Abstract
This paper presents a case of an early malignant transformation of untreated ulcers in a patient with diabetes. This case shows that Marjolin's ulcer can occur not only after chronic injury, but can also develop in the early stages after the onset. Hence, an early biopsy for diabetic foot ulcers that fail to heal with acute treatment can enable an earlier diagnosis and treatment without amputation, resulting in a better quality of life for the patient.
Marjolin's ulcers reflect malignant changes arising from a chronic injury or inflammatory lesion. The most common cause is a burn or scar.1) However, this aggressive condition has also been found in a variety of cases including vaccinations, snake bites, osteomyelitis, pressure sores, spinal injuries, pilonidal abscesses, factitious dermatitis, and venous ulcers.2) Marjolin's ulcers primarily appear as squamous cell carcinomas, followed by basal cell carcinomas. They are also diagnosed as melanomas and sarcomas, albeit rarely.3)
Marjolin's ulcer can occur in all age groups. Fleming et al.4) reported that the average age at which a burn scar transforms into cancer is 58 years. In addition, it has been reported that the age of the injury is more closely associated with malignant changes than the age of the patient. Marjolin's ulcers can be classified into acute or chronic types depending on whether they occur within 1 year or after 1 year. The average latent period of the chronic type was reported about more than 30 years.25) Here, we present a case of Marjolin's ulcer that developed from early stage untreated diabetic foot ulcer.
This case report was approved by the Institutional Review Board of Ajou University Hospital (AJIRB-MED-EXP-17-422). Informed consent has been obtained from the patient for publication, including any necessary photographs. A 54-year-old woman presented with right heel ulceration that had been aggravating her for 2 years. By that time, she had been receiving treatment for diabetes mellitus for 10 years and had developed an ulcer without specific trauma. Her ulcer was deep enough to expose the calcaneus, and simple radiography of the hind foot revealed calcaneus fracture and gas inside the Achilles tendon (Fig. 1). A subsequent blood test and magnetic resonance imaging scan confirmed osteomyelitis of the calcaneus and metatarsal bones, and Achilles tendonitis (Fig. 2). Repeated wound irrigation and resection of necrotic and infected Achilles tendon relieved the patient's symptom (Fig. 3). However, a follow-up examination did not take place because of patient's refusal.
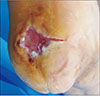
Two years later, the patient was readmitted with the chief complaint of an uncured ulcer in the same area as before. As the ulcer did not improve, she had undergone a skin graft at another hospital 1 year before readmission to our institution. Skin grafting failed to heal the ulcer completely as all grafts were destroyed. However, compared to the ulcer's previous status at discharge from our hospital, the ulcer's size was reduced and granular tissue had formed (Fig. 4). Histopathologic examination of the ulcer area confirmed squamous cell carcinoma (Fig. 5), and magnetic resonance imaging and positron emission tomography-computed tomography scans were performed (Fig. 6). The carcinoma had invaded the calcaneus bones and metastasized to the inguinal region and popliteal lymph nodes. Therefore, we performed lower extremity amputation, which was followed by chemotherapy. However, the patient was suffered from progressive lung metastasis and multiple bone metastasis.
We encountered a rare case of Marjolin's ulcer that had developed early in a patient with a diabetic foot. The association between untreated chronic skin scars and the onset of a malignant tumor has been well established in the literature. In general, Marjolin's ulcer tends to occur when scars are left untreated for more than 30 years.25) Marjolin's ulcer most commonly refers to a squamous cell carcinoma,3) and burns are considered the most common cause of this condition.12) A case of Marjolin's ulcer in a patient with a diabetic foot has been reported, but it occurred 60 years after a scar was formed.6) In our case, the diabetic foot ulcer was confirmed to be a metastasized, infiltrative squamous cell carcinoma within 2 years after onset.
Pathologically, Marjolin's ulcers present as infiltrative/ulcerative and exophytic/papillary types. The ulcerative type is more common and its metastases are frequently observed. Marjolin's ulcer results from a complex process involving various factors, including chronic stimulation, avascularity of scar, toxins released by damaged tissues, immunologic factors, and repeated trauma.2) It usually presents clinically as a flat and ulcerative lesion with a surrounding area that is high and solid. Less frequently, it manifests as an exophytic lesion that is similar to granular tissue.789) Given the nature of diabetic foot wherein ulcers do not go away until they are completely cured, it was hard to suspect carcinoma when the patient was initially hospitalized. Even two years later, the patient did not show any clinical abnormalities except the uncured ulcers and granulation tissue.
Extensive local dissection with a safety margin of 2 cm or wider is the preferred treatment for Marjolin's ulcers.789) Skin grafting is also actively considered for skin lesion reconstruction. Although preventive lymph node dissection is not recommended, some researchers prefer the technique due to the aggressive nature of Marjolin's ulcers.10) Amputation can be a controversial treatment. However, this surgical approach may be necessary given the high risk of metastasis in Marjolin's ulcers located on the extremities. Local dissection alone cannot be an appropriate treatment option in cases of tumor invasion into bones or joints and unresectable tumors. We performed lower-extremity amputation to remove squamous cell carcinoma that had invaded the calcaneus bone.
In our case, the ulcer did not heal despite aggressive treatment during two months of initial hospitalization. We therefore recommend early biopsy to identify any malignancy if a scar is poorly responsive to treatment. Herein, we present a case of early malignant transformation of untreated ulcers in a patient with a diabetic foot. Because of multiple metastases, we performed lower extremity dissection followed by chemotherapy. In line with the increasing prevalence of diabetes, the number of diabetic patients who are not properly treated or develop treatment-resistant foot ulcers is expected to rise due to social or environmental reasons. Although Marjolin's ulcer commonly occurs after chronic injury, it can develop in an acute situation as shown in this study. We therefore recommend an early biopsy for diabetic foot ulcers that fail to heal with acute treatment. Such an approach will help clinicians reach an accurate diagnosis, decide a treatment strategy, and eventually, improve a patient's quality of life.
Figures and Tables
 | Figure 1Initial ankle lateral radiograph showing calcaneal destruction with Achilles tendon gas formation. |
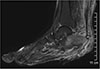 | Figure 2Magnetic resonance imaging showing bone marrow edema and enhancements at the calcaneus, cuboid bone, and navicular bone, and partial tear and severe tendinitis at the Achilles tendon. |
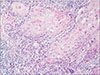 | Figure 5Pathological findings. Low-power field of H&E stained tissue revealed that the ulcer area showing invasive squamous cell carcinoma, well differentiated. |
 | Figure 6Evaluation of the metastasis. (A) Magnetic resonance imaging showing an ill-defined enhancing lesion sized 3.6×1.3×5.7 cm, the sole of the foot, and infiltration of the calcaneal tuberosity (arrow). Positron emission tomography/computed tomography scan showing inguinal (B) and popliteal (C) lymph node metastasis. |
References
1. Ozek C, Cankayali R, Bilkay U, Guner U, Gundogan H, Songur E, et al. Marjolin's ulcers arising in burn scars. J Burn Care Rehabil. 2001; 22:384–389.

2. Elkins-Williams ST, Marston WA, Hultman CS. Management of the chronic burn wound. Clin Plast Surg. 2017; 44:679–687.

3. Spring PM, Myers JN, El-Naggar AK, Langstein HN. Malignant melanoma arising within a burn scar case report and review of the literature. Ann Otol Rhinol Laryngol. 2001; 110:369–376.

4. Fleming MD, Hunt JL, Purdue GF, Sandstad J. Marjolin's ulcer: a review and reevaluation of a difficult problem. J Burn Care Rehabil. 1990; 11:460–469.
5. Oruç M, Kankaya Y, Sungur N, Özer K, Işık VM, Ulusoy MG, et al. Clinicopathological evaluation of Marjolin ulcers over two decades. Kaohsiung J Med Sci. 2017; 33:327–333.

6. Scatena A, Zampa V, Fanelli G, Iacopi E, Piaggesi A. A metastatic squamous cell carcinoma in a diabetic foot: case report. Int J Low Extrem Wounds. 2016; 15:155–157.
7. Copcu E. Marjolin's ulcer: a preventable complication of burns? Plast Reconstr Surg. 2009; 124:156e–164e.

8. Pekarek B, Buck S, Osher L. A comprehensive review on Marjolin's ulcers: diagnosis and treatment. J Am Col Certif Wound Spec. 2011; 3:60–64.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download