1. Edwards MS, Baker CJ. Mandell GL, Bennett JE, Dolin R, editors. Streptococcus agalactiae. Principles and practice of infectious diseases. 2005. 3rd ed. Philadelphia: Elsevier. Churchill Livingstone;2423–2434.
2. Edward MS, Nizet V, Baker CJ. Remington JS, Klien JO, Baker CJ, Wilson CB, editors. Group B streptococcal infection. Infectious diseases of the fetus and newborn infant. 2006. 6th ed. Philadelphia: WB Saunders Co;1091–1141.
3. Boyer KM, Gadzala CA, Kelly PD, Burd LI, Gotoff SP. Selective intrapartum chemoprophylaxis of neonatal group B streptococcal early-onset disease. II. Predictive value of prenatal cultures. J Infect Dis. 1983. 148:802–809.

4. Hood M, Janney A, Dameron G. Beta hemolytic streptococcus group B associated with problems of the perinatal period. Am J Obstet Gynecol. 1961. 82:809–818.

5. Baker CJ, Barrett FF. Transmission of group B streptococci among parturient women and their neonates. J Pediatr. 1973. 83:919–925.

6. Franciosi RA, Knostman JD, Zimmerman RA. Group B streptococcal neonatal and infant infections. J Pediatr. 1973. 82:707–718.

7. Kim KA, Shin SM, Choi JH. A nationwide survey on the causative organisms of neonatal sepsis in Korea. J Korean Pediatr Soc. 2002. 45:55–63.
8. Lee JH, Cho HK, Kim KH, Kim CH, Kim DS, Kim KN, et al. Etiology of invasive bacterial infections in immunocompetent children in Korea (1996-2005): a retrospective multicenter study. J Korean Med Sci. 2011. 26:174–183.

9. Baker CJ, Barrett FF. Group B streptococcal infections in infants. The importance of the various serotypes. JAMA. 1974. 230:1158–1160.

10. Phares CR, Lynfield R, Farley MM, Mohle-Boetani J, Harrison LH, Petit S, et al. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. JAMA. 2008. 299:2056–2065.

11. Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, et al. Group B streptococcal disease in the era of intra-partum antibiotic prophylaxis. N Engl J Med. 2000. 342:15–20.

12. Verani JR, Schrag SJ. Group B streptococcal disease in infants: progress in prevention and continued challenges. Clin Perinatol. 2010. 37:375–392.

13. Edwards MS, Baker CJ. Long SS, Pickering LK, Prober CG, editors. Streptococcus agalactiae (Group B Streptococcus). Principles and practice of pediatric infectious diseases revised reprint. 2009. 3rd ed. Philadelphia: Elsevier, Churchill Livingstone;711–716.
14. Godambe S, Shah PS, Shah V. Breast milk as a source of late onset neonatal sepsis. Pediatr Infect Dis J. 2005. 24:381–382.

15. Hickman ME, Rench MA, Ferrieri P, Baker CJ. Changing epidemiology of group B streptococcal colonization. Pediatrics. 1999. 104:203–209.

16. Campbell JR, Hillier SL, Krohn MA, Ferrieri P, Zaleznik DF, Baker CJ. Group B streptococcal colonization and serotype-specific immunity in pregnant women at delivery. Obstet Gynecol. 2000. 96:498–503.

17. Yancey MK, Schuchat A, Brown LK, Ventura VL, Markenson GR. The accuracy of late antenatal screening cultures in predicting genital group B streptococcal colonization at delivery. Obstet Gynecol. 1996. 88:811–815.

18. Kim MW, Jang HO, Chang DY, Cho JR, Kim YA, Choi HM, et al. Group B streptococcal colonization rate in Korean pregnant women. Korean J Obstet Gynecol. 2006. 49:337–344.
19. Uh Y, Jang IH, Yoon KJ, Lee CH, Kwon JY, Kim MC. Colonization rates and serotypes of group B streptococci isolated from pregnant women in a Korean tertiary hospital. Eur J Clin Microbiol Infect Dis. 1997. 16:753–756.

20. Uh Y, Kwon JY, Jang IH, Yoon KJ, Kim HK. Colonization rate of group B streptococcus in pregnant women and neonates. Korean J Clin Pathol. 1994. 14:447–453.
21. Park LS, Seo K, Kim SK, Park YW, Jung HY, Chong YS, et al. A study of group B streptococcal infection in Korean pregnant women. Korean J Obstet Gynecol. 1999. 42:2038–2042.
22. Uh Y, Choi SJ, Jang IH, Lee KS, Cho HM, Kwon O, et al. Colonization rate, serotypes, and distributions of macrolide-lincosamide-streptograminB resistant types of group B streptococci in pregnant women. Korean J Clin Microbiol. 2009. 12:174–179.

23. Oh CE, Jang HO, Kim NH, Lee J, Choi EH, Lee HJ. Molecular serotyping of group B streptococcus isolated from the pregnant women by polymerase chain reaction and sequence analysis. Korean J Pediatr Infect Dis. 2009. 16:47–53.

24. Hong JS, Choi CW, Park KU, Kim SN, Lee HJ, Lee HR, et al. Genital group B streptococcus carrier rate and serotype distribution in Korean pregnant women: implications for group B streptococcal disease in Korean neonates. J Perinat Med. 2010. 38:373–377.

25. Yoon HK, Song PJ, Choi KC, Ju JR, Cho BS, Jung SJ. A case of neonatal meningitis by group B streptococcus. J Korean Pediatr Soc. 1984. 27:1011–1017.
26. Kim YK, Kwak YH, Kim YJ, Jung HS, Hong JY, Lee HJ. Clinical features of group B β-hemolytic streptococcal infection in infants and children. Korean J Pediatr Infect Dis. 1999. 6:194–202.

27. Kim HJ, Lee JW, Lee KY, Lee HS, Hong JH, Hahn SH. Causative organisms in children with bacterial meningitis (1992-2002). J Korean Pediatr Soc. 2003. 46:1085–1088.
28. Cho HK, Lee H, Kang JH, Kim KN, Kim DS, Kim YK, et al. The causative organisms of bacterial meningitis in Korean children in 1996-2005. J Korean Med Sci. 2010. 25:895–899.

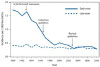
29. Centers for Disease Control and Prevention. Trends in perinatal group B streptococcal disease - United States, 2000-2006. MMWR Morb Mortal Wkly Rep. 2009. 58:109–112.
30. Jordan HT, Farley MM, Craig A, Mohle-Boetani J, Harrison LH, Petit S, et al. Revisiting the need for vaccine prevention of late-onset neonatal group B streptococcal disease: a multistate, population-based analysis. Pediatr Infect Dis J. 2008. 27:1057–1064.

31. Edmond KM, Kortsalioudaki C, Scott S, Schrag SJ, Zaidi AK, Cousens S, et al. Group B streptococcal disease in infants aged younger than 3 months: systematic review and meta-analysis. Lancet. 2012. 379:547–556.

32. Kim JS, Jang YT, Kim JD, Park TH, Park JM, Kilgore PE, et al. Incidence of
Haemophilus influenzae type b and other invasive diseases in South Korean children. Vaccine. 2004. 22:3952–3962.

33. Lee JH, Kim SM, Lee HS, Kim SY, Choi SD, Sung IK, et al. A clinical study of group B streptococcal infection: five year experience. J Korean Soc Neonatol. 2003. 10:226–234.
34. Park KH, Kim KH, Kang JH, Kim KN, Kim DS, Kim YK, et al. Current status and clinical presentations of invasive neonatal group B streptococcal infections in Korea. Pediatr Int. 2011. 53:236–239.

35. Slotved HC, Kong F, Lambertsen L, Sauer S, Gilbert GL. Serotype IX, a proposed new
Streptococcus agalactiae serotype. J Clin Microbiol. 2007. 45:2929–2936.

36. Seo YS, Srinivasan U, Oh KY, Shin JH, Chae JD, Kim MY, et al. Changing Molecular Epidemiology of Group B Streptococcus in Korea. J Korean Med Sci. 2010. 25:817–823.

37. Boyer KM, Gotoff SP. Prevention of early-onset neonatal group B streptococcal disease with selective intrapartum chemoprophylaxis. N Engl J Med. 1986. 314:1665–1669.

38. Lim DV, Morales WJ, Walsh AF, Kazanis D. Reduction of morbidity and mortality rates for neonatal group B streptococcal disease through early diagnosis and chemoprophylaxis. J Clin Microbiol. 1986. 23:489–492.

39. Centers for Disease Control and Prevention. Prevention of perinatal group B streptococcal disease: a public health perspective. MMWR Recomm Rep. 1996. 45(RR-7):1–24.
40. Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002. 51(RR-11):1–22.
41. Centers for Disease Control and Prevention. Perinatal group B streptococcal disease after universal screening recommendations-United States, 2003-2005. MMWR Morb Mortal Wkly Rep. 2007. 56:701–705.
42. Verani JR, McGee L, Schrag SJ. Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease--revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010. 59(RR-10):1–36.
43. de Cueto M, Sanchez MJ, Sampedro A, Miranda JA, Herruzo AJ, Rosa-Fraile M. Timing of intrapartum ampicillin and prevention of vertical transmission of group B Streptococcus. Obstet Gynecol. 1998. 91:112–114.

44. Lin FY, Brenner RA, Johnson YR, Azimi PH, Philips JB 3rd, Regan JA, et al. The effectiveness of risk-based intrapartum chemoprophylaxis for the prevention of early-onset neonatal group B streptococcal disease. Am J Obstet Gynecol. 2001. 184:1204–1210.

45. Fiore Mitchell T, Pearlman MD, Chapman RL, Bhatt-Mehta V, Faix RG. Maternal and transplacental pharmacokinetics of cefazolin. Obstet Gynecol. 2001. 98:1075–1079.

46. Kelkar PS, Li JT. Cephalosporin allergy. N Engl J Med. 2001. 345:804–809.

47. Van Dyke MK, Phares CR, Lynfield R, Thomas AR, Arnold KE, Craig AS, et al. Evaluation of universal antenatal screening for group B streptococcus. N Engl J Med. 2009. 360:2626–2636.

48. Melin P. Neonatal group B streptococcal disease: from pathogenesis to preventive strategies. Clin Microbiol Infect. 2011. 17:1294–1303.

49. Baker CJ, Kasper DL. Correlation of maternal antibody deficiency with susceptibility to neonatal group B streptococcal infection. N Engl J Med. 1976. 294:753–756.

50. Baker CJ, Rench MA, McInnes P. Immunization of pregnant women with group B streptococcal type III capsular polysaccharide-tetanus toxoid conjugate vaccine. Vaccine. 2003. 21:3468–3472.

51. Baker C, Edwards M. Group B streptococcal conjugate vaccines. Arch Dis Child. 2003. 88:375–378.

52. Baker CJ, Paoletti LC, Wessels MR, Guttormsen HK, Rench MA, Hickman ME, et al. Safety and immunogenicity of capsular polysaccharide-tetanus toxoid conjugate vaccines for group B streptococcal types Ia and Ib. J Infect Dis. 1999. 179:142–150.

53. Baker CJ, Paoletti LC, Rench MA, Guttormsen HK, Carey VJ, Hickman ME, et al. Use of capsular polysaccharide-tetanus toxoid conjugate vaccine for type II group B Streptococcus in healthy women. J Infect Dis. 2000. 182:1129–1138.

54. Margarit I, Rinaudo CD, Galeotti CL, Maione D, Ghezzo C, Buttazzoni E, et al. Preventing bacterial infections with pilus-based vaccines: the group B streptococcus paradigm. J Infect Dis. 2009. 199:108–115.

55. Choi KU, Koh SK, Lee JY, Park JH, Hwang SO, Lee BI, et al. Clinical Significance of Group B Streptococcal Infection in Pregnant Women. Korean J Obstet Gynecol. 2002. 45:811–815.
56. Lee SH, Park KU, Lee HK, Kim MY, Kim JY, Kwon WK, et al. Perineal colonization rate and antimicrobial susceptibility of group B streptococcus in pregnant and non-pregnant Korean women. Korean J Clin Microbiol. 2009. 12:180–185.

57. Seo YS, Srinivasan U, Oh KY, Shin JH, Chae JD, Kim MY, et al. Changing molecular epidemiology of group B streptococcus in Korea. J Korean Med Sci. 2010. 25:817–823.

58. Pannaraj PS, Baker CJ. Feigin RD, Cherry J, Demmeler-Harrison GJ, Kaplan SL, editors. Group B streptococcal infections. Feigin and Cherry's textbook of pediatric infectious diseases. 2009. 6th ed. Philadelphia: WB Saunders Co;1239–1257.

59. Swingle HM, Bucciarfelli RL, Ayoub EM. Synergy between penicillins and low concentrations of gentamicin in the killing of group B streptococci. J Infect Dis. 1985. 152:515–520.








 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download