Abstract
Methods
We retrospectively analyzed the medical records of pediatric patients admitted to the Department of Pediatrics at the Jeonju Presbyterian Medical Center from January 2007 to August 2016. We classified patients who were readmitted with pneumonia within 30 days of discharge as the readmission group and patients who were admitted with pneumonia for the first time as the first admission group.
Results
Among 158 patients, the study (readmission) group included 82 patients and the control (first admission) group included 76 patients. Age, the percentage of segmented neutrophils and lymphocytes, the number of admissions in the last 12 months, the associated diseases (respiratory diseases such as asthma), and the affection of the right upper lung were analyzed as risk factors for readmission. However, based on a regression analysis, only age and associated diseases were found to be significant risk factors. The rate of readmission increased with younger age. When there were associated diseases, the rate of readmission also increased.
Conclusions
Young age and associated diseases were significant risk factors for readmission for patients with pediatric pneumonia. When pediatric patients are admitted with pneumonia, if they are young and/or have associated diseases, a comprehensive approach is needed to reduce the rate of readmission with careful consideration of precise examination, treatment, timing of discharge, and follow-up.
Figures and Tables
Table 3
Logistic Regression of Risk Factors Independently Related to Readmission
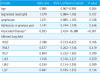
*Respiratory disease, gastrointestinal disease, congenital heart disease, down syndrome, congenital hypothyroidism, and other diseases.
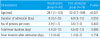
Abbreviations: RULF, right upper lung field; RMLF, right middle lung field; RLLF, righr lower lung filed; LULF, left upper lung field; LMLF, left middle lung field; LLLF, left lower lung filed.
References
1. Bardach NS, Vittinghoff E, Asteria-Penaloza R, Edwards JD, Yazdany J, Lee HC, et al. Measuring hospital quality using pediatric readmission and revisit rates. Pediatrics. 2013; 132:429–436.

2. Berry JG, Hall DE, Kuo DZ, Cohen E, Agrawal R, Feudtner C, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011; 305:682–690.

3. Berry JG, Toomey SL, Zaslavsky AM, Jha AK, Nakamura MM, Klein DJ, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013; 309:372–380.

4. Wever-Hess J, Hermans J, Kouwenberg JM, Duiverman EJ, Wever AM. Hospital admissions and readmissions for asthma in the age group 0-4 years. Pediatr Pulmonol. 2001; 31:30–36.

5. Brogan TV, Hall M, Sills MR, Fieldston ES, Simon HK, Mundorff MB, et al. Hospital readmissions among children with H1N1 influenza infection. Hosp Pediatr. 2014; 4:348–358.

6. Neuman MI, Hall M, Gay JC, Blaschke AJ, Williams DJ, Parikh K, et al. Readmissions among children previously hospitalized with pneumonia. Pediatrics. 2014; 134:100–109.

7. Jasti H, Mortensen EM, Obrosky DS, Kapoor WN, Fine MJ. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis. 2008; 46:550–556.

8. Hong CE. Respiratory diseases. In : Ahn HS, Shin HY, editors. Textbook of pediatrics. 11th ed. Seoul: Miraen;2016. p. 626–713.
9. Schnabel E, Sausenthaler S, Brockow I, Liese J, Herbarth O, Michael B, et al. Burden of otitis media and pneumonia in children up to 6 years of age: results of the LISA birth cohort. Eur J Pediatr. 2009; 168:1251–1257.

11. Kim SA, Kilgore PE, Lee SY, Nyambat B, Ki M. Trends in pneumonia and influenza-associated hospitalizations in South Korea, 2002-2005. J Health Popul Nutr. 2011; 29:574–582.

12. Winterbauer RH, Bedon GA, Ball WC Jr. Recurrent pneumonia. Predisposing illness and clinical patterns in 158 patients. Ann Intern Med. 1969; 70:689–700.
13. Allaudeen N, Vidyarthi A, Maselli J, Auerbach A. Redefining readmission risk factors for general medicine patients. J Hosp Med. 2011; 6:54–60.

14. Yoon KL, Rah YH, Bae CW, Chung SJ. Analysis of risk factors of readmission to hospital for pediatric asthma. J Korean Pediatr Soc. 2000; 43:556–560.
15. Kim MJ. Readmission of late preterm infants after discharge from nursery. Korean J Pediatr. 2009; 52:888–892.

16. Kim MH, Kim HS, Park JD. Factors influencing readmission of home ventilator-assisted children. J Korean Acad Child Health Nurs. 2012; 18:9–18.

17. Jadavji T, Law B, Lebel MH, Kennedy WA, Gold R, Wang EE. A practical guide for the diagnosis and treatment of pediatric pneumonia. CMAJ. 1997; 156:S703–S711.
18. Denny FW, Clyde WA Jr. Acute lower respiratory tract infections in nonhospitalized children. J Pediatr. 1986; 108(5 Pt 1):635–646.

19. Eom KS, Jeon G, Shin TR, Jang SH, Bahn JW, Lee JY, et al. Clinical investigation of recurrent pneumonia in adults: analysis of patients from Hallym University Medical Center. Tuberc Respir Dis. 2004; 57:47–54.

20. Owayed AF, Campbell DM, Wang EE. Underlying causes of recurrent pneumonia in children. Arch Pediatr Adolesc Med. 2000; 154:190–194.

21. Ozdemir O, Sari S, Bakirtas A, Zorlu P, Ertan U. Underlying diseases of recurrent pneumonia in Turkish children. Turk J Med Sci. 2010; 40:25–30.
22. Shin HJ, Lee HH, Park KH, Jeong BJ, Kim KE, Lee KY. Predisposing factors of recurrent pneumonia in children. Pediatr Allergy Respir Dis. 1997; 7:274–281.
23. Elemraid MA, Rushton SP, Thomas MF, Spencer DA, Gennery AR, Clark JE. Utility of inflammatory markers in predicting the aetiology of pneumonia in children. Diagn Microbiol Infect Dis. 2014; 79:458–462.

24. Li JS, Hou ZK, Yu XQ, Li SY, Sun ZK, Zhang W, et al. Prognostic factors for community-acquired pneumonia in middle-aged and elderly patients treated with integrated medicine. J Tradit Chin Med. 2012; 32:179–186.

25. Moret I, Lorenzo MJ, Sarria B, Cases E, Morcillo E, Perpina M, et al. Increased lung neutrophil apoptosis and inflammation resolution in nonresponding pneumonia. Eur Respir J. 2011; 38:1158–1164.

26. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003; 31:1250–1256.

27. Kin Key N, Araujo-Neto CA, Nascimento-Carvalho CM. Severity of childhood community-acquired pneumonia and chest radiographic findings. Pediatr Pulmonol. 2009; 44:249–252.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download