Abstract
Background
The incidence and mortality rates associated with cutaneous melanoma (CM) have steadily increased over the last 20 years. Even with successful treatment, melanoma patients usually experience substantial anxiety regarding the development of terrible recurrence. To date, few studies have investigated various dermatoses what the patients with CM had anxiety for the recurrence during postoperative surveillance (Dw).
Objective
To describe various Dw and to evaluate the risk of subsequent malignant skin disease in patients with CM.
Results
Fifty-six patients presented with a total of 68 Dw. Among them, melanocytic nevus was the most common (n=27), followed by seborrheic keratosis (n=9) and CM recurrence (n=7). Approximately 5.6% of the lesions were diagnosed as malignant skin diseases. This was a single-center study, so the prevalence of malignant skin diseases following primary melanoma may not represent that of all patients with CM.
Conclusion
The results of this study can be referred by dermatologists dealing with melanoma especially when CM patients have too excessive or unrealistic anxiety for melanoma recurrence during postoperative surveillance of CM. However, the importance of postoperative surveillance must still be emphasized because of real risk of melanoma recurrence and other malignant skin.
A significant increase in the incidence of cutaneous melanoma (CM) has been observed worldwide. According to the latest information from the Korean Statistical Information Service, in 2012, an estimated 521 new cases of melanoma were diagnosed in Korea, and in 2014, there were 291 deaths resulting from melanoma12. Although the absolute mortality rate associated with CM has increased over the last 15 years, there has been a gradual increase in the number of patients living with CM; this is mainly due to earlier detection and increased melanoma awareness34. Therefore, the importance of long-term melanoma surveillance has been recently emphasized5.
Current National Comprehensive Cancer Center Network guidelines call for follow-up intervals generally ranging from every 3~6 months for 1~3 years after diagnosis and annually thereafter, depending primarily on the stage of the disease6. The objectives of follow-up are to provide reassurance and other psychosocial support, as well as the early detection of recurrence and new disease7. Although the vast majority of cases detected at an early stage are treated effectively, most survivors of malignant melanoma have to grapple with the ongoing threat of recurrence and the enduring fear of developing a new melanoma. Therefore, patients visit the clinic to seek medical advice whenever they notice any suspicious skin changes during postoperative surveillance.
Many studies have reported on the risk of recurrence in melanoma and second primary malignancies following primary CM. However, to date, there have been no studies investigating various dermatoses what the patients with CM had anxiety for the recurrence during postoperative surveillance (Dw).
We performed a prospective study between August 2002 and August 2015. This study included 160 patients who attended routine follow-up appointments after surgery for CM at the Department of Dermatology of Pusan National University Hospital. The patients visited the hospital every 3~6 months for 1 year after excision of the primary melanoma, and then annually, in accordance with national melanoma center guidelines. The mean follow-up time was 11.8 months (range, 3~144 months). Of the 160 patients, 56 patients presented with Dw. The final Dw diagnoses were based on the combined clinical, dermoscopic, and histopathologic results.
For the Dw, we analyzed diagnoses, onset, the proportion and types of melanoma recurrence through clinical chart reviews, clinical and dermoscopic photos, and histopathologic findings. The study protocol was approved by the institutional review board at the Pusan National University Hospital, Busan, Korea (IRB no. E-2016006).
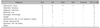
Fifty-six patients presented with a total of 68 cases of Dw. Among them, melanocytic nevus was most common (n=27), followed by seborrheic keratosis (n=9), CM recurrence (n=7), epidermal cyst (n=6), subungual hemorrhage (n=5), lentigo (n=4), melanonychia due to nail appatus lentigo (n=3), fungal melanonychia (n=2), squamous cell carcinoma (n=2), and others (n=3) (Table 1).
The length of time to Dw onset after excision of the primary melanoma varied: 20 lesions occurred 0~3 months after surgery, 15 lesions after 3~6 months, 12 lesions after 6~12 months, 10 lesions after 12~24 months, 6 lesions after 24~60 months, and 5 lesions after 60 months (Fig. 1).
Acral lentiginous melanomas (ALM) was the most common subtype (32 of 56, 57.1%), followed by nodular melanomas (NM, 16 of 56; 28.6%), lentigo maligna melanomas (4 of 56; 7.1%), superficial spreading melanomas (SSM, 2 of 56; 3.6%), and mucoal melanomas (2 of 56; 3.6%). Melanocytic nevus accounted for the largest proportion in all the subtypes, but some difference was found in kinds of dermatoses like subungual hemorrhage, melanonychia and onychomycosis only in ALM. Furthermore, most CM recurrence was observed in NM group (Table 2).
In 3 patients, local recurrence developed within 2 cm of the surgical scar from the primary melanoma excision. Two patients presented with in-transit metastasis, which developed within the lymphatic vessels more than 2 cm from the site of the primary melanoma. One patient with primary melanoma on the chin had multiple distant metastases including skin, liver, and bone metastases. A second primary melanoma occurred in 1 patient.
Most patients diagnosed with cutaneous malignant melanoma undergo routine follow-up after treatment. The main purpose of this follow-up is the surveillance through the early detection of recurrent disease and new primary tumors. Furthermore, follow-up consultations are intended to educate the patient and to reduce the risk of developing future tumors8. Despite the periodical follow-up, both patients and dermatologists can experience substantial anxiety and fear regarding melanoma recurrence whenever any new skin lesions occur. However, no study has investigated the dermatoses that CM patients develop anxiety over during postoperative surveillance. Additionally, the current data on melanoma recurrence during postsurgical surveillance in an Asians is insufficient.
We found various kinds of Dw in our study. The majority (86.8%, 59/68) were benign and, of these, melanocytic nevus accounted for the highest proportion in total (n=27) and in all the subtypes of CM. According to subtypes of CM, there were some difference in the kinds of dermatoses like subungual hemorrhage, melanonychia and onychomycosis only in ALM. A number of previous studies have reported on the association between melanocytic nevus and melanoma91011. Clinicians engaged in the surveillance of nevi for early detection of CM are often confronted with the question of how likely it is that any given nevus will turn into a CM. Tsao et al.12 reported that the annual transformation rate of any single nevus into melanoma ranges from 0.0005% to 0.003% in the general population. This study also reported that, for a 20-year-old individual, the lifetime risk of any selected mole transforming into melanoma by age 80 is approximately 0.03% for men and 0.009% for women. In contrast, individuals with risk factors, such as a previous melanoma or dysplastic nevi, have a high relative risk of developing CM compared with general population. Though this kind of data is lacking in Asians, the incidence of melanoma transformation in Asians could be much lower than that of Caucasians. Anyway, the importance of routine follow-up after surgery for both physicians and patients must be important. Patients must be encouraged to participate in CM surveillance and to practice regular skin self-examination. However, based on our results, patients should not be excessively worried because most lesions suspicious for melanoma by themselves in our study were benign skin diseases. In addition, we believe that the data on various Dw provided in this study may be of use to physicians who deal with melanoma.
Nine of the 68 lesions were diagnosed as malignant skin diseases. These included 7 recurrent or second primary melanomas and 2 squamous cell carcinomas. A total of 7 subsequent CMs comprised 5 local recurrences (including satellite metastases and in-transit melanoma metastases), 1 distant metastasis, and 1 second primary melanoma. The incidence of local recurrence was 3.1%; this was consistent with previous studies that reported a local recurrence rate of approximately 3%~5%131415. The prevalence of a second primary melanoma following a primary CM was 0.6%; this was similar than the prevalence of 0.5%~5.5% reported by previous studies16171819. We also observed a lower prevalence (1.3%) of nonmelanoma skin cancer (NMSC) compared with a previous study (10.7%)20.
Most of these previous studies have focused on Caucasian populations. Skin cancers such as CM and NMSC are relatively rare occurrences in the Asians compared with fair-skinned populations. Factors contributing to these incidence rates include solar UV exposure differences, Fitzpatrick skin type, and inherent genetic variabilities21. Although there has been no previous report on the incidence rate of second primary malignancies in the Asians, we believe that racial differences influenced the low prevalence of second primary malignancies in this study. We propose that the results of our study could be used as basic clinical data for further melanoma studies in Asians.
Most Dw were found within 6 months of follow-up. This early detection could be due to the substantial anxiety and fear associated with melanoma recurrence. According to previous reports on anxiety after cancer diagnosis22, patients experienced high levels of anxiety immediately after cessation of treatment, and this anxiety decreased with time. Thus, within the 6 months following the first surgery, patients tended to observe any skin changes more closely and visit a dermatologist more rapidly when a suspicious lesion was found. Interestingly, 1 patient even visited a dermatologist over 20 times, but these visits were for routine follow-up appointments during postoperative surveillance to check for recurrence of the melanoma.
In summary, most lesions identified by patients themselves as suspicious for melanoma were benign skin diseases, and approximately 5.6% of the lesions were diagnosed as malignant skin diseases. Therefore, if CM patients have too much or unreal anxiety for melanoma recurrence during postoperative surveillance, dermatologists treating melanoma can refer to this result. However, the importance of postoperative surveillance remains to be emphasized, as recurrent melanoma or other malignant skin diseases accounted for about 5.6% of lesions. This study seems to be unique because, to date, there has been no report on various dermatoses that cause anxiety in CM patients during postoperative surveillance.
In addition, the results of this study could inform future melanoma studies in Asians.
There were a few limitations in the present study. First, this was a single-center study, so the prevalence of malignant skin diseases following primary melanoma may not represent that of all patients with CM. Second, subjects in this study were limited to those with Dw, and so some Dw like melanocytic nevi could be exist before surgery. Third, the the follow-up period was not enough in some patients. As all skin lesions that developed during postoperative surveillance were not included in this study, statistical analysis of the prevalence of each diagnosis was limited.
Figures and Tables
Fig. 1
Onsets of dermatoses what the patients with cutaneous melanoma (CM) had anxiety for the recurrence during postoperative surveillance. Dw: dermatoses what the patients with CM had anxiety for the recurrence during postoperative surveillance.

Table 1
Dermatoses what the patients with cutaneous melanoma had anxiety for the recurrence during postoperative surveillance

Table 2
Analysis of dermatoses according to melanoma subtype
References
1. Ministry of Health and Welfare. Cancer incident cases, incidence rates and relative survival rate. Statistics Korea [Internet]. Daejeon: Statistics Korea;2012. Available from: http://kosis.kr.
2. Korean Statistical Information Service. Cause of death statistics. Statistics Korea [Internet]. Daejeon: Statistics Korea;2014. Available from: http://kosis.kr.
3. Stang A, Stang K, Stegmaier C, Hakulinen T, Jöckel KH. Skin melanoma in Saarland: incidence, survival and mortality 1970-1996. Eur J Cancer Prev. 2001; 10:407–415.

4. Garbe C, McLeod GR, Buettner PG. Time trends of cutaneous melanoma in Queensland, Australia and Central Europe. Cancer. 2000; 89:1269–1278.

5. van der Velden HM, van Rossum MM, Blokx WA, Boezeman JB, Gerritsen MJ. Clinical characteristics of cutaneous melanoma and second primary malignancies in a dutch hospital-based cohort of cutaneous melanoma patients. Dermatol Res Pract. 2009; 2009:479183.

6. Coit DG, Andtbacka R, Bichakjian CK, Dilawari RA, Dimaio D, Guild V, et al. Melanoma. J Natl Compr Canc Netw. 2009; 7:250–275.

7. Dancey A, Rayatt S, Courthold J, Roberts J. Views of UK melanoma patients on routine follow-up care. Br J Plast Surg. 2005; 58:245–250.

8. Themstrup L, Jemec GE, Lock-Andersen J. Patients highly value routine follow-up of skin cancer and cutaneous melanoma. Dan Med J. 2013; 60:A4713.
9. Holly EA, Kelly JW, Shpall SN, Chiu SH. Number of melanocytic nevi as a major risk factor for malignant melanoma. J Am Acad Dermatol. 1987; 17:459–468.

10. Garbe C, Büttner P, Weiss J, Soyer HP, Stocker U, Krüger S, et al. Risk factors for developing cutaneous melanoma and criteria for identifying persons at risk: multicenter case-control study of the Central Malignant Melanoma Registry of the German Dermatological Society. J Invest Dermatol. 1994; 102:695–699.

11. Tucker MA, Halpern A, Holly EA, Hartge P, Elder DE, Sagebiel RW, et al. Clinically recognized dysplastic nevi. A central risk factor for cutaneous melanoma. JAMA. 1997; 277:1439–1444.

12. Tsao H, Bevona C, Goggins W, Quinn T. The transformation rate of moles (melanocytic nevi) into cutaneous melanoma: a population-based estimate. Arch Dermatol. 2003; 139:282–288.

13. Cruse CW, Wells KE, Schroer KR, Reintgen DS. Etiology and prognosis of local recurrence in malignant melanoma of the skin. Ann Plast Surg. 1992; 28:26–28.

14. Urist MM, Balch CM, Soong S, Shaw HM, Milton GW, Maddox WA. The influence of surgical margins and prognostic factors predicting the risk of local recurrence in 3445 patients with primary cutaneous melanoma. Cancer. 1985; 55:1398–1402.

15. Cohn-Cedermark G, Månsson-Brahme E, Rutqvist LE, Larsson O, Singnomklao T, Ringborg U. Outcomes of patients with local recurrence of cutaneous malignant melanoma: a population-based study. Cancer. 1997; 80:1418–1425.

16. Wassberg C, Thörn M, Yuen J, Ringborg U, Hakulinen T. Second primary cancers in patients with cutaneous malignant melanoma: a population-based study in Sweden. Br J Cancer. 1996; 73:255–259.

17. Veronesi U, Cascinelli N, Bufalino R. Evaluation of the risk of multiple primaries in malignant cutaneous melanoma. Tumori. 1976; 62:127–130.

18. Brobeil A, Rapaport D, Wells K, Cruse CW, Glass F, Fenske N, et al. Multiple primary melanomas: implications for screening and follow-up programs for melanoma. Ann Surg Oncol. 1997; 4:19–23.

19. DiFronzo LA, Wanek LA, Elashoff R, Morton DL. Increased incidence of second primary melanoma in patients with a previous cutaneous melanoma. Ann Surg Oncol. 1999; 6:705–711.

20. Jung GW, Dover DC, Salopek TG. Risk of second primary malignancies following a diagnosis of cutaneous malignant melanoma or nonmelanoma skin cancer in Alberta, Canada from 1979 to 2009. Br J Dermatol. 2014; 170:136–143.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download