Abstract
An 18-year-old male visited our department complaining of recurrent episodes of an itchy rash after hand washing, showering/bathing, drinking water, and getting rain-soaked. He was diagnosed with aquagenic urticaria after a water provocation test and histopathologic examination. Five months of antihistamine treatment successfully prevented further wheal formation. Aquagenic urticaria is a very unusual form of physical urticaria caused by contact with water. It manifests as pruritic small wheals surrounded by erythema within 30 minutes of exposure. The condition can be diagnosed by a water provocation test. Systemic antihistamines are the first-line treatment, with anticholinergics, phototherapy, or barrier cream used alternatively or additionally. Four cases of aquagenic urticaria have been reported in Korea, but no histopathologic evaluation was reported in the English or Korean literature. Herein, we provide both a case report of aquagenic urticaria diagnosed by the water provocation test and histopathologic examination results for this patient.
Aquagenic urticaria, first described in 1964 by Shelly and Rawnsley1, is a rare variant of physical urticaria induced by direct contact with water, regardless of its temperature or source2. It is characterized by small punctate wheals on the area of skin in contact with the water2. Here we report a case of aquagenic urticaria during adolescence and review the clinical manifestations, pathogenesis, diagnosis, and current treatment modalities.
An 18-year-old male, with no previous medication, presented with a 1-week-history of recurrent erythema and small punctate wheals with pruritus. The lesions occurred 5~10 minutes after water exposure, including hand washing, dishwashing, getting rain-soaked, and showering/bathing, regardless of the water temperature or source, and were limited to the area of skin in contact with the water including face, neck, trunk, and both extremities. He also complained of pruritic erythematous changes, with swelling of the lips and oral cavity, after drinking water. Each episode lasted from 30 to 60 minutes and resolved spontaneously. He had no systemic reactions, such as headache or lightheadedness. Neither exercise nor cold exposure induced wheal formation. He had no personal history of allergies or atopic diseases nor a family history of similar reactions or lesions.
On physical examination, he demonstrated erythematous changes with pruritus on both hands after hand washing. A water provocation test was performed on his right arm using a towel soaked in tap water at body temperature. He complained of pruritus after 5 minutes, and multiple small wheals with surrounding erythema were observed on the water-exposed area (Fig. 1). Stroking of the skin did not induce a wheal or flare reaction.
Laboratory tests revealed mild leukocytosis (11,030/mm3), increased eosinophil cationic protein (48.2 µg/L), and increased total IgE (773 KU/L).
Histopathologic examination revealed conspicuous interstitial edema, a sparse perivascular and interstitial inflammatory infiltration composed of lymphocytes, mast cells, and a few neutrophils, and endothelial swelling (Fig. 2). An increase in the number of mast cells around the blood vessels was demonstrated by immunohistochemical analysis of c-kit (Fig. 3).
The patient was diagnosed with aquagenic urticaria and responded well to 20 mg bepotastine. He then received a prescription for 10 mg bepotastine once a day. At the 5-month follow-up, he did not report any further episodes of urticaria.
Aquagenic urticaria is a rare variant of physical urticaria2. It occurs predominantly in females, especially with the onset of puberty. Most cases are sporadic, but several familial cases have been reported2. Symptoms develop within 30 minutes after contact with water regardless of its temperature or source. The pruritic small wheals surrounded by erythema usually last less than 1 hour. Some patients report additional, systemic symptoms such as headache, lightheadedness, respiratory distress, and palpitations, but these are usually rare2.
The pathogenesis is still unclear, but the interaction of water with unknown components in the epidermis or dermis might cause histamine release from sensitized dermal mast cells, which in turn leads to wheal formation134.
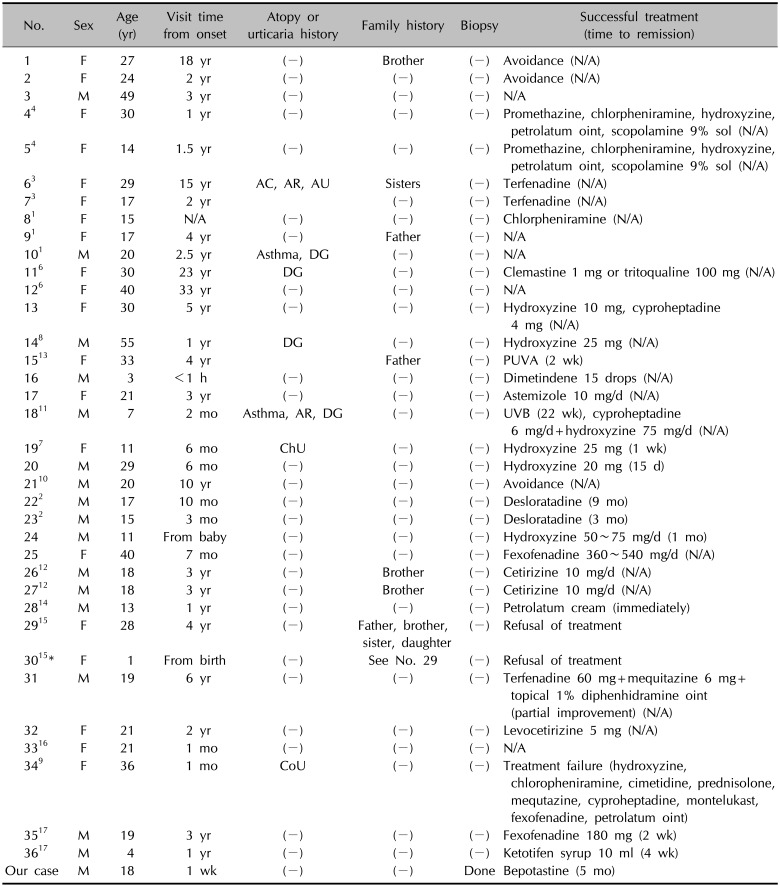
In addition to the patient's history, the diagnosis relies on the results of the water provocation test. Magerl et al.5 (2009) recommended applying a wet cloth at body temperature onto an area of the skin for 20 minutes. Because aquagenic urticaria may be associated with other types of physical urticaria, such as dermographism, cholinergic urticaria, and cold urticaria167891011, these condition should be excluded, especially cholinergic urticaria, in which the wheals are similar morphologically2. Previously reported cases of aquagenic urticaria are described in Table 11234567891011121314151617.
This patient was diagnosed with aquagenic urticaria based on his history, the results of a water provocation test, and a histopathologic examination, which showed interstitial dermal edema, endothelial swelling, and sparse infiltration of inflammatory cells, including mast cells around blood vessels.
Many of these histopathologic findings are the same as those of acute urticaria, in which interstitial dermal edema, dilated venules, endothelial swelling, and sparse infiltration of inflammatory cells have been described18. Mast cells are concentrated around the blood vessels of normal dermis, with one to three cells per cross-sectional vessel profile19, but in this patient there were slightly increased numbers of mast cells around blood vessels.
Antihistamines are the first line treatment for aquagenic urticaria12. In recalcitrant cases, the dose can be increased by as much as four-fold the conventional dose12. Phototherapy and barrier cream are alternative or additional treatments if antihistamines fail to prevent recurrence13. The efficacy of phototherapy is related to its induction of both immunosuppression, including a decreased mast cell response, and epidermal thickening, which disturbs the penetration of water and thus also inhibits mast cell stimulation1020. Barrier cream prevents the penetration of water into the dermis. However, the various emollients and water-resistant creams investigated have not yielded conspicuous success14, except in a few cases in which a petrolatum-containing ointment was applied before water exposure414. Anticholinergics such as scopolamine may also offer relief15. Most of the patients were successfully controlled with antihistamines, although some of them changed treatment modalities because of drowsiness.
References
1. Shelly WB, Rawnsley HM. Aquagenic urticaria. Contact sensitivity reaction to water. JAMA. 1964; 189:895–898. PMID: 14172902.
2. Yavuz ST, Sahiner UM, Tuncer A, Sackesen C. Aquagenic urticaria in 2 adolescents. J Investig Allergol Clin Immunol. 2010; 20:624–625.
3. Czarnetzki BM, Breetholt KH, Traupe H. Evidence that water acts as a carrier for an epidermal antigen in aquagenic urticaria. J Am Acad Dermatol. 1986; 15:623–627. PMID: 2429997.

4. Sibbald RG, Black AK, Eady RA, James M, Greaves MW. Aquagenic urticaria: evidence of cholinergic and histaminergic basis. Br J Dermatol. 1981; 105:297–302. PMID: 7272209.

5. Magerl M, Borzova E, Giménez-Arnau A, Grattan CE, Lawlor F, Mathelier-Fusade P, et al. The definition and diagnostic testing of physical and cholinergic urticarias--EAACI/GA2LEN/EDF/UNEV consensus panel recommendations. Allergy. 2009; 64:1715–1721. PMID: 19793059.
6. Bonnetblanc JM, Andrieu-Pfahl F, Meraud JP, Roux J. Familial aquagenic urticaria. Dermatologica. 1979; 158:468–470. PMID: 38152.

7. Davis RS, Remigio LK, Schocket AL, Bock SA. Evaluation of a patient with both aquagenic and cholinergic urticaria. J Allergy Clin Immunol. 1981; 68:479–483. PMID: 7310013.

8. Gimenez-Arnau A, Serra-Baldrich E, Camarasa JG. Chronic aquagenic urticaria. Acta Derm Venereol. 1992; 72:389. PMID: 1361294.
9. Kim CH, Ryu ST, Park SW, Lee JH, Oh WS, Chang SI, et al. A case of the coexistence of cold urticaria and aquagenic urticaria. Korean J Asthma Allergy Clin Immunol. 2004; 24:350–352.
10. Luong KV, Nguyen LT. Aquagenic urticaria: report of a case and review of the literature. Ann Allergy Asthma Immunol. 1998; 80:483–485. PMID: 9647271.

11. Parker RK, Crowe MJ, Guin JD. Aquagenic urticaria. Cutis. 1992; 50:283–284. PMID: 1424795.
12. Kai AC, Flohr C. Aquagenic urticaria in twins. World Allergy Organ J. 2013; 6:2. PMID: 23663417.

13. Juhlin L, Malmros-Enander I. Familial polymorphous light eruption with aquagenic urticaria: successful treatment with PUVA. Photodermatol. 1986; 3:346–349. PMID: 3588355.
14. McGee JS, Kirkorian AY, Pappert AS, Milgraum SS. An adolescent boy with urticaria to water: review of current treatments for aquagenic urticaria. Pediatr Dermatol. 2014; 31:116–117. PMID: 22994854.

15. Seize MB, Ianhez M, de Souza PK, Rotta O, Cestari Sda C. Familial aquagenic urticaria: report of two cases and literature review. An Bras Dermatol. 2009; 84:530–533. PMID: 20098859.
16. Lee HG, Lee AY, Lee YS. A case of aquagenic urticaria. Korean J Dermatol. 1990; 28:456–458.
17. Park H, Kim HS, Yoo DS, Kim JW, Kim CW, Kim SS, et al. Aquagenic urticaria: a report of two cases. Ann Dermatol. 2011; 23(Suppl 3):S371–S374. PMID: 22346281.

18. Mobini N, Toussaint S, Kamino H. Noninfectious erythematous, papular, and squamous diseases. In : Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2008. p. 169–203.
19. Velazquez EF, Murphy GF. Introduction to dermatopathologic diagnosis. In : Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2008. p. 7–66.
20. Gollhausen R, Kaidbey K, Schechter N. UV suppression of mast cell-mediated wealing in human skin. Photodermatol. 1985; 2:58–67. PMID: 4041035.
Fig. 1
Multiple small wheals with surrounding erythema were seen on the right forearm after applying a towel soaked in tap water at body temperature for 5 minutes.

Fig. 2
(A) Histopathologic examination revealed conspicuous interstitial dermal edema and sparse perivascular and interstitial inflammatory cell infiltration (H&E, ×40). (B) A high-powered view showed perivascular infiltrate of lymphocytes and mast cells with endothelial swelling (H&E, ×400).
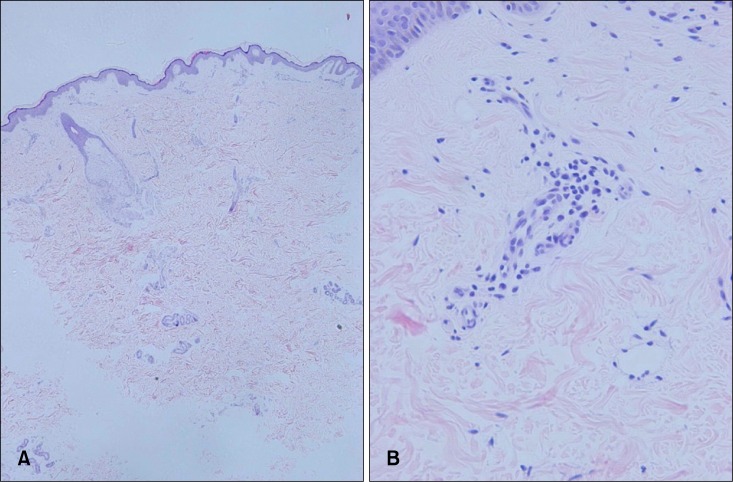
Fig. 3
Immunohistochemistry for c-kit showed slightly increased number of mast cells around blood vessels (×200).
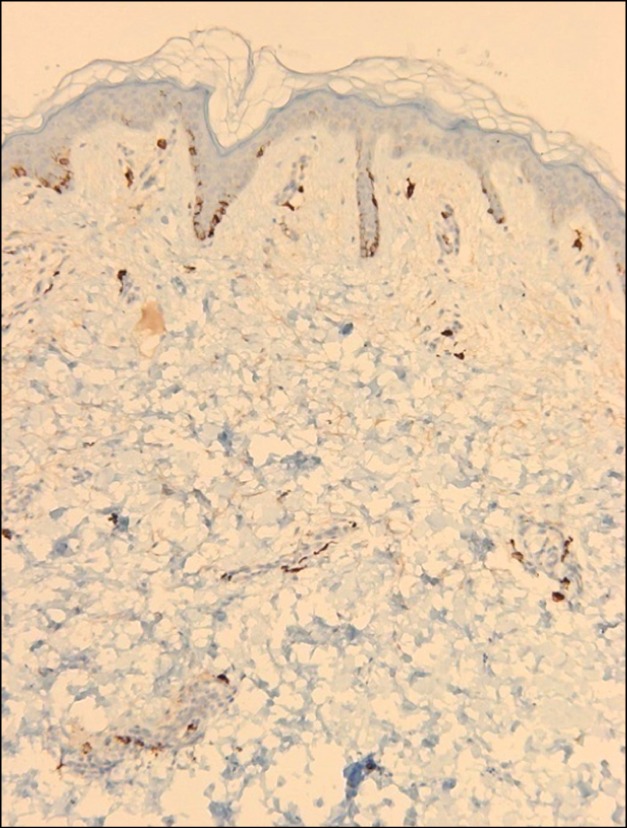
Table 1
Reported cases of aquagenic urticaria in the literature
| No. | Sex | Age (yr) | Visit time from onset | Atopy or urticaria history | Family history | Biopsy | Successful treatment (time to remission) |
|---|---|---|---|---|---|---|---|
| 1 | F | 27 | 18 yr | (−) | Brother | (−) | Avoidance (N/A) |
| 2 | F | 24 | 2 yr | (−) | (−) | (−) | Avoidance (N/A) |
| 3 | M | 49 | 3 yr | (−) | (−) | (−) | N/A |
| 44 | F | 30 | 1 yr | (−) | (−) | (−) | Promethazine, chlorpheniramine, hydroxyzine, petrolatum oint, scopolamine 9% sol (N/A) |
| 54 | F | 14 | 1.5 yr | (−) | (−) | (−) | Promethazine, chlorpheniramine, hydroxyzine, petrolatum oint, scopolamine 9% sol (N/A) |
| 63 | F | 29 | 15 yr | AC, AR, AU | Sisters | (−) | Terfenadine (N/A) |
| 73 | F | 17 | 2 yr | (−) | (−) | Terfenadine (N/A) | |
| 81 | F | 15 | N/A | (−) | (−) | (−) | Chlorpheniramine (N/A) |
| 91 | F | 17 | 4 yr | (−) | Father | (−) | N/A |
| 101 | M | 20 | 2.5 yr | Asthma, DG | (−) | (−) | N/A |
| 116 | F | 30 | 23 yr | DG | (−) | (−) | Clemastine 1 mg or tritoqualine 100 mg (N/A) |
| 126 | F | 40 | 33 yr | (−) | (−) | (−) | N/A |
| 13 | F | 30 | 5 yr | (−) | (−) | (−) | Hydroxyzine 10 mg, cyproheptadine 4 mg (N/A) |
| 148 | M | 55 | 1 yr | DG | (−) | (−) | Hydroxyzine 25 mg (N/A) |
| 1513 | F | 33 | 4 yr | Father | (−) | PUVA (2 wk) | |
| 16 | M | 3 | <1 h | (−) | (−) | (−) | Dimetindene 15 drops (N/A) |
| 17 | F | 21 | 3 yr | (−) | (−) | (−) | Astemizole 10 mg/d (N/A) |
| 1811 | M | 7 | 2 mo | Asthma, AR, DG | (−) | (−) | UVB (22 wk), cyproheptadine 6 mg/d+hydroxyzine 75 mg/d (N/A) |
| 197 | F | 11 | 6 mo | ChU | (−) | (−) | Hydroxyzine 25 mg (1 wk) |
| 20 | M | 29 | 6 mo | (−) | (−) | (−) | Hydroxyzine 20 mg (15 d) |
| 2110 | M | 20 | 10 yr | (−) | (−) | (−) | Avoidance (N/A) |
| 222 | M | 17 | 10 mo | (−) | (−) | (−) | Desloratadine (9 mo) |
| 232 | M | 15 | 3 mo | (−) | (−) | (−) | Desloratadine (3 mo) |
| 24 | M | 11 | From baby | (−) | (−) | (−) | Hydroxyzine 50~75 mg/d (1 mo) |
| 25 | F | 40 | 7 mo | (−) | (−) | (−) | Fexofenadine 360~540 mg/d (N/A) |
| 2612 | M | 18 | 3 yr | (−) | Brother | (−) | Cetirizine 10 mg/d (N/A) |
| 2712 | M | 18 | 3 yr | (−) | Brother | (−) | Cetirizine 10 mg/d (N/A) |
| 2814 | M | 13 | 1 yr | (−) | (−) | (−) | Petrolatum cream (immediately) |
| 2915 | F | 28 | 4 yr | (−) | Father, brother, sister, daughter | (−) | Refusal of treatment |
| 3015* | F | 1 | From birth | (−) | See No. 29 | (−) | Refusal of treatment |
| 31 | M | 19 | 6 yr | (−) | (−) | (−) | Terfenadine 60 mg+mequitazine 6 mg+topical 1% diphenhidramine oint(partial improvement) (N/A) |
| 32 | F | 21 | 2 yr | (−) | (−) | (−) | Levocetirizine 5 mg (N/A) |
| 3316 | F | 21 | 1 mo | (−) | (−) | (−) | N/A |
| 349 | F | 36 | 1 mo | CoU | (−) | (−) | Treatment failure (hydroxyzine, chloropheniramine, cimetidine, prednisolone, mequtazine, cyproheptadine, montelukast, fexofenadine, petrolatum oint) |
| 3517 | M | 19 | 3 yr | (−) | (−) | (−) | Fexofenadine 180 mg (2 wk) |
| 3617 | M | 4 | 1 yr | (−) | (−) | (−) | Ketotifen syrup 10 ml (4 wk) |
| Our case | M | 18 | 1 wk | (−) | (−) | Done | Bepotastine (5 mo) |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download