Abstract
Multiple myeloma (MM) can be defined as a malignancy with monoclonal plasma cell proliferation. A 66-year-old man presented with pruritic erythematous to purplish plaque grouped nodule with black pigmentations and purpura on the right forearm. The patient was diagnosed with MM about five years prior to the visit at our hospital. Erythematous plaque on his right arm grew rapidly in size over one month and appeared about seven months after the fracture surgery. Skin biopsy showed multiple plasma cell infiltration with monoclonality for lambda light chain, which was consistent with cutaneous plasmacytoma. The patient refused to be treated and died two months later. We herein report an interesting case of cutaneous plasmacytoma at the surgical site of fracture repair.
Multiple myeloma (MM) is a hematologic malignancy involving proliferation of monoclonal plasma cells1. The disease is often confined to the bone and bone marrow, but other organ involvement can sometimes occur1. MM occurring in organs besides the bone or the bone marrow is called the extramedullary plasmacytoma, and MM occurring as a result of metastasis is called the metastatic plasmacytoma or the secondary extramedullary plasmacytoma. Few cases of MM occurring at sites of trauma and surgery have been reported, suggesting trauma-specific plasma cell migration1. We herein report an interesting case of secondary cutaneous plasmacytoma at the surgical site of fracture repair.
A 66-year-old man visited a local hospital complaining of dizziness and was diagnosed with MM about five years ago. Quantitative immunoglobulins from serum revealed total IgA level of 6,340 mg/dl (normal 68~378 mg/dl) with decreased IgG and IgM levels. Both serum and urine immunofixation showed monoclonal gammopathy of IgA, lambda type. A bone marrow aspirate demonstrated 60% plasma cell infiltration, which confirmed a diagnosis of IgA lambda MM. The patient received two cycles of cyclophosphamide, dexamethasone, and thalidomide chemotherapy followed by autologous bone marrow transplantation and autologous peripheral blood stem cell transplantation. However, MM recurred after eight months with 11.2% of plasma cells in the bone marrow and eight courses of velcade and dexamethasone (VD) chemotherapy were conducted over nine months. And the MM recurred once again in the bone marrow and the mandible, so he received additional radiotherapy (RTx) on his mandible for ten times. After his RTx, another VD chemotherapy regimen was added to his therapy but the disease did not regress.
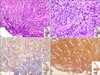
The patient presented with pruritic erythematous to purplish, rapidly growing, multiple grouped nodule with black pigmentations and purpura on the right forearm over one month (Fig. 1). Eight months before his skin lesions appeared, he underwent open reduction and internal fixation with plates and screws for fracture on his right forearm. Histopathologically, epidermal thinning and rete ridge flattening were observed without plasma cell infiltrationand dermal separation probably occurred as an artifact. Atypical cells with hyperchromatic nuclei and mild degree of mitoses and vessel dilatation are dispersed throughout dermis but more prominent in deeper dermis. Multiple plasma cell infiltration and necrosis were found in dermis (Fig. 2A, B) with monoclonality for lambda light chain (Fig. 2C), which was consistent with cutaneous plasmacytoma. Additional immunohistochemical stains such as CD3, CD20, CD56, CD45, pan CK, CK20, CK7, S-100 protein, chromogranin, synaptophysin, TTF-1, and EBER were all negative in tumor cells. The cells were stained positive for CD138 (Fig. 2D). The patient refused to be treated and died two months later.
MM can be defined as a malignancy with monoclonal plasma cell proliferation123456. MM is often diagnosed by following criteria: i) increased levels of monoclonal immunoglobulin in the urine and/or serum, ii) presence of plasmacytes in the bone marrow, and iii) evidence of lytic lesions in bones. Our patient showed monoclonal gammopathy of IgA, lambda type in both urine and serum and had 60% of plasma cells in the bone marrow. Although lytic bone lesions were not evident, he could be diagnosed with MM. The disease is often confined to the bone and bone marrow, however other systemic organ involvement can occur1.
MM occurring in tissues other than bone and bone marrow are called extramedullary plasmacytoma78910. It can also be defined as aggregates of plasma cells showing monoclonality occurring within soft tissue. About 7% of patients diagnosed with MM have extramedullary plasmacytoma at the time of diagnosis, and about additional 6%~7% of MM patients can have extramedullary plasmacytoma over the course of disease7. Cutaneous plasmacytoplasma can occur from hematogenous spread or infiltration of plasma cells from adjacent structures such as bones. It usually occurs in patients with aggressive or highly progressive form of MM and can be divided into primary and secondary. Primary cutaneous extramedullary plasmacytoma is when plasma cells infiltrate skin without the involvement of bone marrow. Secondary cutaneous extramedullary plasmacytoma can occur from metastasis from MM or from primary extramedullary plasmacytoma of other tissues1112. In our case, the patient had secondary cutaneous extramedullary plasmacytoma which occurred from direct spreading of MM at the surgical repair site.
Differential diagnoses include cutaneous plasmacytosis and plasmablastic lymphoma. Cutaneous plasmacytosis shows positive results in CD138 and has polyclonality in cells and in our case, the cells were positive for CD138 but showed monoclonality for lambda. And in plasmablastic lymphoma, skin lesions typically appear as localized, single or multiple, asymptomatic red papules or nodules. Histologically, large-sized cells which may resemble immunoblasts are diffusely infiltrated in the dermis and are stained positive for CD138 and show monoclonality, but are negative for CD56 and positive for Epstein-Barr virus RNA.
Initially, he responded well to chemotherapy, but lesions recurred and even metastasized to mandible. And after two repeated fractures and surgical repairs on his right forearm, cutaneous lesions appeared at the exact surgical site. This could be due to the direct spreading of tumor cells from surgical manipulation. Metastasis of tumor at surgical sites can occur by different mechanisms. It may be due to etiologic factors of local surgical site such as direct wound contamination and manipulation of tumor cells and systemic condition of the patient such as alteration in immune response713. A theory has been proposed to explain the immunologic process of plasmacytoma metastasis at wound sites after chemotherapy regimen. After a course of high-dose induction chemotherapy, myeloma cells with CXCR-4 chemokine receptor survive. A strong immune cell attractant called stroma cell-derived factor-1 (SDF-1), is a ligand for CXCR-4 chemokine receptor and expressed higher in sites of trauma and inflammation. Trauma to skin or subcutaneous tissue will result in higher levels of local SDF-1, thus attracting CXCR-4-positive cells to these sites7. And this will induce release of inflammatory cytokines, leading to increment of plasma cells and tumor formation7.
Few cases of cutaneous plasmacytomas at trauma sites have been reported. Two cases have been reported at the site of venous catheter insertion17 and three case occurred at the pacemaker implantation site141516, and one occurred at the fracture site17. In previously reported case of cutaneous plasmacytoma at the fracture site, the skin lesion appeared as erythematous nodule within few weeks after the surgery17. However, in our case, the skin lesion appeared more aggressive with grouped nodules and purpura. The lesion rapidly grew in size over eight months. Four out of seven patients in these cases died from rapid progression of the disease. Concurrent chemoradiation therapy is considered a treatment of choice in patients with extensive involvement7101213. We herein report an interesting case of cutaneous plasmacytoma at the surgical site of fracture repair.
Figures and Tables
References
1. Rosenblum MD, Bredeson CN, Chang CC, Rizzo JD. Subcutaneous plasmacytomas with tropism to sites of previous trauma in a multiple myeloma patient treated with an autologous bone marrow transplant. Am J Hematol. 2003; 72:274–277.

2. Kato N, Kimura K, Yasukawa K, Aikawa K. Metastatic cutaneous plasmacytoma: a case report associated with IgA lambda multiple myeloma and a review of the literature of metastatic cutaneous plasmacytomas associated with multiple myeloma and primary cutaneous plasmacytomas. J Dermatol. 1999; 26:587–594.

3. Trullemans F, Schots R, Storme G, Camp BV. Late and localized extramedullary relapse of a light chain kappa myeloma after syngeneic bone marrow transplantation. Bone Marrow Transplant. 2000; 25:115–117.

4. Requena L, Kutzner H, Palmedo G, Calonje E, Requena C, Pérez G, et al. Cutaneous involvement in multiple myeloma: a clinicopathologic, immunohistochemical, and cytogenetic study of 8 cases. Arch Dermatol. 2003; 139:475–486.
5. Malysz J, Talamo G, Zhu J, Clarke LE, Bayerl MG, Ali L, et al. Cutaneous involvement in multiple myeloma (MM): a case series with clinicopathologic correlation. J Am Acad Dermatol. 2016; 74:878–884.

6. Bayer-Garner IB, Smoller BR. The spectrum of cutaneous disease in multiple myeloma. J Am Acad Dermatol. 2003; 48:497–507.

7. Gaba RC, Kenny JP, Gundavaram P, Katz JR, Escuadro LR, Gaitonde S. Subcutaneous plasmacytoma metastasis precipitated by tunneled central venous catheter insertion. Case Rep Oncol. 2011; 4:315–322.

8. Patterson JW, Parsons JM, White RM, Fitzpatrick JE, Kohout-Dutz E. Cutaneous involvement of multiple myeloma and extramedullary plasmacytoma. J Am Acad Dermatol. 1988; 19:879–890.

9. Yoon YH, Cho WI, Seo SJ. Case of multiple myeloma associated with extramedullary cutaneous plasmacytoma and pyoderma gangrenosum. Int J Dermatol. 2006; 45:594–597.

10. Jorizzo JL, Gammon WR, Briggaman RA. Cutaneous plasmacytomas. A review and presentation of an unusual case. J Am Acad Dermatol. 1979; 1:59–66.
12. Santos G, Sousa L, Fernandes T, João A. Case for diagnosis. Cutaneous involvement associated to multiple myeloma. An Bras Dermatol. 2014; 89:173–174.
13. Ah-Weng A, Charles-Holmes R, Rose P, Basu S, Marsden JR, Sanders DS. Multiple cutaneous plasmacytomas following an autologous peripheral stem cell transplant. Clin Exp Dermatol. 2002; 27:293–295.

14. Li A, Chen A, Gallagher M, Kaczmarek P, Tinwell B, Sneddon J, et al. Primary cutaneous plasmacytoma occurring after pacemaker implantation and recurring in scar tissue. Dermatol Online J. 2013; 19:3.

15. Hamaker WR, Lindell ME, Gomez AC. Plasmacytoma arising in a pacemaker pocket. Ann Thorac Surg. 1976; 21:354–356.

16. Sasaki M, Katoh Y, Niwakawa M, Andoh A, Hodohara K, Fujiyama Y, et al. Multiple myeloma with a mass formation in a pacemaker pocket. Rinsho Ketsueki. 1992; 33:1747–1752.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download