full scan range of cardiothoracic CT, which may be suboptimal in the optimization point of view and result in a CT radiation dose slightly higher than necessary for the user-determined image quality level. In contrast, the CTDI
vol was initially entered for the minimal scan range at the same position as the axial CT image where the CTDI
vol was calculated and the minimal range then was longitudinally extended to the full scan range of cardiothoracic CT in the new method (group 2). Although CT scanning is commonly performed with tube current modulation (
45678), such details of the input steps of radiation dose have not been evaluated or described. In this respect, the aforementioned result of this study is obviously a small step forward in CT radiation dose optimization that can be easily and widely used in our clinical practice. A lower or insignificant correlation between radiation dose and image noise in the group 2 than in the group 1 (
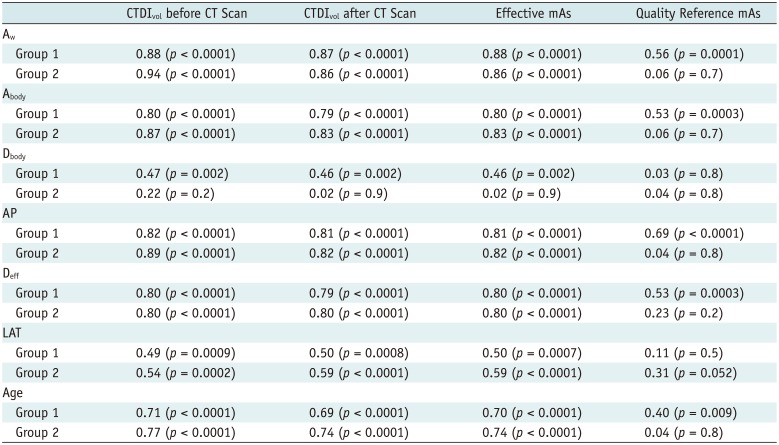
Fig. 5) also would suggest a better CT radiation dose adaptation to patient size and habitus in group 2.
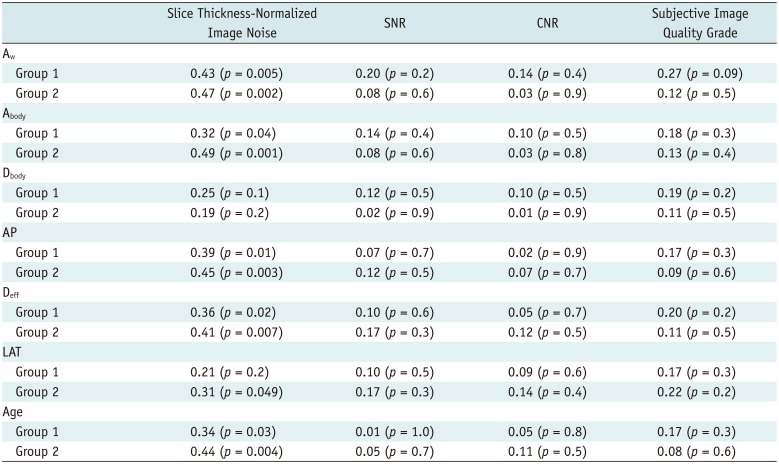
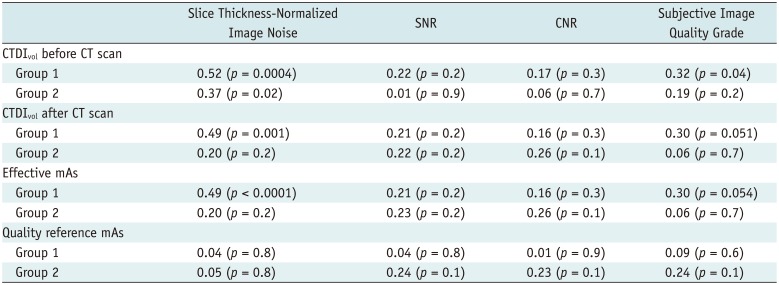
Among body size indices evaluated in this study, A
w showed the highest (
r = 0.86–0.94) correlations with CTDI
vol values before and after the CT scan as well as effective mAs in both groups, particularly between A
w and CTDI
vol before the CT scan in the group 2 (
r = 0.94). In this regard, the single best variable (A
w), instead of using a combination of two variables (A
body and mean D
body) as previously reported (
14), can be used to develop a new best fit equation using this high linear relationship between the two for estimating a better body size-adapted CT radiation dose prior to CT scanning. Compared with A
w in this study, A
body showed a lower correlation (
r = 0.73;
p < 0.001) in the group using 80 kVp in the previous study (
14). On the contrary, D
body showed no significant correlation in this study and the previous study (
14). Recent studies also have shown that an attenuation-based method, such as A
w or water equivalent diameter, is superior to geometric parameters. This is especially true in the thoracic region demonstrating a greater difference in CT numbers than other regions due to the inclusion of the lung, for estimating patient size that can be used to determine optimal CT radiation dose (
121317181920).
The attenuation-based patient size can be obtained from CT scout image or axial CT images. The method using CT scout image is limited by a complicated calibration process of pixel values using a series of water phantoms, a non-edge enhanced image filter that are not currently available from all manufacturers, and magnification errors caused by patient miscentering (
13). On the other hand, the method using axial CT images can only be performed after the CT scan is finished and, therefore, cannot be used to determine a user-defined image quality level prior to the CT scan (
13). Moreover, frequent image truncation on clinical CT images leads to incomplete extraction of the whole patient cross section (
20). The CT image-based method requires a threshold-based segmentation to extract A
body and D
body necessary for calculating A
w as in this study. When manual drawing of a region of interest was performed to include the whole patient cross section for the axial CT image, care was taken to exclude the patient table and other attenuating materials in this study. In the previous study (
13), inclusion of the patient table led to overestimation of an attenuation-based patient size measure, particularly for pediatric patients due to their relatively small size, up to 45.7%. On the contrary, the patient table was not included in the patient cross section in this study by using a careful manual drawing of a region of interest. As a result, potential overestimation of A
w could be completely avoided. It is noteworthy that the manual drawing of a region of interest necessary for excluding the patient table, however, makes automated calculations of an attenuation-based patient size difficult.
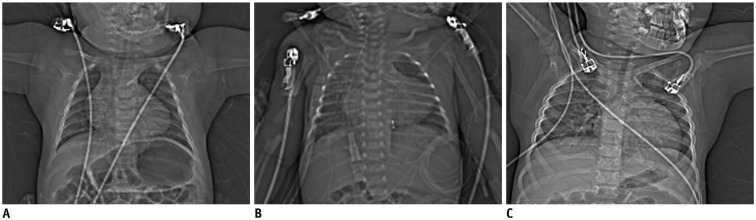
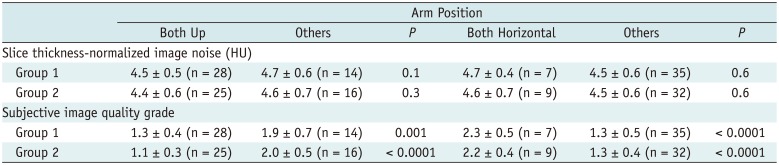
In this study, subjective image quality in the shoulder regions was frequently degraded by a horizontal arm position. Arm position on a CT scout image is important to avoid an unexpectedly high radiation dose from a CT scan with tube current modulation. In this regard, the position with both arms up is recommended for this reason (
6721). Nonetheless, both arms could not be raised up in all the patients in this study due to a risk of patient movement and awakening when both arms were raised up in some patients (34% in the group 1 and 39% in the group 2). Increased radiation dose, caused by arm position on CT scout image, could not be evaluated because patients with different arm positions had different patient sizes and body densities in this study. The degraded image quality caused by a horizontal arm position and localized in the shoulder regions in this study was thought to result from tube current saturation in those regions. Tube current saturation occurred in thick body regions, e.g., the shoulder, also diminishes the dose saving effect of tube current modulation especially at low kVp or fast scan speed (
52223). No significant effect of arm position on image noise in this study seemed to be misleading because image noise was not measured in the shoulder regions showing the degraded image quality.
A recent multi-center, multi-vendor study on radiation dose of pediatric cardiac CT (
24) clearly demonstrates a further demand for CT radiation dose optimization. In this regard, the results of this study would be beneficial in the optimization process. The previous study using the same best fit equation (
14) showed considerably higher image noise (approximately 13.7 HU) than this study (approximately 4.6 HU). The lower image noise in this study might be mainly due to the use of iterative reconstruction algorithm instead of conventional filtered back projection. Based on the results of this study, radiation dose of pediatric cardiothoracic CT in our institution was reduced by 15%. In addition, it is planned to use the CTDI
vol value individually determined prior to CT scan by using the A
w only rather than a combination of A
body and mean D
body for further CT radiation dose optimization because the former showed the highest correlation with X-ray outputs of CT scans in this study.
This study has several limitations. First, the unpaired comparison between the two groups in this retrospective study might introduce an imperfect statistical comparison, compared with paired comparison. However, paired comparison between the two methods in the same patient may be regarded unethical in young children because two CT exams in the same patient inevitably double radiation risks. As an alternative, the paired comparison can be tested by using an anthropomorphic phantom in a future study. Nevertheless, the unpaired comparison in this study might not cause a substantial statistical error because the independent variables including patient age, body parameters, and arm position on a CT scout image were comparable between the two groups. Second, to ensure patient centering in vertical direction, a lateral scout image is very useful (
61619). Because only anterolateral scout image was used in this study, a potential error in patient centering might affect the CT X-ray outputs and radiation exposure to patient in this study using tube current modulation and a bowtie filter (
1625). However, technologists used the same protocol for positioning patients in the isocenter in the two groups in this study. A radiolucent pad was additionally placed on the CT table to compensate for a low vertical position of a smaller patient in this study because the low position was reported to be particularly pronounced in smaller children (
16). Furthermore, the center of body actually depends on the z-location and therefore cannot be at the same isocenter for the entire longitudinal scan range (
16). Third, the results of this study were obtained in a single CT manufacturer. Therefore, different results may be obtained in others. Last, size-specific dose estimate or effective dose of pediatric cardiothoracic CT was not calculated because this study was not aimed to estimate CT radiation dose but to compare the two different methods in CT radiation dose optimization.
In conclusion, the CTDIvol entered before scan range adjustment provides a significant radiation dose reduction (18%) with comparable image noise in pediatric cardiothoracic CT with tube current modulation, compared with that entered after scan range adjustment.
Go to :








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download