Abstract
Purpose
Methods
Results
Figures and Tables
Table 1
The Characteristics of Pediatric Patients with Infective Endocarditis and Congenital Heart Disease

Abbreviations: OHS, open heart surgery; MPA, main pulmonary artery; ASD, atrial septal defect; MV, mitral valve; CNS, coagulase negative staphylococcus; TR, tricuspid regurgitation; TV, tricuspid valve; PDA, patent ductus arteriosus; S. viridans, Streptococcus viridans; RA, right atrium; MR, mitral regurgitation; TGA, transposition of great artery; VSD, ventricular septal defect; TOF, tetralogy of Fallot; PVR, pulmonary valve replacement; PV, pulmonary valve; TAP, transannular patch; RVOT, right ventricular outflow tract; MRSA, methicillin resistant Staphylococcus aureus; MSSA, methicillin sensitive Staphylococcus aureus; PS, pulmonary stenosis; AV, aortic valve; AS, aortic stenosis.
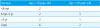
Table 2
The History of Congenital Heart Disease and Types of Open Heart Surgery in Each Patient with Infective Endocarditis

Table 3
The Characteristics of Adult Patients with Infective Endocarditis and Congenital Heart Disease

*Case 1 and 2 occurred 1 year apart in one patient.
†Two blood cultures were positive in case 1 and 3.
‡Only one blood culture was positive in case 2.
Abbreviations: OHS, open heart surgery; AV, aortic valve; AS, aortic stenosis; MRSA, methicillin resistant Staphylococcus aureus; AVR, aortic valve replacement; L. garvieae, Lactococcus garvieae; PDA, patent ductus arteriosus; PA, pulmonary artery; S. viridans, Streptococcus viridans; TOF, tetralogy of Fallot; PS, pulmonary stenosis; PR, pulmonary regurgitation; VSD, ventricular septal defect; MSSA, methicillin sensitive Staphylococcus aureus; CNS, coagulase negative Staphylococcus; MV, mitral valve; PV, pulmonary valve.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download