Abstract
Paragonimiasis was one of the most common causes of cavitary lung lesions until the 1960s, but now it has become a very rare disease in Korea. A 16-year-old boy presented with hemoptysis and several days of cough. His plain chest radiograph showed nodular opacity with a cavity in the left upper lung region. Although his symptoms disappeared after taking antituberculous drugs, his plain chest radiograph and computed tomography images after completion of therapy showed a new nodule with a cavity in the left lung field. Through video-assisted thoracoscopic wedge resection, Paragonimus eggs were found in the lung tissues.
Figures and Tables
 | Figure 1(A) Initial chest radiograph shows a subpleural nodule (arrow) in the left upper lung field with localized pleural thickening (arrowhead). Note subtle bubble-like air density within the nodule. (B) Follow-up chest radiograph after completion of antituberculosis medication reveals enlargement of the nodule with increased cavitary portion (arrow) accompanied with pulmonic infiltrates (arrowheads). |
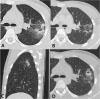 | Figure 2Serial follow-up of computed tomography (CT). (A) Initial CT scan image shows subpleural air space consolidation and nodule (arrow) with peripheral ground-glass attenuation and tubular shape cavity in the left upper lobe. (B) Follow-up CT scan during antituberculosis medication shows clusters of tiny centrilobular nodules (arrowheads) whereas surrounding ground-glass opacities are resolved. (C) Sagittal image reveals subpleural linear air space consolidation with internal cavitation and surrounding halo of ground-glass attenuation. Note the indentation of the pleura (curved arrow). (D) CT image obtained after completion of antituberculosis medication shows newly appeared nodule with central cavitation (arrow) and increased extent of surrounding ground-glass attenuation (arrowheads). |
References
2. Yun DJ. Paragonimiasis in children in Korea, related to the custom of ingesting raw crayfish for the treatment of measles. J Pediatr. 1960; 56:736–751.
3. Lee S, Yu Y, An J, Lee J, Son JS, Lee YK, et al. A case of delayed diagnosis of pulmonary paragonimiasis due to improvement after anti-tuberculosis therapy. Tuberc Respir Dis (Seoul). 2014; 77:178–183.

4. Lee JJ, Choi CM, Kwon HH, Kim MS, Kim JS, Park SY, et al. A case of pulmonary paragonimiasis mimicking lung cancer diagnosed by EBUS-TBNA. Korean J Med. 2013; 84:423–427.

5. Kim KU, Lee K, Park HK, Jeong YJ, Yu HS, Lee MK. A pulmonary paragonimiasis case mimicking metastatic pulmonary tumor. Korean J Parasitol. 2011; 49:69–72.

7. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download