INTRODUCTION
Senile lentigo is a benign and common discoloration in older people. Clinically, senile lentigo demonstrates a well-defined, annular or ovoid, uniform tan to brown, small macule or patch, which presents on sun-exposed skin, such as the face, dorsal hands, and extensor forearms. Aged skin in Asians is characterized by striking pigmentary changes rather than the wrinkles apparent in Caucasian skin with aging
1. Exposure to sunlight has been suggested to be the major cause of various pigmentary disorders in aged skin. For the development of senile lentigines, chronic sun exposure is necessary in pathogenesis. Prior studies suggested that keratinocytes and melanocytes play a role in the formation of senile lentigo in response to ultraviolet irradiation
2.
Senile lentigines are not harmful to health, but may cause cosmetic problems in elderly individuals with widespread and disfiguring features. Q-switched (QS) lasers, including 532 nm QS Neodymium:Yttrium-Aluminum-Garnet (Nd:YAG), QS ruby and QS alexandrite lasers, have become popular in treating senile lentigo. However, post-inflammatory hyperpigmentation can occur in 10%∼25% of irradiated patients
3.
Use of a low fluence 1,064 nm QS Nd:YAG laser, also termed laser toning, has been introduced to improve a variety of benign pigmentary disorders, including melasma and nevus of Ota
45. Laser toning has become a mainstay in the treatment armamentarium for the management of benign pigmented lesions by achieving successful outcomes and lowering side effects accompanied with conventional QS laser therapy
5.
Although the efficacy of laser toning has been proven through diverse experience with various skin lesions, no studies have addressed the efficacy of laser toning in the treatment of solar lentigo. Here, we describe laser treatment using a low fluence 1,064 nm QS Nd:YAG laser to reduce senile lentigo on the face.
Go to :

MATERIALS AND METHODS
Study participants
A retrospective review was conducted on patients treated at least four times with low fluence 1,064 nm QS Nd:YAG laser for skin brightening between 2009 and 2015. The participants were older than 40 years of age and had moderate to severe grade of multiple senile lentigines on the face. To clarify the extent of disease, other pigmentary lesions, such as melasma, freckle, and obvious seborrheic keratosis, were excluded. In addition, any patients who had undergone previous laser or cosmetic procedures on the face within 3 weeks of the first treatment session were excluded. The study protocols have been approved by the institutional review board (IRB) of Kangbuk Samsung Hospital, Seoul, Korea (KBSMC IRB no. 2016-02-028).
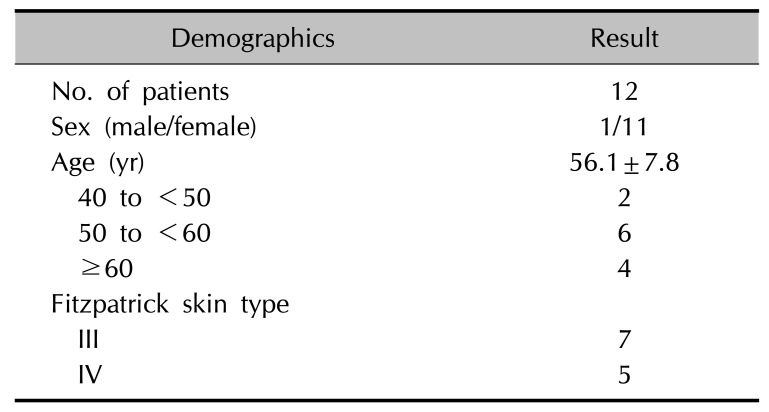
Twelve individuals (one male and 11 females) were included. The mean age at the first visit was 56.1 years (range, 43∼69 years) (
Table 1).
Table 1
Demographics of study participants (n=12)
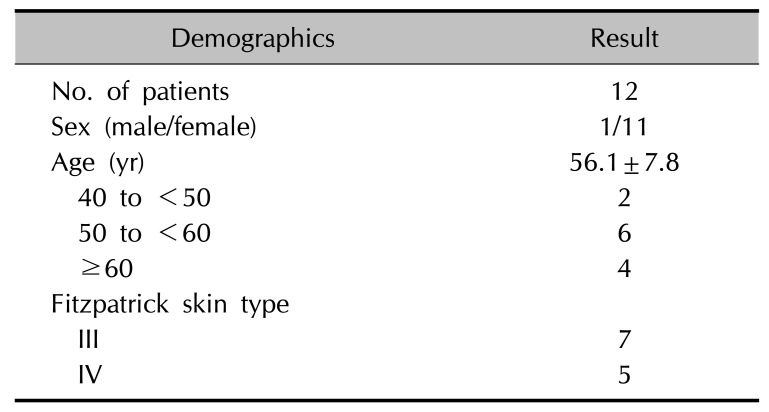
|
Demographics |
Result |
|
No. of patients |
12 |
|
Sex (male/female) |
1/11 |
|
Age (yr) |
56.1±7.8 |
|
40 to <50 |
2 |
|
50 to <60 |
6 |
|
≥60 |
4 |
|
Fitzpatrick skin type |
|
|
III |
7 |
|
IV |
5 |

Laser treatment
All 12 patients were treated in 5 to 12 sessions with low-fluence QS Nd:YAG laser (Spectra VRMIII®; Lutronic Corp., Seoul, Korea) at a wavelength of 1,064 nm, pulse duration of 5∼10 nsec, spot size of 8 mm, and fluence of 0.8∼2.0 J/cm2. The entire face was covered as a treatment field, since general facial brightening was the goal throughout the treatment period. The laser fluence was adjusted based on patients' response to the previous treatment. No topical anesthesia and pre-procedure processes were used. The treatment endpoint was immediate moderate erythema.
Clinical assessment
Clinical response after laser treatment was independently scored by two dermatologists with clinical photographs taken at each visit. A quartile scale was used: minimal improvement (<25% response), moderate improvement (26%∼50% improvement), marked improvement (51%∼75% improvement), and near total improvement (>75% response). Physicians' scores were confirmed only if the ratings of the two dermatologists were consistent. All cutaneous adverse events were recorded to assess the safety of the laser modality; these included hyperpigmentation, hypopigmentation, persistent erythema, crust, and burning and itching sensation.
Statistical analysis
To compare treatment-related factors between two groups classified with clinical response rate, a Mann-Whitney test was performed on the number of treatment session, mean treatment fluence, and mean treatment interval. All analyses were conducted using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA). Statistical significance was defined as p<0.05.
Go to :

RESULTS
The demographics of the study participants are presented in
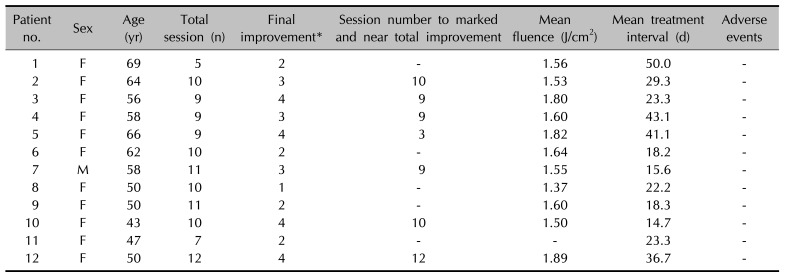
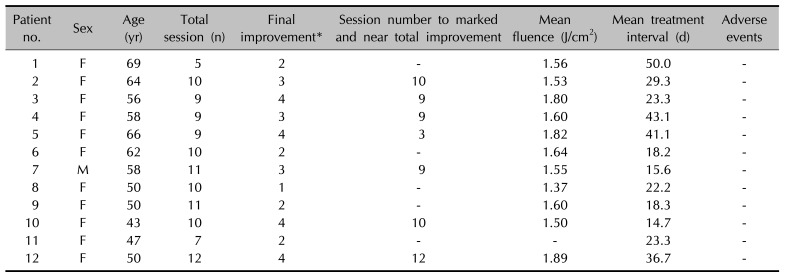
Table 1. The male-to-female ratio was 1:11. The individual clinical data are summarized in
Table 2. The mean number of treatment sessions was 8.8±2.6, the mean interval between sessions was 28.0±11.4 days, and the mean treatment fluence was 1.62±0.16 J/cm
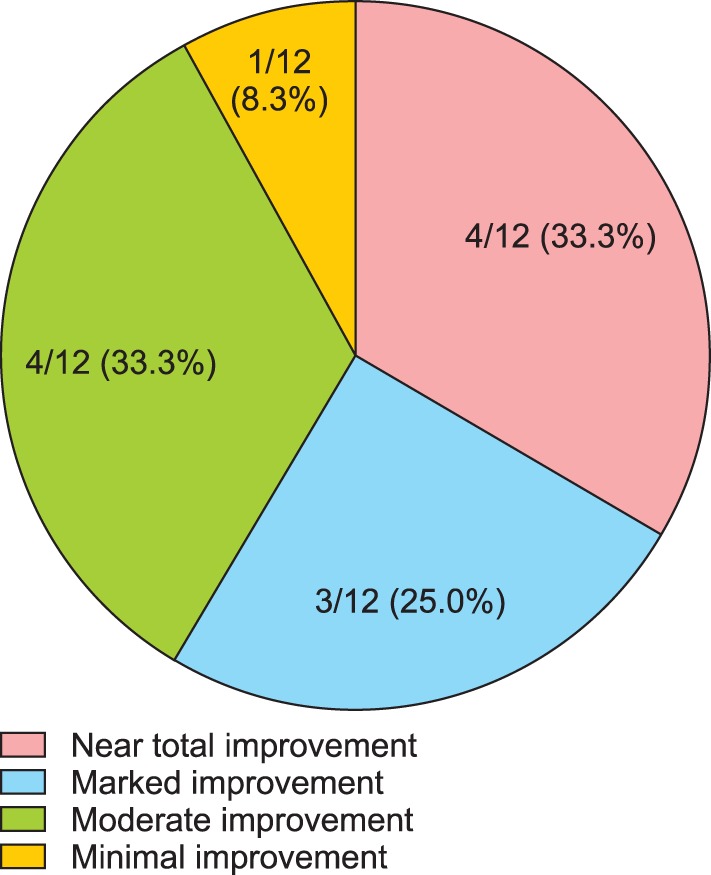
2. The mean number of treatment sessions required to reach marked and near-total improvement was 8.7±2.8. At the final visit, all patients showed an improved response compared to pre-treatment status. Seven of 12 (58.3%) patients achieved marked and near-total improvement, and three of 12 (25.0%) patients achieved moderate improvement (
Fig. 1).
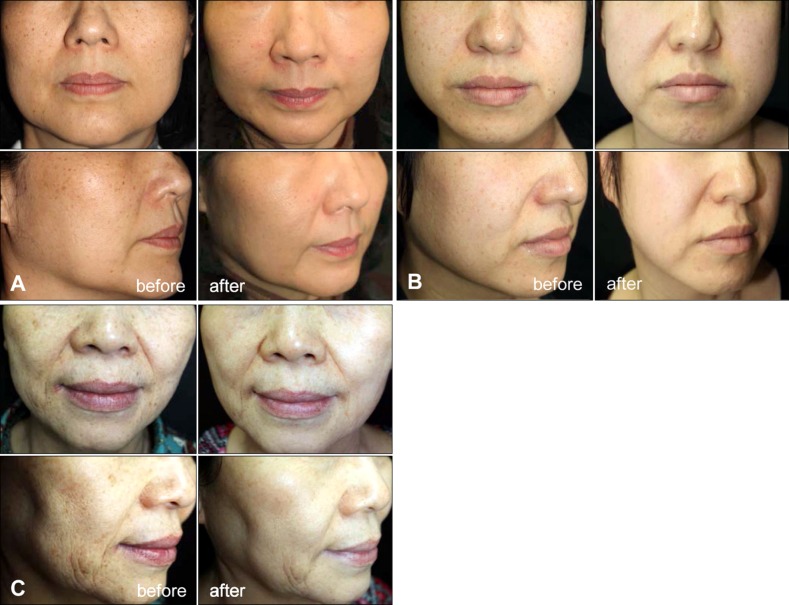
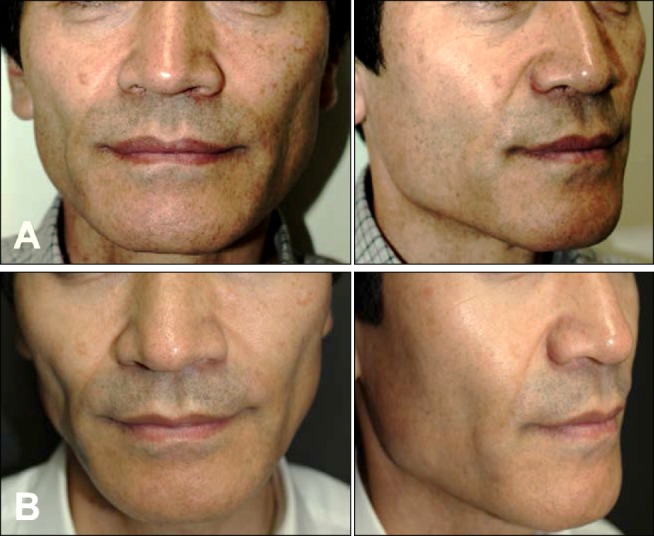
Fig. 2 and
3 present representative cases of near-total improvement and marked improvement respectively. Side effects were not noticeable during all laser sessions (
Table 2).
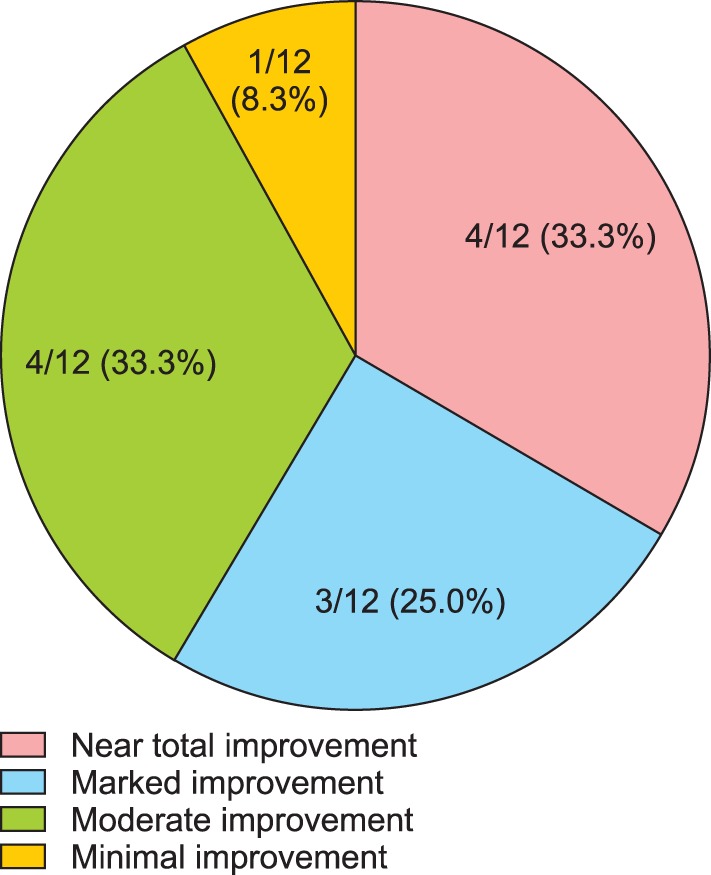 | Fig. 1Clinical improvement at the final visit (n=12).
|
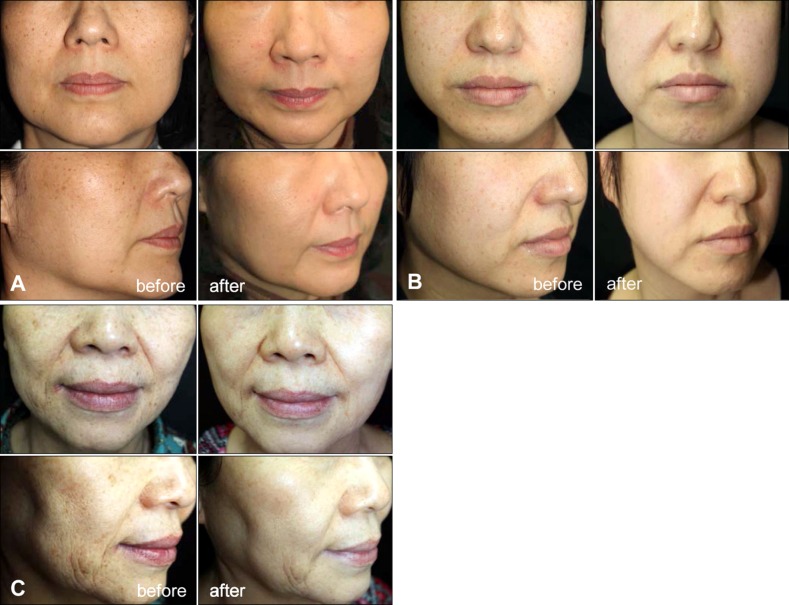 | Fig. 2Clinical images of near total improvement cases. (A) No. 3 patient before treatment (left) and at 7-month visit after 9 sessions of Neodymium:Yttrium-Aluminum-Garnet laser treatment (right), (B) No. 10 patient before treatment (left) and at 5-month visit after 10 sessions of laser treatment (right), and (C) No. 12 patient before treatment (left) and at 14-month visit after 12 sessions of laser treatment (right).
|
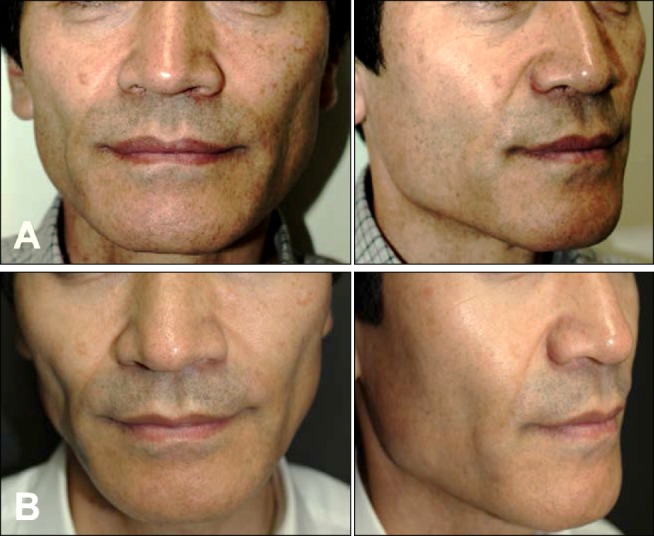 | Fig. 3Clinical image of marked improvement case (No. 7 patient) (A) before treatment and (B) at 5-month visit after 9 sessions of Neodymium:Yttrium-Aluminum-Garnet laser treatment on the face.
|
Table 2
Overall results of patients with low fluence 1,064 nm Q-switched Neodymium:Yttrium-Aluminum-Garnet laser treatment (n=12)
|
Patient no. |
Sex |
Age (yr) |
Total session (n) |
Final improvement*
|
Session number to marked and near total improvement |
Mean fluence (J/cm2) |
Mean treatment interval (d) |
Adverse events |
|
1 |
F |
69 |
5 |
2 |
- |
1.56 |
50.0 |
- |
|
2 |
F |
64 |
10 |
3 |
10 |
1.53 |
29.3 |
- |
|
3 |
F |
56 |
9 |
4 |
9 |
1.80 |
23.3 |
- |
|
4 |
F |
58 |
9 |
3 |
9 |
1.60 |
43.1 |
- |
|
5 |
F |
66 |
9 |
4 |
3 |
1.82 |
41.1 |
- |
|
6 |
F |
62 |
10 |
2 |
- |
1.64 |
18.2 |
- |
|
7 |
M |
58 |
11 |
3 |
9 |
1.55 |
15.6 |
- |
|
8 |
F |
50 |
10 |
1 |
- |
1.37 |
22.2 |
- |
|
9 |
F |
50 |
11 |
2 |
- |
1.60 |
18.3 |
- |
|
10 |
F |
43 |
10 |
4 |
10 |
1.50 |
14.7 |
- |
|
11 |
F |
47 |
7 |
2 |
- |
- |
23.3 |
- |
|
12 |
F |
50 |
12 |
4 |
12 |
1.89 |
36.7 |
- |

To identify the factors significantly associated with the clinical response rate of senile lentigo to treatment with a 1,064 nm QS Nd:YAG laser, we classified patients into the good-response group, which showed near-total and marked improvement (n=7), and the remaining patients into the poor-response group (n=5). However, no difference between the groups was evident for mean number of treatment sessions (8.86 in the good-response group vs. 8.60 in the poor-response group, p>0.93), mean treatment treatment fluence (1.67 J/cm2 vs. 1.54 J/cm2, p>0.51), and mean treatment interval (29.1 days vs. 26.4 days, p> 0.69).
Go to :

DISCUSSION
Senile lentigo can occur with 90% of people older than 60 years of age and is generally regarded as an early sign of aged skin
13. In terms of pathogenesis, keratinocytes secrete prostaglandin and chemical mediators, which lead to an increase in tyrosinase activity in melanocytes following upregulation of the endothelin-1 and endothelin-B pathways
6. In addition, melanocytes fail to facilitate melanosome transfer in the epidermis, which disturbs the interaction between keratinocytes and melanocytes
2. Over the long-term, the epidermis becomes thickened and pigmented, which is associated with an increased number of melanocytes as well as an increased amount of melanin
7.
Senile lentigo usually presents as an evenly pigmented and well-demarcated discoloration. Multiple spots, rather than a single spot, are characteristic. Melanoma, on the contrary, appears as irregular shaped, variegated dark macule or patch. The melanoma surface exhibits bleeding and ulceration, which may imply malignancy
8. In addition to apprehension with malignant skin tumor, common cosmetic concerns with benign pigmented lesion include melasma, seborrheic keratosis, lentigines, freckles and acquired bilateral nevus-of-Ota-like macules (ABNOM). While melasma and freckles occur at a relatively young age, senile lentigo is mostly observed in older individuals. Seborrheic keratosis often demonstrates brown macules similar to senile lentigo, although it has more verrucous surface and a darker hue than the latter
1. Bilateral, confluent, brown to slate-gray dermal pigmentation favors ABNOM over senile lentigo
9. Our study only included the lesions with distinct features of multiple, uniformly colored, and wrinkled around lesions to exclude misclassification. Given that age can help differentiate senile lentigo from other benign pigmented lesions, our participants all were older than 40 years of age.
Various laser systems have been used for the treatment of senile lentigo. QS lasers, such as 532 nm Nd:YAG lasers, ruby lasers and alexandrite lasers, are recognized as a mainstay in the treatment of senile lentigo. These lasers utilize a nanosecond pulse duration, thus allowing laser energy to be absorbed by melanin and melanosomes, resulting in the destruction of melanocytes on the basis of the selective photothermolysis
10. Unfortunately, the use of QS lasers is associated with post-inflammatory hyperpigmentation; QS laser generated acoustic waves injure pigmented cells and adjacent vessels by inducing a photomechanical effect
1011. Alternatively, long pulsed lasers, such as 595 nm dye lasers, alexandrite lasers and potassium-titanyl-phosphate (KTP) lasers, can also be applied to patients with lentigines. Unlike QS lasers, long pulsed lasers yield significant results based on the photothermal effect only, which contributes to bulk heating and, consequently, diffuse damage in the pigmented epidermis
310. Despite the plethora of laser options, there has been no research on the treatment of senile lentigo using laser toning. The present retrospective study investigated the effect of laser toning in the treatment of senile lentigo in Asian skin.
Significant improvement of senile lentigines with laser toning was shown. A large majority of patients experienced marked improvement or more satisfactory results without permanent injuries, such as scarring or pigmentary changes. Little downtime, which is another advantage of laser toning, has been reported in all cases as in other studies using laser toning
12. The optimized but effective low fluence beam is directed through epidermis into the dermis, while damaging the melanosomes at the subcellular level
1314. A key problem with much of the literature in relation to laser toning on pigmented lesions is that a longer period of treatment with appropriate frequency is required for better clinical results
13, which was also evident in our retrospective analysis. Little is known of the mechanism of lentigo removal. Supposedly, pigmentation may be removed through destruction of melanosomes induced by selective photothermolysis as apparent in Café au lait macule or melasma lesions
131516. Histopathologically, epidermal hyperplasia is present, but is not exceedingly prominent, in lentigo lesions, in agreement with more noticeable dyspigmentation rather than the surface change that is seen clinically
7. Therefore, just pigment improvement induced by laser toning may lead to overall enhancement on the evaluation of the outcome.
With respect to post laser toning hypopigmentation, color changes are likely to be related to cumulative laser sessions and short interval between sessions
17. This supports our finding of no leukoderma following laser toning in the patients treated for an average interval of 28.0 days, which was longer than the standard weekly or fortnightly schedules of treatment.
In this study, marked improvement was achieved after only three sessions, which was far earlier than in other patients. Indeed, in one patient, who received intense pulsed light (IPL) 4 weeks earlier, improvement was rather evident in a relatively brief time. It was postulated that IPL prior to laser toning might exert an additive effect on lentigo reduction when used within a short period of time.
There are three limitations to the study. The first is that a retrospective study was conducted, which hampers any cause-and-effect conclusion. For this reason, additional follow-ups since the last treatment were not able to be undertaken. Therefore, we are not sure whether clinical clearance would be maintained or decreased over time after cessation of treatment. The second is the small sample size. Thirdly, the histopathologic evidence was unclear. Thus, other similar pigmented tumors, such as flat seborrheic keratosis and lentigo maligna, may have been included, particularly in the poor-response group, irrespective of our intention. Lastly, several relevant factors, which may affect clinical outcomes, were not addressed. For instance, skin thickness or texture can be considered in determining which laser systems lead to favorable results. Future work needs to be carried out to establish whether laser toning provides consistent clinical outcomes in a large population-based prospective study.
In conclusion, we herein offer a new approach to the treatment of senile lentigo with laser toning. This technique improved diffuse senile lentigines on the face after multiple sessions, and resulted in acceptable clinical outcomes. Laser toning, which represents a steady but safe and effective methodology, may be an alternative to conventional laser systems, particularly in patients in whom no downtime or post-inflammatory hyperpigmentation is acceptable.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download