Abstract
Background
Delivery of pathology reports to the patient is a key step in the biopsy pathway, which is important for patient safety in dermatology. Automated systems for facilitating such medical process began in 2010 in our hospital, sending short message service to scheduled patients.
Objective
The purpose of this study was to evaluate the delivery of pathology reports to patients and investigate factors that influence this process and annual trends.
Methods
We retrospectively reviewed the medical records of all outpatients (n=2,452) who underwent skin biopsy at our department of dermatology in 2009 and 2014. In each year group, we analyzed the proportion of revisiting patients in terms of year, sex, age, season, biopsy method and diagnosis.
Results
In 2009, a smaller proportion of patients (205; 91.5%) who had undergone shave or excisional biopsy than of those who had undergone punch biopsy returned (781; 98.0%; p<0.001). This trend was not significant in 2014. Whereas there was no significant difference of return visit ratio between men and women in 2009, a higher proportion of women (754; 98.0%) than men (633; 95.6%) re-visited after skin biopsy to confirm their diagnosis in 2014 (p=0.008). Three patients with either a malignant tumor or suspected malignant lesion that required complete excision did not return to our clinic.
Skin biopsy is the most common and critical test in determining the diagnosis and etiology of skin diseases. Biopsy quality involves several aspects (test site, proficiency of the physician, quality and preservation of the sample, and proficiency of the pathologist), and each aspect is important to the quality of the entire test12. However, even if all of the above aspects are satisfactory, the ultimate purpose of the test can only be fulfilled when the pathology test results are delivered to the dermatology staff within an appropriate time period, and when the information is then delivered to the patient. It is the clinician's ethical responsibility to deliver the test results to the patient promptly, especially if the results indicate a malignant tumor or the need for a surgical resection. Because telemedicine is prohibited in South Korea except for specific conditions (prison and backwoods), return visit of patients is essential for delivery of test results. To the best of our knowledge, apart from one study in an Israeli hospital3, few studies have examined the delivery of pathology test results from the perspective of patient safety.
Advances in data-processing equipment have provided medical staff with easier access to patients' test results. In this regard, SMG-SNU Boramae Medical Center began to computerize medical records in 2010; in the same year, it implemented a notification system that automatically sends text messages to patients who are scheduled for revisits. Patients with systemic disease such as systemic lupus erythematosus showed better adherence by cellular text messaging service4. However, the effect of the automated system on patient revisits has not yet been evaluated in Korea.
For this reason, we sought to identify differences in the revisit ratios of patients who underwent skin biopsy at the dermatology clinic of our hospital in terms of their visiting year (2009 or 2014), age, and sex, season, biopsy method, and diagnosis. We also sought to assess the current information delivery system at our hospital, and to propose improvements to the system by identifying the changes of patients' behaviors in the context of skin biopsy.
A single-center, retrospective study was performed searching electronic medical records from January 1st 2009 to December 31st 2009 and from January 2014 1st to December 31st 2014 at the Department of Dermatology, SMG-SNU Boramae Medical Center, which is a secondary referral center in Seoul. Patients who visited our outpatient clinics and underwent skin biopsy were included. This study was approved by the internal Institutional Review Board (IRB no. 16-2015-116).
Patient data including sex, test dates, age at test, punch biopsy or shave/excisional biopsy according to order code were gathered retrospectively from the electronic medical records. If a patient received biopsy for multiple sites on the same day, we regarded it as one patient. When a patient underwent multiple skin biopsy procedures on different dates, we counted separately. Patients were considered to revisit when they visit our clinic within 1 month after skin biopsy. Diagnosis for benign or malignant lesion was determined by one dermatologic specialist and one resident of the department of dermatology, based on pathologic reports by pathologist in our hospital. One case with malignancy suspected lesion which required complete excision was classified as malignant. Biopsy dates were recorded daily, and divided into four seasons by 3 month-interval from March in order.
Data were analyzed by software (IBM SPSS Statistics ver. 20.0 for Windows; IBM Co., Armonk, NY, USA). The chi-square test was performed to analyze revisiting after skin biopsy with different sex, biopsy method, pathologic report, and biopsy date, respectively. Student's t-test was performed to evaluate age difference between patients who revisited and who did not. Breslow-Day test for homogeneity of odds ratio was used to evaluate whether changes in the degree of difference are heterogeneous enough between revisit trend in 2009 and 2014. A p<0.05 was considered statistically significant.
Total 2,452 patients were included in the study and their demographic data was summarized in Table 1. Numbers of biopsy procedures were 1.4 times increased from 1,021 patients in 2009 to 1,431 patients in 2014. Sex ratio was almost 1 in 2009, but female proportion was slightly increased in 2014. Average age (mean±standard deviation) were 45.8±20.5 years in 2009 and 49.2±21.0 years in 2014. There was slight increase in patient visits and biopsies in summer compared to other seasons, but there was no significant difference between them in 2009 and 2014. Patients received punch biopsy approximately 4 times more often than shave or excisional biopsy in 2009 and 2014. As for the pathology test results in 2009, benign lesions were 981 cases (96.1%) and malignant or excision-required lesions were 40 cases (3.9%); in 2014, 1,356 cases (94.8%) with benign and 75 cases (5.2%) with malignant and proportion of malignant disease was slightly increased.
Patients who returned to clinics after skin biopsy were 986 of 1,021 patients (96.6%) in 2009 and 1,387 of 1,431 patients (96.9%) in 2014. There was no statistically significant difference across year (p=0.625).
In case of combined data of year 2009 and 2014 (2009+2014 for short) and separate data of 2009, there was no statistically significant difference; 1,123 male (96.1%) and 1,250 female patients (97.4%) in 2009+2014 and 490 male (96.8%) and 496 female patients (96.3%) in 2009 revisited after skin biopsy. However, in 2014, 633 male patients (95.6%) returned as compared to 754 female patients (98.0%) did and it was statistically significant difference (p=0.008). Breslow-Day test also showed statistically significant difference by yearly sexual difference (p=0.034).
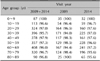
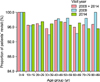
There was no significant difference of average age (mean±standard deviation) between the patients who revisited and who did not in 2009 (43.9±17.8 years vs. 45.9±20.6 years), 2014 (53.5±20.3 years vs. 49.1±21.0 years), and 2009+2014 (49.2±19.7 years vs. 47.8±20.9 years). Considering age group revisits, age between 0 and 9 showed complete revisit ratio (100.0%) in both 2009 and 2014 (Table 6, Fig. 1). Otherwise, there was no consistent trend of return visit ratio according to age groups.
There was statistically significant difference between punch biopsy and shave or excisional biopsy in 2009 (p=0.000); while almost all the patients with punch biopsy (781/797, 98.0%) returned, only 205 of 224 patients (91.5%) who had taken shave or excisional biopsy came back to clinics. Results for 2009+2014 also showed a significant difference, less patients with shave or excisional biopsy (486/518, 93.8%) revisited compared to patients with punch biopsy (1,887/1,934, 97.6%). Breslow-Day test also showed that this temporal trend has significant difference (p=0.036).
In 2009+2014, there was no significant difference of return visit ratio between benign (2,261/2,337, 96.7%) and malignant (112/115, 97.4%) lesions (p=0.703). Similar aspects were observed in 2009 and 2014, separately.
Considering seasonal revisits, in 2009+2014, 537 patients (97.6%) in spring, 660 patients (95.9%) in summer, 603 patients (96.8%) in autumn, and 573 patients (97.0%) in winter came back to clinics after skin biopsy. In 2009, there were 228 patients (96.6%) in spring, 275 patients (95.8%) in summer, 231 patients (97.9%) in autumn, and 252 patients (96.2%) in winter who returned and in 2014, 309 patients (98.4%), 385 patients (96.0%), 372 patients (96.1%), 321 patients (97.6%), respectively. Except autumn in 2009, relatively more patients tended to visit again after skin biopsy in spring and winter, but it had no significant difference (Fig. 2).
There were three critical patients with malignancy or malignancy suspected lesion who did not return to dermatology clinics. The first patient was a 76-year-old woman who consulted to the dermatology clinic regarding multiple papules in the neck that had occurred during treatment and follow-up at the hemato-oncology clinic. Her pathology test results indicated leukemia cutis due to T-cell large granular lymphocytic leukemia. She did not revisit the appointed dermatology clinic, but later continued treatment at Internal Medicine via radiation therapy based on the pathology test results. The second patient was a 59-year-old man who visited our department because of a nodular lesion in the right finger that had recurred after a surgical removal at another hospital. After biopsy at our department, the patient received the test results of proliferation of spindle cells with a mitotic index of 4 mitotic figures per 10 high power fields requiring a complete resection at the plastic surgery department and the physician recommended surgical resection but the patient did not comply with the follow-ups. The third patient was a 79-year-old man with erythematous plaque, nodules, and papules in the scrotum and penis region. His pathology test indicated extramammary Paget's disease. After the biopsy, the patient did not revisit the dermatology clinic at his scheduled appointment, and he did not seek treatment. He revisited one year later when the lesion became aggravated. We referred the patient to urology and he underwent a wide resection.
In 2000, a report was published by the Institute of Medicine addressing the situation regarding patient safety and suggesting some improvements2. This has sparked societal interest in patient safety. Medical errors, such as medication errors, surgical errors, anesthetic errors, intra-hospital infections, fall injuries, and misdiagnoses, are critically related to patient safety. Such mistakes may result from errors in medical judgment, procedures, or equipment, as well as in physician-patient communication.
Therefore, it is essential that the physician communicate effectively with the patient, not only to ensure the quality of health management, but also to improve the patient's health outcomes5. In dermatology clinics, skin biopsies are critically important in cases where definitive diagnosis cannot be made on the basis of the patient's medical history and clinical findings alone. The procedure is also essential in determining treatment direction and consultation with the patient. In other countries such as America and Britain, more than half of patients who had undergone a skin biopsy to diagnose potential malignant tumors preferred to receive the results through the quickest method (phone consultation)6 and 30% of patients suffered from mental stress waiting for the results, regardless of whether the tumor is malignant or not7. Therefore, timely and prompt delivery of pathology test results is essential in terms of patient safety. However, skin biopsies inevitably involve the following processes: slide production, pathologist's reading and findings, and delivery of these findings to the dermatology clinic. Subsequently, the results can be relayed to the patient. In the past, it was difficult to view and track the test procedures performed by medical staff, because all medical information was recorded on paper89. Our hospital computerized all medical records in 2010, but the efficiency of electronic system has not yet been surveyed.
About 1.4 times more patients received a skin biopsy in 2014 than in 2009. The Ministry of Health and Welfare ranked skin and subcutaneous diseases as the 6th highest in prevalence in both 2009 and 201410; this trend is reflected by the growing interest in skin and skin diseases that has come with the increase of quality of life and advances in society.
In the present study, the proportion of patients who revisited after skin biopsy was about 97%—higher than in another study from a dermatology clinic at a tertiary hospital in Israel, where the proportion of patients who revisited increased from 90% to 97% only after the hospital had implemented measures to enhance the quality of medical care. This included patient education through face-to-face instruction by medical staff emphasizing how important it is that pathology test results are delivered to patients, and that patients revisit the hospital. Moreover, the Israeli hospital implemented a computerized system to enable medical staff to regularly monitor test results within two weeks3.
The proportion of patients who revisited depended on certain factors. First, in 2014, a higher proportion of women than men revisited. Choi et al.11 reported that about 90% of Koreans have heard about skin cancer, and that women are about twice as aware of the illness as men. Coupled with the growing interest in dermatological disorders over time, this may have contributed to the higher revisit ratio among women. In addition, they may want a more definitive diagnosis of skin cancer or other skin disorders, and they wish to consult with their physicians regarding treatment procedures. Second, the revisit ratio also differed significantly in terms of the method of skin biopsy. In 2009, the revisit ratio was lower when either a shave biopsy or an excisional biopsy was performed and the entire lesion was removed. However, there was no such difference in 2014. This implies that patients were more focused on the removal of lesions in the past, and that over time they have become more interested in an accurate diagnosis of their skin disorders. Several changes were made in our hospital between 2009 and 2014. First, electronic medical record system was introduced to our hospital in January 2010. Such system enabled medical staff to immediately confirm which medical care or test procedures were performed and to view test results quickly without additional processes. Second, our hospital also had implemented an automated text message system to remind patients of their revisit schedules since 2010. This automated notification system was not specific for dermatology clinic, but generalized for patients who had been scheduled for visiting our hospital. The message is sent 3 days before scheduled date, and it included date, time, clinic department and name of attending clinician in Korean. Statistical analysis of the 2009 and 2014 data did not show a significant difference in the revisit ratios; however, the absolute numbers of patients who did not revisit in 2009 and 2014 were similar, even though the number of patients who underwent skin biopsy in 2014 had increased by 1.4 times. This implies that the automated message systems may have contributed to patient revisits to a certain extent, but additional studies would be required to confirm such conclusions.
There were three crucial patients who did not revisit the dermatologic clinic even though their lesions required further management. Fortunately, two of them were able to receive the test results through medical staff at different departments. However, in the case of the third patient, the test results were not delivered to the patient and the hospital had failed to track him, which undermined his safety with his aggravated condition that might have caused treatment difficulties. Therefore, we recommend an organized system to ensure more rigorous management of patient safety; (1) recording patients' medical record number, test date, and biopsy method in the biopsy records that the department itself manages, and (2) regularly recording the pathology test results and patients' revisit status. A computerized biopsy records would be much easier for staffs to administer, in this case. In addition to these internal efforts by the dermatology clinic, additional measures by the hospital should be considered, such as an automated text messaging system which not only reminds patients of simple schedule but also notifies of the presence of tests results to be delivered. Furthermore, an automated system can also inform attending physicians of critical abnormal findings in the biopsy results.
Some of the limitations of this study include simplified comparison between benign and malignant lesions. A part of benign skin lesions such as actinic keratosis need further treatment and patient should know their real nature. However, as criteria for simple benign lesions and the others requiring further treatment are practically subjective and variable, we classified according to existence of atypical or malignant cells. We could not investigate the attitude of the patients or their caregivers to the system due to the retrospective study design and further studies are required.
In conclusion, this study analyzed 2,452 patients who took skin biopsy at our dermatology clinics in 2009 and 2014 for revisit ratio after skin biopsy and influencing factors. Most of patients (96.8%) returned clinics and their pathology results were delivered. Whereas sex and the method of skin biopsy influenced revisit ratio, age at biopsy, date, and pathology test results did not make significant difference. Female patients or patients with partial lesion removal through biopsy were more willing to revisit after skin biopsy. There were critical cases that failed in result delivery and follow-up in our department, which required improvement from the perspective of patient safety. In addition to dermatologists' own efforts, improved computerization system of the hospital enabling to trace test results should be considered for better patient management.
Figures and Tables
Table 1
Demographic characteristics of the participants
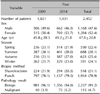
Table 2
Distribution of patients' revisit after skin biopsy (2009 and 2014 year)

Table 3
Distribution of patients' revisit after skin biopsy (2009 year)

Table 4
Distribution of patients' revisit after skin biopsy (2014 year)

Table 5
Breslow-Day test for homogeneity of the odds ratio between 2009 and 2014 year

| Variable | Revisit | |
|---|---|---|
| χ2 | p-value | |
| Sex | 4.512 | 0.034 |
| Biopsy method | 4.414 | 0.036 |
| Pathology result | 0.021 | 0.885 |
Table 6
Distribution of revisit and its ratio according to age groups
ACKNOWLEDGMENT
We would like to appreciate Dr. Sohee Oh, who helped us with data analysis and statistics.
References
1. Hansen TJ, Lolis M, Goldberg DJ, MacFarlane DF. Patient safety in dermatologic surgery: part I. Safety related to surgical procedures. J Am Acad Dermatol. 2015; 73:1–12. quiz 13-14.
2. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, D.C.: National Academy Press;2000. p. xxi. p. 287.
3. Topol P, Porat N, Zelker R, Ingber A, Zlotogorski A, Brezis M. Quality improvement program to assure the delivery of pathology test results: a systemic intervention in a large general hospital. Dermatol Nurs. 2007; 19:253–257.
4. Ting TV, Kudalkar D, Nelson S, Cortina S, Pendl J, Budhani S, et al. Usefulness of cellular text messaging for improving adherence among adolescents and young adults with systemic lupus erythematosus. J Rheumatol. 2012; 39:174–179.

5. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995; 152:1423–1433.
6. Choudhry A, Hong J, Chong K, Jiang B, Hartman R, Chu E, et al. Patients' preferences for biopsy result notification in an era of electronic messaging methods. JAMA Dermatol. 2015; 151:513–521.

7. Al-Shakhli H, Harcourt D, Kenealy J. Psychological distress surrounding diagnosis of malignant and nonmalignant skin lesions at a pigmented lesion clinic. J Plast Reconstr Aesthet Surg. 2006; 59:479–486.

8. Boohaker EA, Ward RE, Uman JE, McCarthy BD. Patient notification and follow-up of abnormal test results. A physician survey. Arch Intern Med. 1996; 156:327–331.

9. Poon EG, Gandhi TK, Sequist TD, Murff HJ, Karson AS, Bates DW. “I wish I had seen this test result earlier!”: Dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004; 164:2223–2228.
10. Ministry of Health and Welfare. Statistical research of trends of the number of daily visiting patients to outpatient clinics in 2009 and 2014; by year and by disease diagnosed [Internet]. Daejeon: Ministry of Health and Welfare;2016. 03. 30. updated 2015. cited 2016 Mar 30. Available from: http://kosis.kr.
11. Choi YL, You SA, Lee DY, Lee JH, Yang JM, Lee ES, et al. A survey of awareness, knowledge and behavior regarding skin cancer in Korea. Korean J Dermatol. 2006; 44:405–419.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download