Abstract
PURPOSE
The goal of this study was to evaluate the clinical outcome of single short implants, less than 8 mm in length, placed in the posterior area.
MATERIALS AND METHODS
A total of 128 patients (75 male and 53 female, mean age: 52.6±11.2 years) with 154 implants participated. Implant marginal bone loss, and survival and success rates were measured.
RESULTS
The mean follow-up period was 51.35±24.97 months. A total of 128 implants, 8 mm in length, were placed in patients who had mean marginal bone loss of 0.75 mm. These implants had a survival rate of 95.3%. Twenty-six implants, 7 mm in length, were placed in areas with a mean marginal bone loss of 0.78 mm and had a survival rate of 96.2%. Both marginal bone loss and survival rate were not statistically different among the groups. In the maxilla, 34 implants showed a mean marginal bone loss of 0.77 mm and a survival rate of 97.1%. In the mandible, 120 implants showed a mean marginal bone loss of 0.75 mm and a survival rate of 95.0%. The average marginal bone loss around all implants was 0.76±0.27 mm at the last follow-up review after functional loading. The survival rate was 95.6% and success rate was 93.5%.
With the recent development of implant surface treatment and bone graft techniques, implants can be placed in the anterior and posterior areas with high predictability. However, the length of mandibular implants may be limited due to insufficient vertical height from the ridge to the inferior alveolar nerve. This height deficiency results from alveolar bone resorption, commonly seen after long-term tooth loss. As a result, several methods for placing short implants have been proposed. Short implants are advantageous for several reasons: 1) invasive surgical procedures such as ridge augmentation can be avoided in the posterior area; 2) overheating during drilling is minimized; 3) maxillary sinus and inferior alveolar canal invasion is minimized; 4) root damage can be prevented in cases where adjacent teeth have large root curvatures; 5) labial bone perforation can be avoided in the areas where buccal undercut or concavity exists; and 6) surgeons are able to use simple instruments, shorten procedure times, and minimize bone grafting.1
Several studies have reported high failure rates with short implants less than 10 mm in length after load-bearing in the posterior area in partially edentulous patients. However, minimally invasive procedures using short implants may be the only treatment option for patients with unfavorable anatomical conditions such as insufficient alveolar ridge height or a reduced vertical distance to the inferior alveolar nerve. Furthermore, the prognosis of these implants has been significantly improved due to recent improvements in implant designs and surface treatment techniques. Failure rates are higher in the maxilla than in the mandible because the maxilla has a lower bone density and is relatively softer.23456
According to Misch, when two or more implants are placed, they must be connected.7 As such, it is generally accepted as a principle when two or more short implants are placed in the posterior area, they are splinted to distribute the stress among them. Many authors reported that the success rate of splinted short implants has been reported to be higher than that of non-splinted short implants.8910 Antoun evaluated the outcomes of wide-diameter implants immediately provisionalized with cement-retained single crowns in posterior molar sites. They suggested that wide-diameter (6 mm) implants can safely and successfully replace single posterior molars.11 Calandriello and Tomatis reported that the use of immediately loaded single lower molars supported by Branemark System Wide Platform TiUnite implants had favorable results. A total of 40 Brånemark System TiUnite Wide Platform MK III implants were placed. All implants were provided with provisional crowns in full centric occlusion at the time of surgery. Two implants failed so that the cumulative success rate at 5 years was 95.0%. The mean marginal bone remodeling (n = 38) expressed as an average of mesial and distal values was −1.17 mm (SD ± 0.90) at the 5-year time point.12
However, in 2004, Fugazzotto et al.13 reported a mean success rate of 95.1% during a period of 29.3 months for single implants less than 9 mm in length. Malmstrom et al.14 reported similar success rates among short implants 6-mm or 8-mm in length and long implants 11 mm in length and found no clinically significant difference between splinted implants and single crowns. Despite these studies, research on the clinical prognosis of single short implants in the posterior area is rare.
The goal of this study was to evaluate the clinical prognosis of single short implants less than 8 mm in length placed in the maxillary and mandibular posterior areas.
Among patients who underwent implant placement in Seoul National University Bundang Hospital (SNUBH) between January 2006 and December 2014, 128 patients (75 male and 53 female, mean age: 52.6 ± 11.2 years), who received short implants, were selected. The inclusion and exclusion criteria are as follows.
Inclusion criteria
Exclusion criteria
A total of 154 Implantium Superline implants (Dentium, Suwon, Korea) were placed by one surgeon. This study was performed with the permission of SNUBH Institutional Review Board (IRB) (No. B-1501/284-104). Implant length, width, placement area, primary and secondary stability, survival and success rates, and surgical method, additional bone grafting, marginal bone loss and complications were investigated through a careful review of the patients' medical records and radiographs. Implant stability was measured with using an Osstell Mentor device (Osstell, Gothenburg, Sweden) to determine ISQ values. Primary stability was measured at the time of implant placement and the secondary stability was measured at the time of prosthetic impression taking.
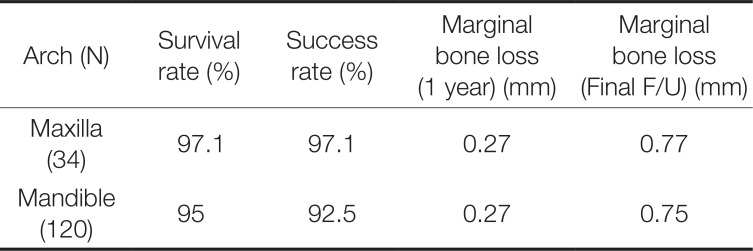
The implants were divided into a 7 mm group and an 8 mm group. There were 26 implants 7 mm-long and 128 implants 8 mm-long. The implants were also classified according to their width (4 mm, 4.5 mm, 5.0 mm, 6 mm, and 7 mm). There were 9 implants 4 mm-wide, 7 implants 4.5 mm-wide, 71 implants 5.0 mm-wide, 57 implants 6 mm-wide, and 10 implants 7 mm-wide. Also, the implants were classified according to the dental arch in which they were placed, and 34 implants were in the maxilla and 120 were in the mandible. When classified according to the placement method, it was found that non-submerged placement was used for 65 implants, and submerged placement was used for 89 implants (Table 1).
Successful implant placement was defined according to Albrektsson's definition proposed in 198615: 1) Individual unattached implant that is immobile when tested clinically; 2) radiography without evidence of peri-implant radiolucency; 3) Bone loss less than 0.2 mm annually after the first post-operative year; 4) No persistent pain, discomfort, or infection; 5) By these criteria, success is defined as success rate of at least 85% at the end of a 5-year observation period and 80% at the end of a 10 year period. The survival rate is the ratio of the number of retained implants from placement to the final examination regardless of loosening, inflammation, and bone loss, to the total number of implants placed.16
To measure the degree of alveolar bone resorption, periapical radiographs obtained immediately after the prosthesis placement were set as the baseline. Marginal bone loss was assessed by comparing periapical radiographs obtained using the paralleling technique 12 months after the functional loading and during the last visit to the hospital. Magnification was calculated by calculating the ratio of the length of the implant fixture to the length of the fixture on the periapical radiographs. The mean amounts of alveolar bone resorption in the mesial and distal implant surfaces were calculated.
Changes in primary and secondary stability were analyzed with a paired t-test. The significance of the differences in the amount of marginal bone loss as determined by implant width and length, dental arch, and placement method were tested using an independent sample t-test at the significant probability of 95% (SPSS Inc., Chicago, IL, USA).
All 154 implants were placed in the posterior area as single restorations. The mean follow-up period was 51.35 ± 24.97 months (minimum 2.53 months; maximum 125.43 months). Of the 154 implants, 7 failed and were removed within 23.28 months after the functional loading, making their survival rate 95.6%. The cause of failure is unclear and various factors such as infection, overload, and insufficient healing time seem to have been involved (Table 2). Implant placement was unsuccessful in 10 implant cases due to excessive marginal bone loss, resulting in a success rate of 93.5%. The mean marginal bone loss around the implants was 0.27 mm at 12 months after the functional loading and 0.76 mm on the last day of follow-up. Primary stability measured with Osstell device was 71.26 ± 16.07 and secondary stability was 77.83 ± 10.01. The increase in primary and secondary stability was statistically significant. Of the 154 implants, 15 resulted in complications including screw loosening, fixture fracture, fixture surface exposure, peri-implantitis, and peri-implant gingivitis.
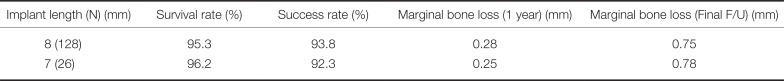
Of the 154 implants, 128 implants were 8 mm in length and 26 implants were 7 mm in length. In the 8 mm group, the mean period of follow-up was 52.1 months, and the mean marginal bone loss was 0.28 mm one year after the functional loading as compared to 0.75 mm at the last hospital visit. Of the 128 implants, 8 implants failed (6 were removed, and 2 had large bone loss), resulting in a success rate of 93.8% and a survival rate of 95.3%. In the 7 mm group, the mean period of follow-up was 47.4 months. The mean marginal bone loss was 0.25 mm one year after the functional loading and 0.78 mm at the last hospital visit. Of the 26 implants, 2 failed (1 was removed and 1 showed severe bone loss), resulting in a success rate of 92.3% and a survival rate of 96.2%. No significant differences in the amount of marginal bone loss, success rate, and survival rate were found between the two groups (P > .05) (Table 3).
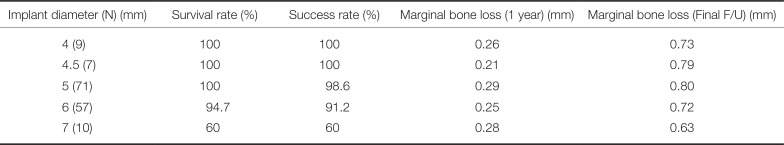
9 implants of 4 mm width, 7 implants of 4.5 mm width, 71 implants of 5.0 mm width, 57 implants of 6 mm width, and 10 implants of 7 mm width were placed. Regarding success and survival rates for each type of implants, the 4 mm- and 4.5 mm-wide implants had success rates and survival rates of 100%. None of the 5 mm-wide implants were removed, but 1 showed severe bone loss, resulting in a survival rate of 100% and a success rate of 98.6%. Of the 6 mm-wide implants, 3 were removed, and 2 showed severe bone loss, resulting in a success rate of 91.2% and a survival rate of 94.7%. Four of the 7 mm-wide implants were removed, and the implants showed success and survival rates of 60% (Table 4).
34 implants were placed in the maxilla and 120 in the mandible. In the maxilla group, the mean period of follow-up was 45 months. The mean marginal bone loss was 0.27 mm one year after functional loading and 0.7 mm at the last hospital visit. One implant was removed, resulting in success and survival rates of 97.1%. In the mandible group, the mean period of follow-up was 53.2 months. The mean marginal bone loss was 0.27 mm one year after functional loading and 0.75 mm at the last hospital visit. 6 implants were removed, and 3 implants showed severe bone loss, resulting in a success rate of 92.5% and a survival rate of 95%. No significant differences were noted in the success rate, survival rate, and the amount of marginal bone loss between the two groups (P > .05) (Table 5).
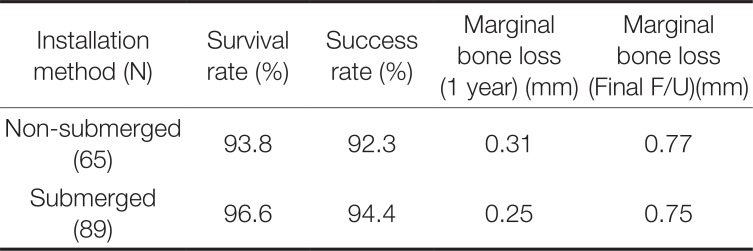
69 implants were non-submerged and 89 were submerged. Primary stability was measured at the time of implant placement and the secondary stability was measured at the time of prosthetic impression taking. A statistically significant difference in the primary and secondary stability measurements was found between the two groups (P < .05). Primary stability ISQ values were 77.67 ± 7.46 and 67.95 ± 15.99 for the non-submerged and submerged group, respectively. Secondary stability ISQ values were 81.37 ± 8.93 and 75.57 ± 10.11, respectively. The mean amount of marginal bone loss one year later was 0.31 ± 0.16 mm in the non-submerged group and 0.25 ± 0.14 mm in the submerged group. The final amount of marginal bone loss was 0.77 ± 0.28 mm in the non-submerged group and 0.75 ± 0.26 mm in the submerged group. The non-submerged implants had a survival rate of 93.8% and a success rate of 92.3%. The submerged implants had a survival rate of 96.6% and a success rate of 94.4%. No significant differences in success rates and survival rates were found between the two groups (Table 6).
Herrmann et al.17 reported a success rate of 78.2% for short implants 7 mm in length and attributed the low success rate to the short implant length. In a study by Weng et al.,18 60% of all implants that failed were short implants less than 10 mm in length, and the cumulative success rate of short implants was significantly lower than that of all implants. According to Telleman et al.,19 the shortest implants were more likely to fail than short implants that were a bit longer in partially edentulous patients, and implants in maxilla had a greater failure rate than implants in mandible. However, in a 14-year cumulative study by Romeo et al.,20 in which 8 mm- and 10 mm-long implants were compared, no significant difference in the amount of marginal bone loss was found, and the success rate of short implant was found to be 97.9% vs 97.1 for the standard implants.
With improvements in implant surface treatment techniques and implant designs, positive prognosis of short implants has been reported. Maló et al.21 reported a high success rate of 96.2% for Brånemark implants 7 mm in length and 97.1% for Brånemark implants 8.5 mm in length in their study using 408 Brånemark implants. In 2012, Kim et al.22 published on the prognosis, prosthetic complications, and factors affecting these results following placement of single short implants in the maxillary and mandibular posterior areas. In a total of 87 patients, 96 single implants were placed. 6 implants failed in osseointegration until the last day of follow up, resulting in a survival rate of 91.1%. All of the failed implants had been placed in the mandibular second molar region. Screw loosening was the most common prosthetic complication and was significantly associated with mesiodistal cantilever. The mean amount of marginal bone loss until the last day of follow-up was 0.2 mm. In conclusion, the success of single implant placement in the maxillary and mandibular posterior areas depends on cantilever minimization and is affected by precise placement of the implant and consistent postoperative management. Kim et al.23 published another retrospective cohort study in 2014 in which they reported the outcomes of single implant placement accompanied by sinus lifting in the maxilla. This study showed that maxillary sinusitis can affect the prognosis of implant placement accompanied by sinus lifting in the maxilla. 8 mm long short implants also showed relatively good results. In this study, a total of 154 implants that measured less than 8 mm in length were analyzed. Of all the implants, 7 led to fail in osseointegration, resulting in a mean survival rate of 95.6%. Three implants were considered unsuccessful because they did not meet the standard regarding the amount of marginal bone loss, resulting in a mean success rate of 93.5%. The mean amount of bone absorption was 0.27 mm one year after the functional loading and 0.76 mm on the last day of follow-up. No significant difference in outcome was found between the 7 mm- and 8 mm-long single implants in this study. Reasons for implant removal were infection, overload, and insufficient healing period. Implant failure appeared to be insignificantly associated with implant length. During implantation, preventive measures are important for preventing implant failures, which include disinfecting the wound area following surgery, appropriate use of antibiotics, determination of an appropriate amount of healing time, and timing of functional loading.
Since this study only included single implants, it was not possible to compare them to splinted crowns. Of the total of 154 implants included in this study, 65 were placed using the one-stage approach and 89 using the two-stage approach. Primary and secondary stability were found to be significantly higher in the implants using the one-stage approach. However, there were no statistically significant differences between the groups with regard to the amount of marginal bone loss, survival rate, and success rate. The values for primary stability and secondary stability were all within a stable range, and a notable increase in secondary stability was observed after a certain amount of time elapsed after the healing period. The primary stability of the submerged type implants was greater than that of the non-submerged type in this study; this was possibly because in the two-stage approach, submerged type implants are often placed when primary stability is low. Implant stability was observed to increase for all the implants over time, and no significant differences in survival rates and the amount of marginal bone loss were observed between the two placement methods. Therefore, placement methods and healing time may not affect implant prognosis if the outcomes are determined according to the bone quality and primary stability at the time of surgery.
The maxilla has a relatively low bone density and is soft. As a result, the failure rate of short implants is higher in the maxilla than in the mandible.234 Therefore, it is advisable to perform the second surgery after a healing period of approximately 6 months, after which the prosthetic treatment in the maxilla can be completed. However, the mandibular alveolar bone is dense and the initial fixation is firm, so implants can be placed by using the one-stage, non-submerged method. The prosthetic treatment can begin after a 2 – 3 month healing period. Various results have been reported with regard to changes in the success rate of short implants depending on whether one-stage or two-stage placement was performed. Gentile et al.5 reported higher success rates for short implants placed through the two-stage placement method. However, Sun et al.6 reported no difference in success rates between one-stage and two-stage placement methods.
Several studies have reported that the diameter of an implant plays an important role in primary stability and implant prognosis.2425 In this study, while no significant difference in the amount of marginal bone loss was observed according to implant diameter, the survival and success rates of the 6 mm- and 7 mm-wide implants were lower than those of the 5 mm-wide implants. In this study, the implants were divided into several groups according to their diameter as follows: 4 mm group (n = 9), 4.5 mm group (n = 7), 5.0 mm group (n = 71), 6 mm group (n = 57), and 7 mm group (n = 10). No significant differences were found among the groups in the amount of marginal bone loss, survival rate, or in the success rate.
This study had several limitations. First, it was difficult to perform a standardized statistical analysis since all the data were retrospectively analyzed. Furthermore, we did not perform an analysis on cantilever and crown/implant ratio. There was a problem that the statistical comparison was difficult because the sample difference between the groups was large. Future research designs must be standardized, and prospective clinical research must be conducted to produce meaningful results.
References
1. Misch CE, Suzuki JB, Misch-Dietsh FM, Bidez MW. A positive correlation between occlusal trauma and peri-implant bone loss: literature support. Implant Dent. 2005; 14:108–116. PMID: 15968181.

2. Rocci A, Martignoni M, Gottlow J. Immediate loading of Brånemark System TiUnite and machined-surface implants in the posterior mandible: a randomized open-ended clinical trial. Clin Implant Dent Relat Res. 2003; 5(Suppl 1):57–63.

3. Glauser R, Lundgren AK, Gottlow J, Sennerby L, Portmann M, Ruhstaller P, Hämmerle CH. Immediate occlusal loading of Brånemark TiUnite implants placed predominantly in soft bone: 1-year results of a prospective clinical study. Clin Implant Dent Relat Res. 2003; 5(Suppl 1):47–56.

4. Sun HL, Huang C, Wu YR, Shi B. Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: a systematic review. Int J Oral Maxillofac Implants. 2011; 26:816–825. PMID: 21841992.
5. Gentile MA, Chuang SK, Dodson TB. Survival estimates and risk factors for failure with 6 × 5.7-mm implants. Int J Oral Maxillofac Implants. 2005; 20:930–937. PMID: 16392351.
6. Chan MF, Närhi TO, de Baat C, Kalk W. Treatment of the atrophic edentulous maxilla with implant-supported overdentures: a review of the literature. Int J Prosthodont. 1998; 11:7–15. PMID: 9588985.
7. Misch CE. Short dental implants: a literature review and rationale for use. Dent Today. 2005; 24:64–66. 68
8. Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. A retrospective analysis of 800 Brånemark System implants following the All-on-Four™ protocol. J Prosthodont. 2014; 23:83–88. PMID: 23890014.

9. Annibali S, Cristalli MP, Dell'Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. J Dent Res. 2012; 91:25–32. PMID: 22034499.
10. Mendonça JA, Francischone CE, Senna PM, Matosde Oliveira AE, Sotto-Maior BS. A retrospective evaluation of the survival rates of splinted and non-splinted short dental implants in posterior partially edentulous jaws. J Periodontol. 2014; 85:787–794. PMID: 24171498.

11. Antoun H, Cherfane P, Sojod B. Consecutive Case Series of Healed Single-Molar Sites Immediately Restored with Wide-Diameter Implants: A 1-Year Evaluation. Int J Dent. 2016; 2016:5645892. PMID: 27195008.

12. Calandriello R, Tomatis M. Immediate occlusal loading of single lower molars using Brånemark System® Wide Platform TiUnite™ implants: a 5-year follow-up report of a prospective clinical multicenter study. Clin Implant Dent Relat Res. 2011; 13:311–318. PMID: 19673926.

13. Fugazzotto PA, Vlassis J, Butler B. ITI implant use in private practice: Clinical results with 5,526 implants followed up to 72+ months in function. Int J Oral Maxillofac Implants. 2004; 19:408–412. PMID: 15214226.
14. Malmstrom H, Gupta B, Ghanem A, Cacciato R, Ren Y, Romanos GE. Success rate of short dental implants supporting single crowns and fixed bridges. Clin Oral Implants Res. 2016; 27:1093–1098. PMID: 26391214.

15. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25. PMID: 3527955.
16. Zarb GA, Albrektsson T. Consensus report: towards optimized treatment outcomes for dental implants. J Prosthet Dent. 1998; 80:641. PMID: 9830066.
17. Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. Int J Oral Maxillofac Implants. 2005; 20:220–230. PMID: 15839115.
18. Weng D, Jacobson Z, Tarnow D, Hürzeler MB, Faehn O, Sanavi F, Barkvoll P, Stach RM. A prospective multicenter clinical trial of 3i machined-surface implants: results after 6 years of follow-up. Int J Oral Maxillofac Implants. 2003; 18:417–423. PMID: 12814318.
19. Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol. 2011; 38:667–676. PMID: 21564158.
20. Romeo E, Ghisolfi M, Rozza R, Chiapasco M, Lops D. Short (8-mm) dental implants in the rehabilitation of partial and complete edentulism: a 3- to 14-year longitudinal study. Int J Prosthodont. 2006; 19:586–592. PMID: 17165298.
21. Maló P, de Araújo Nobre M, Rangert B. Short implants placed one-stage in maxillae and mandibles: a retrospective clinical study with 1 to 9 years of follow-up. Clin Implant Dent Relat Res. 2007; 9:15–21. PMID: 17362493.

22. Kim YK, Kim SG, Yun PY, Hwang JW, Son MK. Prognosis of single molar implants: a retrospective study. Int J Periodontics Restorative Dent. 2010; 30:401–407. PMID: 20664842.
23. Kim YK, Ahn KJ, Yun PY. A retrospective study on the prognosis of single implant placed at the sinus bone graft site. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014; 118:181–186. PMID: 23838074.

24. Isidor F. Clinical probing and radiographic assessment in relation to the histologic bone level at oral implants in monkeys. Clin Oral Implants Res. 1997; 8:255–264. PMID: 9586471.
25. Yilmaz B, Seidt JD, McGlumphy EA, Clelland NL. Comparison of strains for splinted and nonsplinted screw-retained prostheses on short implants. Int J Oral Maxillofac Implants. 2011; 26:1176–1182. PMID: 22167421.
Table 1
Distribution of installed short implants
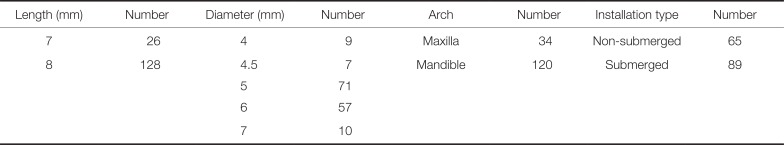
| Length (mm) | Number | Diameter (mm) | Number | Arch | Number | Installation type | Number |
|---|---|---|---|---|---|---|---|
| 7 | 26 | 4 | 9 | Maxilla | 34 | Non-submerged | 65 |
| 8 | 128 | 4.5 | 7 | Mandible | 120 | Submerged | 89 |
| 5 | 71 | ||||||
| 6 | 57 | ||||||
| 7 | 10 |
Table 2
Removed implants
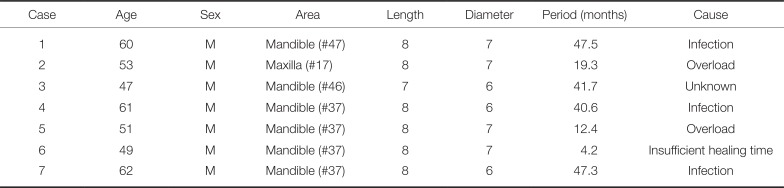
Table 3
Comparison by implant length
| Implant length (N) (mm) | Survival rate (%) | Success rate (%) | Marginal bone loss (1 year) (mm) | Marginal bone loss (Final F/U) (mm) |
|---|---|---|---|---|
| 8 (128) | 95.3 | 93.8 | 0.28 | 0.75 |
| 7 (26) | 96.2 | 92.3 | 0.25 | 0.78 |
Table 4
Comparison by implant diameter




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download