Abstract
Discoid lupus erythematosus (DLE) is a chronic form of cutaneous lupus that can cause permanent scarring. Treatment of DLE includes protection from sunlight and artificial sources of ultraviolet light, as well as systemic and topical medications. The first-line standard therapies are antimalarials and topical steroids. Other systemic therapies include systemic steroid, azathioprine, dapsone, and immunosuppressive agents. Topical tacrolimus and pimecrolimus have also been evaluated. Recent studies reported that several treatments, including pulsed dye laser, CO2 laser, intense pulsed light (IPL), and 1,064-nm long-pulse neodymium-doped yttrium aluminum (Nd:YAG) have been used for the cosmetic treatment of DLE. Here, we report a case of a DLE scar that was successfully treated with a combination therapy of IPL and Q-switched 1,064-nm Nd:YAG laser.
Discoid lupus erythematosus (DLE) is a chronic form of cutaneous lupus that can cause permanent scarring. Treatment of DLE includes protection from sunlight and artificial sources of ultraviolet (UV) light, as well as systemic and topical medications1. The first-line standard therapies are antimalarials and topical steroids12. Other systemic therapies include systemic steroid, azathioprine, dapsone, and immunosuppressive agents1. Topical tacrolimus and pimecrolimus have also been evaluated3. Recent studies reported that several treatments, including pulsed dye laser, CO2 laser, intense pulsed light (IPL), and 1,064-nm long-pulse neodymium-doped yttrium aluminum (Nd:YAG) have been used for the cosmetic treatment of DLE456. Here, we report a case of a DLE scar that was successfully treated with a combination therapy of IPL and Q-switched 1,064-nm Nd:YAG laser.
A 42-year-old female patient with a 20-year history of DLE scarring, presented sharply demarcated erythematous and hyperpigmented, indurated plaques and atrophic scars on the cheek and back. She had been treated with systemic corticosteroid and hydroxychloroquine for systemic lupus erythematosus, for 20 years. Laboratory findings were normal except for a high antinuclear antibody titer of 1:320 with a homogenous pattern. A lesional skin biopsy was consistent with lupus erythematosus (Fig. 1). She suffered from disfiguring DLE scars on her face, which were refractory to systemic medicine and topical steroid. She expressed a desire to receive other forms of interventions, so we decided to try IPL (Ellipse Flex; Danish Dermatologic Development, Hoersholm, Denmark). IPL resolved the erythematous lesions but not the hyperpigmentation (Fig. 2). These hyperpigmented lesions were improved after Q-switched 1,064-nm Nd:YAG laser (Iris; Bluecore Company, Seoul, Korea) treatment. The treatment parameters of IPL were 555~950 nm, 11~12 J/cm2, 8 ms. The treatment parameters of Q-switched Nd:YAG laser were 1,064 nm, 3-mm spot size, fluences 6~6.5 J/cm2, 10 Hz. For improvement of the erythematous and hyperpigmented mixed lesion, we decided to try combination of IPL and Q-switched 1,064-nm Nd:YAG laser. After the third session of treatment (3~5-week intervals), the skin lesion showed marked improvement (Fig. 3). During the treatment, she had mild erythema and oozing but no serious side effects. Improvement was maintained for one year of follow up without relapse.
IPL is effective in clearing the epidermal pigmentary and vascular tissue, but not satisfactory for mixed or dermal lesions. Treatment using the Q-switched 1,064-nm Nd:YAG laser can selectively target dermal melanosomes without producing inflammation or epidermal damage.
Previous studies reported that several treatments have been successful for the scarring lesions of DLE456. However, we found that IPL treatment could not resolve the hyperpigmented lesions and Q-switched 1,064-nm Nd:YAG laser could not resolve the erythematous lesions. It was postulated that the combination of IPL and Q-switched 1,064-nm Nd:YAG laser could be successful for treatment of DLE scarring lesions, because a DLE lesion is composed of telangiectasia and dermal hyperpigmentation. IPL emits visible light, and discoid lupus lesions have photosensitivity. This is usually related to UV light radiation but visible light also has effect at high fluencies. Therefore IPL could cause exacerbation of the lesions. Treatment with IPL should be made in caution, because skin lesion in DLE might be aggravated by visible light, which wavelength is same with IPL. For safety, we tried low fluences 11~12 J/cm2 of IPL. The lesion was not worsened by either the low-fluence IPL or Q-switched 1,064-nm Nd:YAG laser during and after the treatment periods.
This is the first case report of the use of combined IPL and Q-switched 1,064-nm Nd:YAG laser, as a cosmetic treatment for scarring lesions of DLE. It seems that this combination therapy is safe and highly effective when performed with careful caution.
Figures and Tables
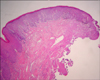 | Fig. 1The epidermis shows vacuolar basal cell degeneration, and the perivascular inflammatory cells infiltrate the upper dermis (H&E, ×40). |
ACKNOWLEDGMENT
This research was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2017R1A2B4006252) and HI17C0597 and Hallym University Research Fund 2017 (HURF-2017-35).
References
1. Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: issues in diagnosis and treatment. Am J Clin Dermatol. 2009; 10:365–381.
2. Han YW, Kim HO, Park SH, Park YM. Four cases of facial discoid lupus erythematosus successfully treated with topical pimecrolimus or tacrolimus. Ann Dermatol. 2010; 22:307–311.

3. Tzellos TG, Kouvelas D. Topical tacrolimus and pimecrolimus in the treatment of cutaneous lupus erythematosus: an evidence-based evaluation. Eur J Clin Pharmacol. 2008; 64:337–341.

4. Ekbäck MP, Troilius A. Laser therapy for refractory discoid lupus erythematosus when everything else has failed. J Cosmet Laser Ther. 2013; 15:260–265.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download