INTRODUCTION
Nevus of Ota (NO), or oculodermal melanocytosis, affects about 0.02%~0.8% of Asians. However, it is rarely present in white populations
12. Pathologically, it is a dermal melanocytic hamartoma that presents with unilateral or bilateral, brown or blue discoloration on the facial skin innervated by the trigeminal nerve
23. To date, a variety of treatments for this ‘infamous’ patch on the face have been introduced
4. In the early phase, cryosurgery, surgical excision, skin grafting and dermabrasion are typically employed
5. Since the development of laser technology, several lasers have been introduced into the treatment of benign pigmentary lesions. Notably, Q-switched (QS) laser systems have gained popularity in the treatment of NO as they produce less scarring and better outcomes
6. Nonetheless, the introduction of various treatment options for NO have made it difficult for dermatologists to choose the best solution in practice.
Tanino's classification has been widely accepted by dermatologists to classify NO. It was coined by Tanino in 1939, who observed several patients with NO and divided these cases into types by the extent of skin involvement
7. Until now, many studies concerning NO were performed and discussed using Tanino's classificaition
289. However, several studies have demonstrated that Tanino's classification leaves a considerable portion of patients unexplained
1011. Variants unclassified by conventional classification have been reported and therefore have revealed the weaknesses of the original version of Tanino's classifications. Several new classifications have been suggested, but have not drawn much attention yet
1112. In this context, we attempted to present an overview of our experience concerning laser modalities for the treatment of NO, clinical outcomes, and factors affecting the results. In addition, we analyzed the current classification systems in a literature review.
Go to :

MATERIALS AND METHODS
Patients
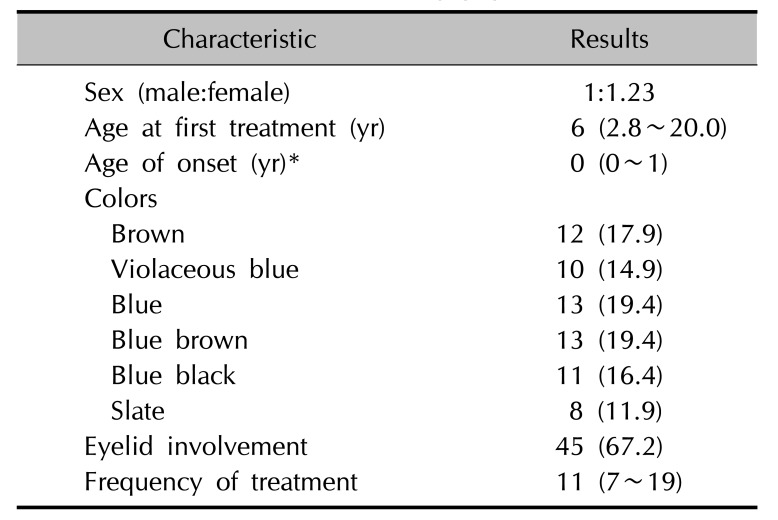
From 2009 to 2015, 67 patients were retrospectively identified who had visited Kangbuk Samsung Hospital, Seoul, South Korea for the treatment of NO. The study also included the participants who were involved in the authors' previous reports
613. Compared to our previous studies, which chose patients treated with a single laser modality only, patients treated with multiple different laser modalities were included since the aim of our present research was to extend our knowledge of what types of lasers are used in a real practice and to investigate the difference in prognosis between laser systems. The study protocol was approved by the institutional review board of Kangbuk Samsung Hospital (KBSMC IRB 2015-08-023).
Study design
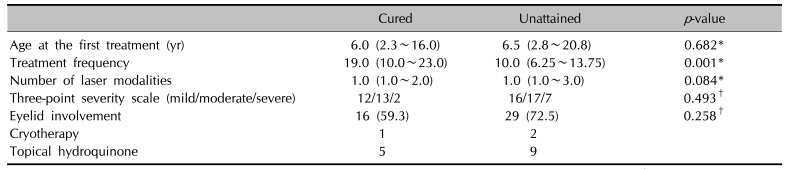
A retrospective review was conducted by two dermatologists, who were not informed of the clinical details regarding the treatment or the patients. Electronic medical charts and photographs taken at each visit were reviewed. The following recorded characteristics were evaluated: sex, age at first treatment, age of onset, color of the NO, involvement of the eyelid and treatment modalities other than laser therapy. Also, laser treatment related factors included in the assessment were the number of laser modalities used and the number of treatment sessions. Objective clinical assessments were performed by two dermatologists who evaluated the photographs taken at the first visit and last visit and classified as follows: cured or excellent, 95%~100% improvement; good, 75%~94% improvement; fair, 50%~74% improvement; poor, 25%~49% improvement; no change, 0%~24% improvement. Given the patients' satisfaction with the treatment and the physicians' aim to cure a disease in a real practice, greater than 95% improvement was considered to be a reasonable treatment end point.
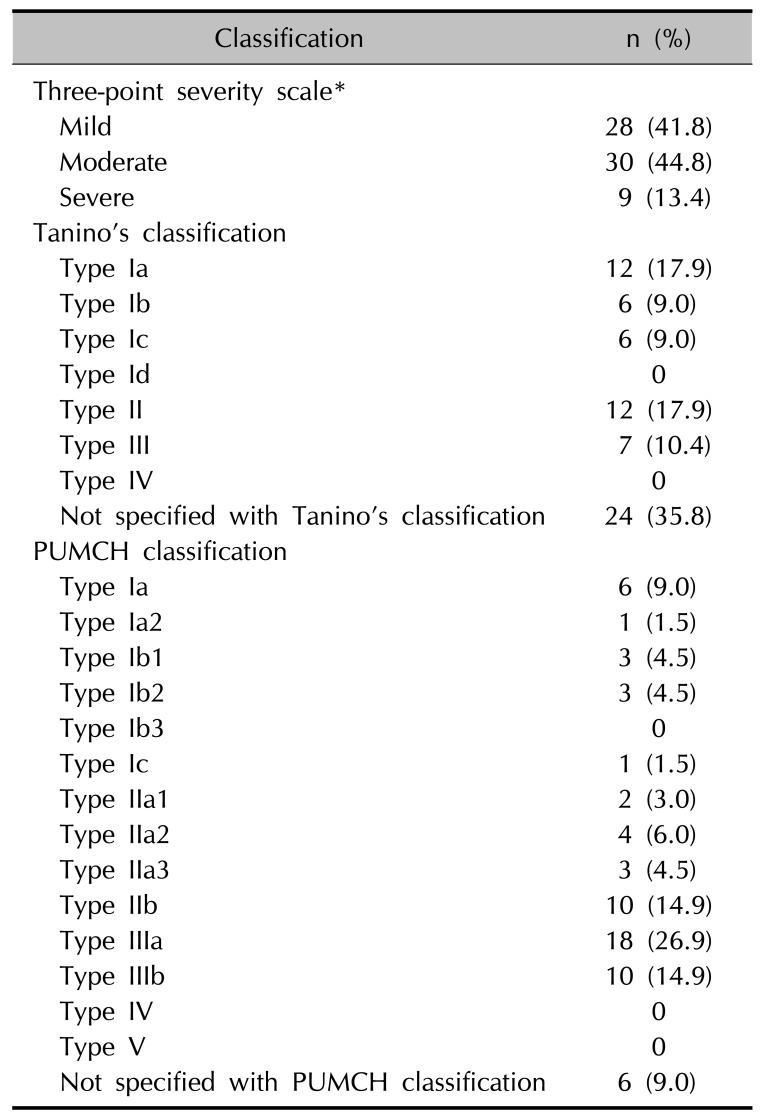
Study participants were sorted by three different classification methods: Tanino's classification, in which NO was divided into 7 types according to the skin involvement area: Type Ia, eyelids, periorbital and temporal area; Type Ib, zygomatic area, nasolabial fold and the lower eyelid; Type Ic, forehead area; Type Id, nostril area; Type II, upper and lower eyelids, zygomatic area, cheek, temple area; Type III, scalp, forehead, eyebrow, and nose; Type IV, bilateral
8, and the Peking Union Medical College Hospital (PUMCH) classification, a new system developed by a Chinese group in 2013, in which NO was distributed into 5 large categories and 15 subdivisions according to the extent of involvement in innervated areas of the trigeminal nerve branches: Type I, pigmentation involving one branch of the trigeminal nerve; Type II, pigmentation involving two branches of the trigeminal nerve; Type III, pigmentation involving all three branches of the trigeminal nerve; Type IV, bilateral type; Type V, NO accompanied by other cutaneous complications
11. For convenience, the authors used a three-point severity scale based on the proportion of the NO on the half face as follows: mild, ≤one third of the half face; moderate, >one third, ≤two thirds and severe, >two thirds.
Specification of laser systems
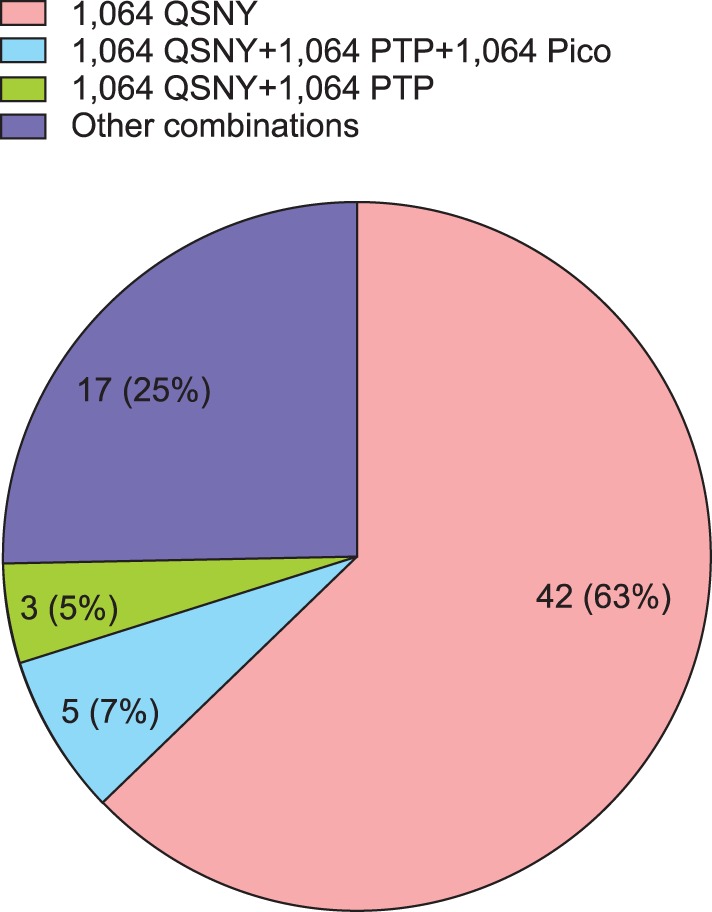
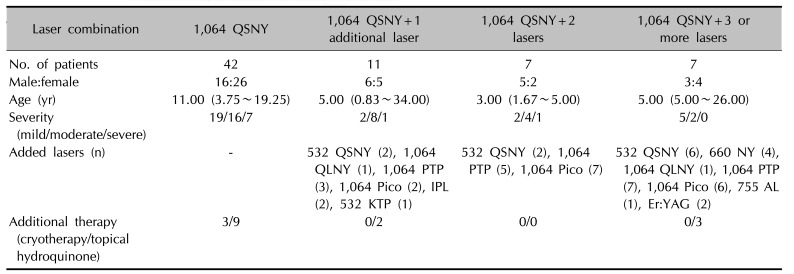
According to the physicians' personal experience, available equipment and preference, several laser modalities were used including QS neodymium-doped yttrium aluminium garnet (Nd:YAG) lasers (Spectra VRMIII™; Spectra XT™; Lutronic Corp., Goyang, Korea or Pastelle™; Won Tech., Daejeon, Korea), dual pulsed Nd:YAG laser (Pastelle™-photoacoustic twin pulse mode; Won Tech.), picosecond-domain Nd:YAG laser (PNY) (Enlighten™; Cutera, Brisbane, CA, USA), 532 nm potassium-titanylphosphate (KTP) and 1,064 nm long-pulsed Nd:YAG laser (Gemini™; Laserscope Corp., San Jose, CA, USA), 755 nm Alexandrite (AL) and 1,064 nm long-pulsed Nd:YAG laser (Clarity™; Lutronic Corp.), 660 nm QS Nd:YAG laser (660NY) (Spectra XT™-Ruvy Touch mode; Lutronic Corp.), quasi-long-pulsed (190 µsec) Nd:YAG laser (QLNY) (Spectra XT™-Spectra mode; Lutronic Corp.), erbium-doped yttrium aluminium garnet (Er:YAG) laser (AVVIO™; Won Tech.), and intense pulsed light (IPL) (RPL™; Ahwon Medi Instrument, Bucheon, Korea).
Three different QS Nd:YAG laser devices were simultaneously used were considered as a single device as they had similar outcomes. Specific modes in the same laser platform were categorized as different laser systems (e.g., photoacoustic twin pulse mode, PTP; Spectra XT™-Spectra mode). PTP mode refers to a dual-pulse method, in which the pulse is divided into two half-fluence pulses with a 140-µs interval
14. With the exception of the laser systems mentioned above, lasers or chemical substances used in irrelevant areas or side effects following laser treatment were excluded.
Statistical analysis
Statistical analyses were conducted with IBM SPSS Statistics ver. 19.0 for Windows (IBM Co., Armonk, NY, USA). Categorical variables were presented as percentages and compared by using the χ2 and Fisher's exact tests. Mann-Whitney U-test was applied to compare two groups with continuous data in a non-normal distribution. A p-value <0.05 was set as the point of significance.
Go to :

Discussion
A NO is composed of melanocytes distributed between the collagen fibers in the dermis
17. Relatively little is known about the underlying mechanism of the treatment of NO with lasers. Theoretically, extremely short bursts emitted by QS lasers are absorbed by melanosomes at a sufficient energy to break down tissue with the lowest collateral thermal damage, referred to as selective photothermolysis
5. Our study validates the usefulness of QS lasers as a single effective treatment modality for NO as the results reveal a significant improvement in patients treated with a 1,064 QSNY laser. In addition, laser treatments may not only stimulate laser-induced pigmentary destruction, but also, dermal regeneration of collagen fibers. Thus dermal fibrosis as well as the disappearance of pigmentation following laser irradiation might deter the residual pigment particles from being noticable
18. In our study, long pulsed and quasi-long-pulsed laser systems were included as a treatment modality. Despite the small number of cases and inconsistent schedules, we expected that long pulsed lasers would work by stimulating collagen remodeling through combined mechanical and thermal effects
19. The IPL with a 560 nm filter also performed based on the suggested mechanism, in which diffuse epidermal necrosis occurs through energy distribution
20. The latest 1,064 nm picosecond laser was used with expectations that the shortest pulse duration may facilitate the removal of pigmentation without lateral heat damage. The novel QS 660 nm Nd:YAG laser was thought to function similar to a conventional QS ruby laser. Lastly, an Er:YAG laser was used for only two patients as they seemed to have superficial skin changes over the NO. Notably, 18 patients (26.8%) exhibited a bumpy skin surface to varying degrees. In this regard, it is recommended that improving pigmentation as well as skin roughness should be taken into consideration in the treatment of NO. Unlike other researchers, our study included all the patients treated with multiple laser modalities, which demonstrated the possibilities of various combinations with QS lasers.
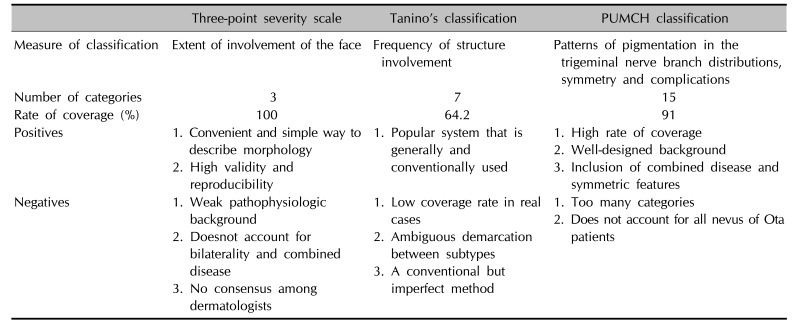
Since 1939, Tanino's classification has been used to describe NO
7. Basically, the classification is based on the severity of the disease according to arbitrarily divided areas of the face. The flaws of Tanino's method included ambiguity of the body parts, low coverage rate and acceptance without consensus. A few authors have attempted to define a new standard
12. Huang et al.
11 recently discovered that 19.74% of patients with a NO were not sorted with Tanino's classification, which is less than 35.8% in our study. The study added the innervated area of the trigeminal nerve to the existing classification. It also took into account the symmetry of pigmentation and NO related complications, such as hemangiomas and vitiligo
11. Although all 1,139 patients in the study were able to be organized with the new classification, referred to as the PUMCH classification, six patients (9.0%) were still not able to be classified with the PUMCH classification. In addition, 15 subtypes may seem excessive and, therefore, another drawback. Tanino's and PUMCH classification systems are also not correlated with clinical outcomes, as the severity scale is. At this point, there is no ideal classification system (
Table 5).
Table 5
Comparison of the nevus of Ota classification methodology
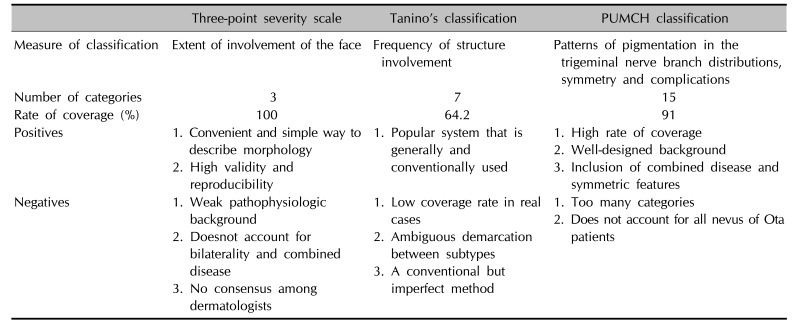
|
Three-point severity scale |
Tanino's classification |
PUMCH classification |
|
Measure of classification |
Extent of involvement of the face |
Frequency of structure involvement |
Patterns of pigmentation in the trigeminal nerve branch distributions, symmetry and complications |
|
Number of categories |
3 |
7 |
15 |
|
Rate of coverage (%) |
100 |
64.2 |
91 |
|
Positives |
1. Convenient and simple way to describe morphology
2. High validity and reproducibility |
1. Popular system that is generally and conventionally used |
1. High rate of coverage
2. Well-designed background
3. Inclusion of combined disease and symmetric features |
|
Negatives |
1. Weak pathophysiologic background
2. Doesnot account for bilaterality and combined disease
3. No consensus among dermatologists |
1. Low coverage rate in real cases
2. Ambiguous demarcation between subtypes
3. A conventional but imperfect method |
1. Too many categories
2. Does not account for all nevus of Ota patients |

The possible factors that influence the results of the study were identified in the current literature: eyelid lesions, Tanino's classification, number of treatment sessions, a bilateral nevus, skin phototype, color of the lesion, and age at the first treatment
261618. Our results revealed that the frequency of treatments was the key factor, which confirmed that more treatments would result in better outcomes, which is in agreement with other studies
216. On the other hand, no significant correlation was revealed between the presence of an eyelid lesion and the severity or classification and clinical outcomes. These results can be corroborated by Zong and Lin's finding
9, in which Tanino's classification had no relationship with the cure rate, although Wang et al.
2 found that eyelid lesions and Tanino's classification were correlated with clinical outcomes.
In addition, the present analysis did not show any significant difference between age at the first treatment and clinical results, which is not consistent with the results of our previous study
6. It was speculated that various laser combinations without homogeneity may affect the results and attenuate significance. Also, our treatment standard was set high at 95% or above improvement, to meet the patients' and clinicians' satisfaction in a real practice
26. For better cosmetic outcomes, various lasers were selected, but this did not lead to significant differences in outcomes in this study. Even with this slight non-alignment, the results revealed that NO is curable with consistent and repetitive laser treatment.
In most studies, transient pigmentary changes were identified, ranging from 8% to 25.1%, which were consistent with that of 15.0% in our study. Only two (3.0%) patients experienced atrophic scarring, which showed gradual improvements with time.
This project was limited in that it was a retrospective and uncontrolled study, including irregular and unequal treatment intervals as well as variable parameters. Second, the recurrence rate was not able to be analyzed because long term follow-up was not feasible. Third, a small sample size may result in a lack of association with the classifications and outcomes. Lastly, skin biopsies were not performed in most of NO patients; thus, we couldn't evaluate the histopathogical aspects of NO.
Since the aforementioned shortcomings existed in this study, a long-term, controlled prospective study with a large study population is required to determine a new classification system that reflects the pathogenesis and clinical prognosis of NO and to determine the best treatment methods for NO.
Our study confirmed that a 1,064 nm QSNY is an effective modality in the treatment of NO, which can function as a single infallible as well as a combination treatment modality. Various treatment sessions are crucial in order to achieve successful and satisfactory results. Existing clinical classifications are not well suited for real-world application. A new clinical classification system should be developed.
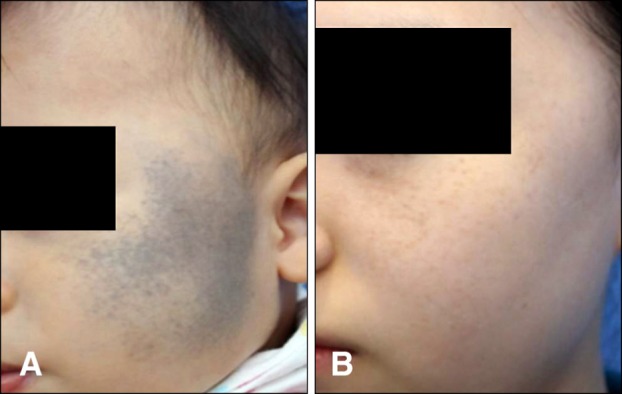
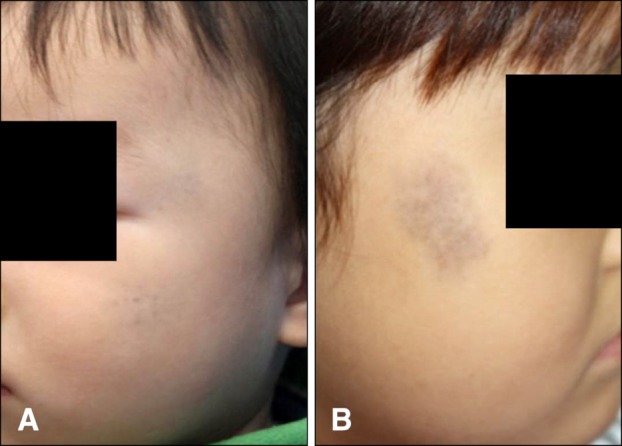
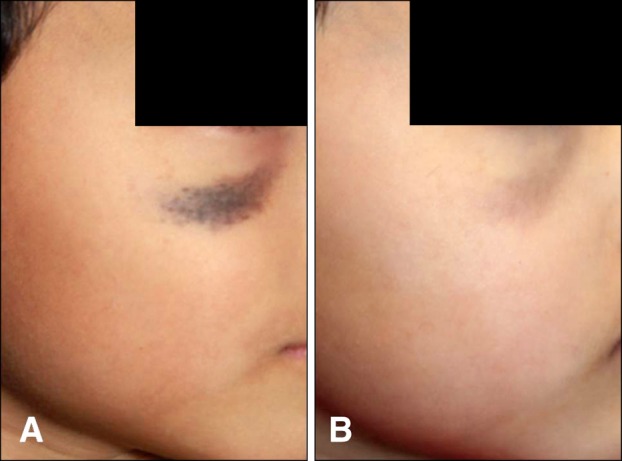
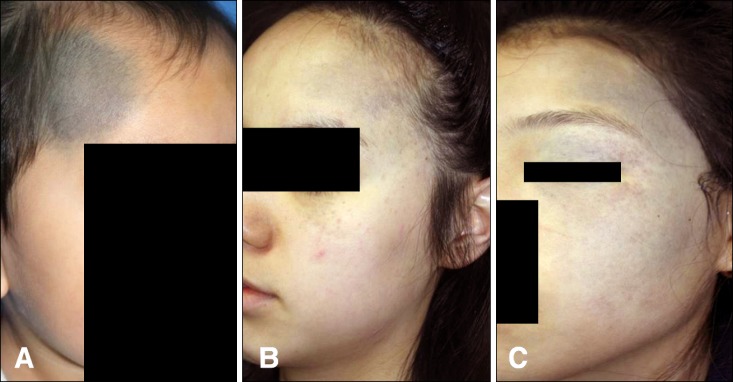
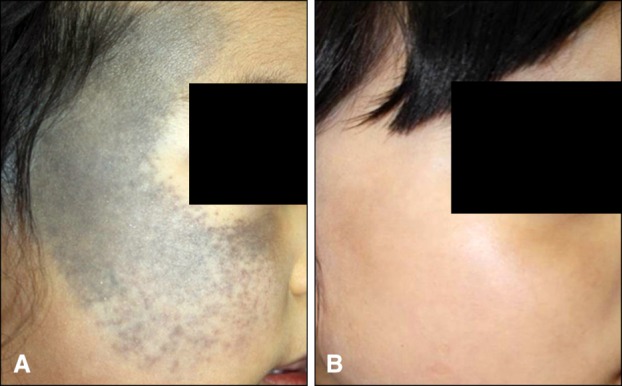
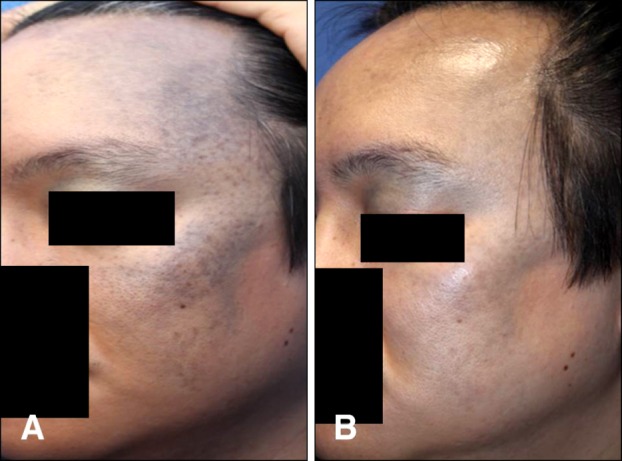
Fig. 6. A 3-year-old female patient classified as “moderate” (A) before treatment, and (B) at the final visit after 30 treatments (excellent outcome).
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download