Abstract
Purpose
The aim of this study is to investigate the colonization rate of Methicillin-resistant Staphylococcus aureus (MRSA) in neonates by different clinical characteristics, to presume the origin of MRSA acquisition, and to identify the risk factors associated with MRSA colonization.
Methods
We retrospectively reviewed the medical records of 1,733 neonates admitted to Seoul Eulji hospital Neonatal Intensive Care Unit between January 2008 and December 2011. Nasal, inguinal and rectal swab specimens were obtained upon admission and each week until discharge. We classified the route of MRSA acquisition as; hospital associated (HA-MRSA) and community associated (CA-MRSA) according to the case definition.
Results
Among 1,733 neonates, 415 (23.9%) were colonized with MRSA. Gestational age, birth weight, delivery type, maternal antibiotics usage before delivery, birth place and care place before admission were influencing factors in colonization of MRSA. The colonization rate was significantly high in neonates without maternal prophylactic antibiotics use before delivery than in the other group (relative risk 2.77, 95% CI 1.88-4.07; P<0.01), and outborns showed higher MRSA colonization rate compared to inborns (relative risk 2.28, 95% CI 1.17-4.42; P=0.015).
Conclusion
We identified the neonatal MRSA colonization rate to be 23.9%. We estimated HA-MRSA colonization rate to be 10% (51/511) and CA-MRSA colonization rate to be 36% (309/858). We ascertained that risk factors in MRSA colonization in neonates were prophylactic use of antibiotics in mothers and the birth place.
Figures and Tables
Fig. 1
Kaplan-Meier estimated cumulative probability of methicillin-resistant Staphylococcus aureus colonization free staus in hospitalized neonates by birth weight group. Neonates less 1,500 g were methicillin-resistant Staphylococcus aureus non-colonizer when they were admitted. But they rapidly became methicillin-resistant Staphylococcus aureus colonizer over time. Most neonates excess 2,500 g tended to be methicillin-resistant Staphylococcus aureus colonizer when they admitted.
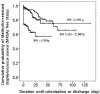
Fig. 2
Kaplan-Meier estimated cumulative probability of methicillin-resistant Staphylococcus aureus colonization free status in hospitalized neonates by care place group. Neonates from community had shorter hospitalized days than inborn neonates. Inborn neonates became methicillin-resistant Staphylococcus aureus colonizer over time. Community means home, private facility (Joriwon) or public facility.
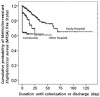
Table 1
Methicilin-resistant Staphylococcus aureus Colonization Rates in Neonates according to Clinical Characteristics

Table 2
Methicilin-resistant Staphylococcus aureus Colonization Rates in Neonates by Invasive Procedures

References
1. Wertheim HF, Melles DC, Vos MC, Van Leewen WU, Vasn Belkum AV, Verbrugh HA, et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005. 5:751–762.
2. Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998. 339:520–532.
3. Song X, Perencevich E, Campos J, Short B, Singh N. Clinical and economic impact of methicillin-resistant Staphylococcus aureus colonization or infection on neonates in intensive care units. Infect Control Hosp Epidemiol. 2010. 31:177–182.

4. Lessa FC, Edwards JR, Fridkin SK, Tenover FC, Horan TC, Gorwitz RJ. Trends in incidence of late-onset methicillin-resistant Staphylococcus aureus infection in neonatal intensive care units: data from the National Nosocomial infections Surveillance System, 1995-2004. Pediatr infect Dis J. 2009. 28:577–581.

5. Maraqa NF, Aigbivbalu L, Masnita-lusan C, Wludyka P, Shareef Z, Bailey C, et al. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus colonization and infection among infants at a level III neonatal intensive care unit. Am J Infect Control. 2011. 39:35–41.

6. Chung MK, Choi JH, Chang JK, Chung SH, Bae CW, Cha SH. Clinical characteristics and risk factors for staphylococcal infections in neonatal intensive care unit. Korean J Pediatr. 2006. 49:1287–1295.

7. Park J, Kim S, Lee J. Infection of methicillin-resistant S. aureus nasal carriage in the community pediatric population. Korean J Epidemiol. 2006. 28:171–181.
8. Kim DH, Kim SM, Park JY, Cho EY, Choi CH. Characteristics of methicillin-resistant Staphylococcus aureus nasal colonization among neonatal unit staffs and infection control measures. Korean J Pediatr Infect Dis. 2009. 16:131–141.
9. Na DC, Seo JM, Lee JH, Lee WU, Kim ER. Carriage rates of methicillin-resistant Staphylococcus aureus in neonates with neonatal jaundice. Korean J Pediatr Infect Dis. 2011. 18:143–153.

10. Regev-Yochay G, Rubinstein E, Barzilai A, Carmeli Y, Kuint J, Etienne J, et al. Methicilin-resistant Staphylococcus aureus in neonatal intensive care unit. Emerg Infect Dis. 2005. 11:453–456.

11. McHugh CG, Riley LW. Risk factors and costs associated with methicillin-reskstant Staphylococcus aureus bloodstream infections. Infect Control Hosp Epidemiol. 2004. 25:425–430.

12. Von Baum H, Schmidt C, Svoboda D, Bock-Hensley O, Wendt C. Risk factors for methicillin-resistant Staphylococcus aureus carriage in residents of German nursing homes. Infect Control Hosp Epidemiol. 2002. 23:511–515.
13. Clinical and Laboratory Standards Institute. 18th informational supplement, M100-S18. Performance standards for antimicrobial susceptibility testing. 2008. Wayne, PA: CLSI.
14. Kim CR, Kim SY, Park HJ, Ki MR, Yoon HS. Risk factors of nosocomial sepsis in very low birth weight infants. J Korean Soc Neonatol. 2010. 17:84–93.
15. Davis KA, Stewart JJ, Crouch HK, Florez CE, Hospenthal DR. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis. 2004. 39:776–782.

16. Huang SS, Platt R. Risk of methicillin-resistant Staphylococcus aureus infection after previous infection or colonization. Clin Infect Dis. 2003. 36:281–285.

17. Garrouste-Orgeas M, Timsit JF, Kallel H, Ben AA, Dumay MF, Paoli B. Colonization with methicillin-resistant Staphylococcus aureus in ICU patients: morbidity, mortality and glycopeptides use. Infect Control Hosp Epidemiol. 2001. 22:687–692.

18. Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, Fosheim GE, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001-2004. J infect Dis. 2008. 197:1226–1234.

19. Chaix C, Durand-Zaleski I, Alberti C, Brun-Burisson C. Control of endemic methicillin-resistant Staphylococcus aureus: a cost-benefit analysis in an intensive care unit. JAMA. 1999. 282:1745–1751.

20. Alfaro C, Mascher-Denen M, Fergie J, Purcell K. Prevalence of methicillin-resistant Staphylococcus aureus nasal carriage in patients admitted to Driscoll children's hospital. Pediatr Infect Dis J. 2006. 25:459–461.

21. Kim YM, Oh CE, Kim SH, Lee J, Choi EH, Lee HJ. Nasal carriage of Staphylococcus aureus from healthy children attending day care center. Korean J Pediatr Infect Dis. 2010. 17:9–15.

22. Kim HJ, Kang SJ, Park HK, Kim CR, Choi TY, Oh SH. The effect of eradication of methicillin-resistatant Staphylococcus aureus from neonatal intensive care unit by aggressive infection control measures: isolation program and the use of chlorhexidine. Korean J Perinatol. 2010. 21:248–257.
23. From the centers for disease control and prevention. Four pediatric deaths from community-aquired methicillin-resistant Staphylococcus aureus-Minnesota and North Dakota, 1997-1999. JAMA. 1999. 282:1123–1125.
24. Seybold U, Halvosa JS, White N, Voris V, Ray SM, Blumberg HM. Emergence of and risk factors for methicillin-resistant Staphylococcus aureus of community origin in intensive care nurseries. Pediatrics. 2008. 122:1039–1046.

25. Al-Tawfiq JA. Father-to-Infant transmission of community-acquired methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2006. 27:636–637.

26. Chen KT, Huard RC, Della-Latta P, Saiman L. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet Gynecol. 2006. 108:482–487.

27. Centers for Disease Control and Prevention. Community-associated methicillin-resistant Staphylococcus aureus infection among healthy newborns-Chicago and Los Angeles County, 2004. MMWR Morb Mortal Wkly Rep. 2006. 55:329–332.
28. Verani JR, MaGee L, Schrag SJ. Prevention of perinatal group B Streptococcal disease-revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010. 59:1–36.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download