Abstract
Purpose
Varicella Zoster Immune Globulin (VZIG) is available in Korea for post-exposure prophylaxis of the Varicella-zoster virus (VZV) in high-risk patients. In July 2013, the United States Centers for Disease Control and Prevention (US CDC) recommended extending the time for administration of VariZIG® from within 96 hours up to 10 days after VZV exposure. This study was performed to analyze the effectiveness of VZIG prophylaxis between the two groups of patients who received VZIG within 96 hours and more than 96 hours of exposure to varicella.
Methods
A retrospective chart review was performed in pediatric patients who received VZIG at Samsung Medical Center, Seoul, Korea from January 2001 to December 2012.
Results
A total of 91 patients were identified. Fifty-seven patients were male (62.6%) and the median age was 5.91 years. Thirty-nine patients (42.9%) were exposed to VZV in the hospital. Underlying diseases were solid tumors (41.8%), hematologic malignancies (40.7%), and others (17.5%). Forty-five patients (49.5%) were hematopoietic cell transplant recipients. Seventy-four patients (81.3%) received VZIG within 96 hours after VZV exposure. There was no significant difference in the development of chickenpox between the two groups (2.7% vs. 5.9%, P=0.4664). In 22 seronegative patients, we also observed no significant difference between the groups in terms of the development of chickenpox (6.6% vs. 0%, P=0.667).
Varicella (i.e., chickenpox) is a highly infectious disease caused by the Varicella-zoster virus (VZV). Secondary attack rates for this virus may reach 90% in susceptible household contacts1). Varicella can be severely dangerous in immunocompromised children23). Although the disease can be prevented by vaccination, the varicella vaccine, which contains live attenuated virus, is generally contraindicated for immunocompromised hosts4).
Post-exposure prophylaxis of varicella is recommended in high-risk groups such as immunocompromised patients, newborns, and pregnant women5). Varicella-Zoster Immune Globulins reduce the severity of VZV infections. Zoster Immune Globulin (ZIG), Varicella Zoster Immune Globulin (VZIG) and VariZIG ® are all Varicella-Zoster Immune Globulins6). In Korea, only VZIG is currently available for patient use, not VariZIG ®.
In July 2013, the United States Center for Disease Control (US CDC) recommended extending the time for administration of VariZIG ® beyond the 96 hourtime point for up to 10 days after VZV exposure, based on data from published literature67891011). This study was performed to comparatively analyze the effectiveness of VZIG prophylaxis between patients who received VZIG within 96 hours and patients who received VZIG more than 96 hours after exposure.
A retrospective chart review was performed in pediatric patients who received VZIG at Samsung Medical Center, Seoul, Korea from January 2001 to December 2012. Although the recommendation in our center for high risk patients who were exposed to VZV was to administer VZIG within 96 hours, there were certain cases that the VZIG was administered when time had passed more than 96 hours after the exposure. Patients were divided into two groups based on the time between varicella exposure and VZIG administration: patients who received VZIG within 96 hours of varicella exposure and patients who received VZIG more than 96 hours after varicella exposure. Median days from exposure to VZIG administration between two groups were compared using the Mann-Whitney test. Rates of chickenpox development in two groups were compared using Fisher's exact test.
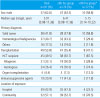
The clinical characteristics of patients are shown in Table 1. A total of 91 patients were identified. The underlying diseases of patients were solid tumors (n=38, 41.8%), hematological malignancies (n=37, 40.7%), and others (n=16, 17.5%). Solid tumors included neuroblastoma (n=13), medulloblastoma (n=4), retinoblastoma (n=4), rhabdomyosarcoma (n=4), hepatoblastoma (n= 3), primitive neuroectodermal tumor (n=3), germ cell tumor (n=2), hemangioendothelioma (n=1), Wilms tumor (n=1), synovial sarcoma (n=1), Ewing sarcoma (n=1), osteosarcoma (n=1) and craniopharyngioma (n=1). Hematologic malignancies included acute lymphoblastic leukemia (ALL, n=27), acute myeloid leukemia (n=7), juvenile myelomonocytic leukemia (n=1), lymphoma (n=1) and severe aplastic anemia (n=1). Other diseases included biliary atresia (n=5), systemic lupus erythematosus (n=2), severe combined immunodeficiency (n=1), Wiskott-Aldrich syndrome (n=1), Langerhans cell histiocytosis (n=1), idiopathic pulmonary hemosiderosis (n=1), multiple sclerosis (n=1), mucopolysaccharidosis (n=1), and chronic granulomatous disease (n=1). Immunosuppressive agents included tacrolimus, prednisolone, cyclosporine and mycophenolate.
Patients were divided into two groups, as shown in Table 1, based on the time of VZIG administration after exposure to VZV from varicella. Seventy-four patients (81.3%) received VZIG within 96 hours of exposure and 17 (18.7%) received it after 96 hours. In the within 96 hours group, the median number of days from exposure to VZIG administration was 3 (range, 1–4 days) and in the more than 96 hours group, the median number of days was 5 (range, 5–16 days; P<0.0001). One patient received VZIG 16 days after exposure.
Of the patients who received VZIG within 96 hours, two of 74 patients (2.7%) developed chickenpox. Of the patients who received VZIG more than 96 hours after exposure, one out of 17 patients (5.9%) developed chickenpox. There was no significant difference in chickenpox development between the two groups (P=0.4664, Fisher's exact test). None of these three patients who developed chickenpox experienced any serious complications.
Two patients who received VZIG within 96 hours, and developed chickenpox, were treated with intravenous acyclovir in the general ward without any severe complications. One allogeneic hematopoietic cell transplant (HCT) recipient was exposed to VZV in the hospital. At that time, he was receiving intravenous foscarnet for CMV retinitis and prednisolone for graftversus- host disease. He received VZIG 4 days after exposure and continued foscarnet for an additional 2 weeks to control the CMV infection. Eleven days after his last foscarnet therapy (24 days after VZIG), he was admitted to the hospital with chickenpox. Initially he was treated with oral acyclovir for 3 days at an outpatient clinic. However, due to an increasing number of vesicles, he was eventually hospitalized and treated with intravenous acyclovir for 7 days. Another patient with ALL was exposed to VZV at home. She received VZIG 4 days after exposure. The patient developed chickenpox 18 days after administration of VZIG and was treated with oral acyclovir for 4 days at an outpatient clinic before being hospitalized and treated with intravenous acyclovir for 10 days.
The patient who received VZIG after 96 hours and developed chickenpox was treated at an outpatient clinic. He was exposed to VZV at school. He was 3 months after finishing chemotherapy for his ALL. He received VZIG 5 days after exposure and developed chickenpox 13 days after VZIG administration. He was treated with oral acyclovir for 7 days at an outpatient clinic.
One patient was exposed to VZV at home. She received VZIG 16 days after exposure to VZV, which occurred 2 years after finishing chemotherapy and autologous HCT for an immature teratoma in her right ovary with lung metastasis. She did not develop chickenpox.
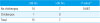
By enzyme-linked immunosorbent assay (ELISA) test, negative IgG was observed in 22 of the 57 patients for whom VZV IgG serology was available (38.6%, Table 2). There was no significant difference in the development of clinical chickenpox between different VZIG administration timing groups in seronegative patients (6.6% vs. 0%, P=0.667).
The rate of chickenpox development according to previously published literature is reviewed in Table 3. In the studies from 1978 and 1980, ZIG was administered as a post-exposure prophylaxis of varicella. VZIG was administered in the studies from 2000 and 2002.
In this study, we found that the effectiveness of VZIG in preventing chickenpox was comparable between patients who received VZIG within 96 hours and those who received it more than 96 hours after exposure to VZV from varicella (2.7% vs. 5.9%,P=0.4664).
Primary VZV infection in healthy children usually follows a mild clinical course and serious complications are rare12). In immunocompetent children, varicella is generally a self-limited illness that lasts 4–5 days and presents itself as fever, malaise, and vesicles associated with 250–500 lesions1314). Teenagers, adults, and immunocompromised persons commonly suffer more seriously from the disease and are at a higher risk for complications15). In immunocompromised children, progressive, severe varicella is commonly characterized by the continuing eruption of lesions and a high fever, and serious complications such as encephalitis, hepatitis, and pneumonia can also develop131617). In children with cancer, the consequences of untreated varicella are associated with a death rate of 7%18192021). VZV can be spread to immunocompromised patients through direct contact or inhalation of respiratory secretions from a patient with the VZV disease22). The typical incubation period of varicella in children is 14 to 16 days, but ranges from 10 to 21 days after exposure11). The incubation period may last as long as 28 days after administration of VZIG and may be shortened in immunocompromised patients.
Varicella can be avoided by vaccination, however, the varicella vaccine, which contains live attenuated virus, is commonly contraindicated for immunocompromised patients4). The varicella vaccine is recommended as a post-exposure prophylaxis in susceptible immunocompetent children 12 months of age or older1411) and should be administered within 72 to 120 hours after exposure to VZV11). This vaccine can aid in avoiding illness or reducing the severity of varicella11123).
ZIG, VZIG and VariZIG® are all forms of Varicella- Zoster Immune Globulins6). ZIG was originally isolated from patients recovering from herpes zoster in the late 1960s and was commonly administered within 72 hours after exposure to VZV2425). The first commercial VZIG was administered in the US in 1978. VZIG was made from plasma donated from healthy volunteers with high antibody titers to VZV. VZIG was shown to be effective in preventing the varicella disease in susceptible immunocompromised children when administered within 96 hours after exposure to VZV26). In February 2006, the VZIG supply was withdrawn and a new product, VariZIG®, became available for administration within 96 hours of exposure to VZV in the US427). VariZIG®, a purified immune globulin was made from human plasma containing high levels of anti-VZV antibodies that contains 125 U per vial628). In July 2013, the US CDC extended the recommended time for administration of VariZIG® from within 96 hours to up to 10 days after VZV exposure6). In Korea, VZIG that also contains 125 U in a vial is commonly used in the field.
Although the US CDC extended the time for administration of VariZIG®, that recommendation was based on a relatively small number of data from the literature. In Table 3, our results are summarized along with previously reported studies7891029). Overall, our data supports the finding of previous reports as well as the extension of VZIG administration time beyond 96 hours.
Winsnes et al. performed a study analyzing data from ZIG prophylaxis between groups of patients who received ZIG either within 3 days or more than 3 days after exposure to varicella. The occurrence of chickenpox was greatly reduced to 2.9% in patients who received ZIG within 3 days of exposure. Although administration of ZIG more than 3 days after exposure did not reduce the disease rate (43.8%), the course of varicella was attenuated.
In a study by Evans et al., ZIG was administered to 80 VZV seronegative patients between the ages of 3 months and 16 years after varicella exposure. Of the patients who were exposed to varicella at home, 18 out of 27 patients (66.7%) developed chickenpox. Of the patients who were exposed to varicella in hospital, 6 out of 43 patients (14.0%) developed chickenpox. Ten patients did not know where they had been exposed to varicella.Table 3 shows data from 21 home-exposure patients, for whom the ZIG administration time point was available. There was no significant difference in chickenpox development between the two groups (P= 1.0000, Fisher's exact test).
Enders et al. performed a study to analyze the effectiveness of VZIG prophylaxis between seronegative pregnant patients who received VZIG within 3 days and those who received it more than 3 days after exposure to varicella. There was no significant difference in chickenpox development between the two groups (P= 0.8783, Fisher's exact test).
In a study by Koren et al., they examined the effectiveness of VZIG prophylaxis between groups of seronegative pregnant patients who received VZIG within 4 days and those who received it more than 4 days after exposure to varicella. There was no significant difference in chickenpox development between the two groups (P==1.000, Fisher's exact test).
Our study is one of few examinations of this issue that includes a relatively large number of immunocompromised pediatric patients (more than 80% were cancer patients). Although vaccination records or serology test results were not available for the patients in this retrospective study, our observations support the recent updated recommendation from the US CDC.
One of our patients received VZIG 16 days after exposure and did not go on to develop chickenpox. Although she was a transplant recipient, two years have passed from the time of transplant, and her absolute lymphocyte count was 2.728×10 3/µL at the time of exposure and her general immune status was considered as relative competent. Therefore, this duration may not be applicable to other further immunocompromised hosts.
It is important to establish how late Varicella-Zoster Immune Globulins can be given to exposed patients while maintaining its effectiveness. In the previously referenced report, Winsnes et al. did not mention the latest administration date. Evans et al. reported that two study patients developed severe chickenpox; one who had received ZIG 10 days after exposure and the other 15 days after exposure. In a study by Enders et al., the longest period between exposure and VZIG administration was 10 days and in Koren et al.'s study, the longest period before VZIG administration was 14 days post exposure. These two studies did not mention, however, whether these patients developed chickenpox.
Previous studies were performed in seronegative patients who received ZIG or VZIG after varicella exposure including seronegative pregnant women (studies by Enders and Koren). In contrast, our study included mainly immunocompromised children with varicella exposure who were either seronegative, positive, or serostatus unknown. Although our study involves patients with heterogeneous VZV serostatuses, most of the patients were highly immunocompromised (82.5% were cancer patients and 53.8% were HCT recipients). Therefore, we suggest that our data may better represent a real-life situation to aid clinicians in the field, particularly in countries where one dose of VZV vaccination is recommended as a part of national immunization program, as it is in Korea. In our study, ELISA was used for serology test, which may not reveal the true serostatus of the pateints and would be one of the limitations of this study. However, these tests are commonly used as a routine clinical laborytory study and the data from these patients may also represent the real-life situation in clinical practice.
While seventy-four patients received VZIG within 96 hours of exposure to varicella, only 17 received it more than 96 hours. This is the limitation of this study and the number of patients who received VZIG more than 96 hours after exposure is much smaller than that of within 96-hour group. However, even though the data in this study was collected from a retrospective chart review, this study is one of the few reports to analyze chickenpox development in pediatric patients who received VZIG more than 96 hours after exposure to varicella. It would be preferable to give VZIG to high risk patients as soon as possible within 96 hours. However, it appears that the patients who receive VZIG after 96 hours of exposure may also be protected. Therefore, our findings support the previous observations found in the literature and the 2013 US CDC recommendation.
In conclusion, we observed that the effectiveness of VZIG in preventing varicella was comparable between patients who received VZIG within 96 hours and those who received it more than 96 hours after exposure to varicella. A careful and continuous monitoring is required in more patients who receive VZIG at different time points after exposure.
Figures and Tables
References
1. Prevention of varicella. Update recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1999; 48:1–5.
2. Feldman S, Hughes WT, Daniel CB. Varicella in children with cancer: Seventy-seven cases. Pediatrics. 1975; 56:388–397.
3. Levin MJ. Varicella vaccination of immunocompromised children. J Infect Dis. 2008; 197:Suppl 2. S200–S206.

4. Marin M, Guris D, Chaves SS, Schmid S, Seward JF. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007; 56:1–40.
5. Orenstein WA, Heymann DL, Ellis RJ, Rosenberg RL, Nakano J, Halsey NA, et al. Prophylaxis of varicella in high-risk children: dose-response effect of zoster immune globulin. J Pediatr. 1981; 98:368–373.

6. Updated recommendations for use of VariZIG--United States, 2013. MMWR Morb Mortal Wkly Rep. 2013; 62:574–576.
7. Winsnes R. Efficacy of zoster immunoglobulin in prophylaxis of varicella in high-risk patients. Acta Paediatr Scand. 1978; 67:77–82.

8. Evans EB, Pollock TM, Cradock-Watson JE, Ridehalgh MK. Human anti-chickenpox immunoglobulin in the prevention of chickenpox. Lancet. 1980; 1:354–356.

9. Enders G, Miller E. Varicella-zoster virus: virology and clinical management. Varicella and herpes zoster in pregnancy and the newborn. Cambridge, UK: Cambridge University Press;2000.
10. Koren G, Money D, Boucher M, Aoki F, Petric M, Innocencion G, et al. Serum concentrations, efficacy, and safety of a new, intravenously administered varicella zoster immune globulin in pregnant women. J Clin Pharmacol. 2002; 42:267–274.

11. Pickering LK, Baker CJ, Kimberlin DW, Long SS. Red book. 2012. p. 92p. 774–781.
12. Cameron JC, Allan G, Johnston F, Finn A, Heath PT, Booy R. Severe complications of chickenpox in hospitalised children in the UK and Ireland. Arch Dis Child. 2007; 92:1062–1066.

13. Balfour HH Jr. Varicella zoster virus infections in immunocompromised hosts. A review of the natural history and management. Am J Med. 1988; 85:68–73.
14. Swingler G. Chickenpox. Clin Evid. 2003. p. 755–762.
15. Prevention of varicella. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Centers for Disease Control and Prevention. MMWR Recomm Rep. 1996; 45:1–36.
17. Roderick M, Finn A, Ramanan AV. Chickenpox in the immunocompromised child. Arch Dis Child. 2012; 97:587–589.

18. Feldman S, Lott L. Varicella in children with cancer: impact of antiviral therapy and prophylaxis. Pediatrics. 1987; 80:465–472.

19. Brandt L, Broadbent V. A survey of recommendations given to patients going home after bone marrow transplant. Arch Dis Child. 1994; 71:529–531.

20. Weinstock DM, Boeckh M, Sepkowitz KA. Postexposure prophylaxis against varicella zoster virus infection among hematopoietic stem cell transplant recipients. Biol Blood Marrow Transplant. 2006; 12:1096–1097.

21. Bate J, Chisholm J, Heath PT, Breuer J, Skinner R, Manley S, et al. PEPtalk: postexposure prophylaxis against varicella in children with cancer. Arch Dis Child. 2011; 96:841–845.

22. Weinstock DM, Boeckh M, Boulad F, Eagan JA, Fraser VJ, Henderson DK, et al. Postexposure prophylaxis against varicella-zoster virus infection among recipients of hematopoietic stem cell transplant: unresolved issues. Infect Control Hosp Epidemiol. 2004; 25:603–608.

23. Salzman MB, Garcia C. Postexposure varicella vaccination in siblings of children with active varicella. Pediatr Infect Dis J. 1998; 17:256–257.

24. Brunell PA, Ross A, Miller LH, Kuo B. Prevention of varicella by zoster immune globulin. N Engl J Med. 1969; 280:1191–1194.

25. Brunell PA, Gershon AA, Hughes WT, Riley HD, Jr . , Smith J. Prevention of varicella in high risk children: a collaborative study. Pediatrics. 1972; 50:718–722.
26. Zaia JA, Levin MJ, Preblud SR, Leszczynski J, Wright GG, Ellis RJ, et al. Evaluation of varicella-zoster immune globulin: protection of immunosuppressed children after household exposure to varicella. J Infect Dis. 1983; 147:737–743.

27. A new product (VariZIG) for postexposure prophylaxis of varicella available under an investigational new drug application expanded access protocol. MMWR Morb Mortal Wkly Rep. 2006; 55:209–210.
28. FDA approval of an extended period for administering VariZIG for postexposure prophylaxis of varicella. MMWR Morb Mortal Wkly Rep. 2012; 61:212.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download