Abstract
Background
The Koebner phenomenon (KP) is a common entity observed in dermatological disorders. The reported incidence of KP in vitiligo varies widely. Although the KP is frequently observed in patients with viltiligo, the associated factors with KP has not been established yet.
Objective
The aim is to estimate the prevalence of KP in vitiligo patients and to investigate the associated factors with KP among vitiligo characteristics.
Methods
A cross-sectional observational study was conducted using 381 vitiligo patients. Demographic and clinical information was obtained via the completion of Vitiligo European Task Force (VETF) questionnaires. Patients with positive history of KP were extracted from this vitiligo database. Multivariate analysis was performed to assess associations with KP.
Results
The median age of cases was 24 years (range, 0.6~76). In total, 237 of the patients were male (62.2%). Vitiligo vulgaris was the most common type observed (152/381, 39.9%). Seventy-two percent (274/381) patients did not exhibit KP, whereas 28.1% (107/381) of patients exhibited this condition. Multivariable analysis showed the following to be independent factors with KP in patients with vitiligo: the progressive disease (odds ratio [OR], 1.82; 95% confidence interval [95% CI], 1.17~2.92; p=0.041), disease duration longer than 5 years (OR, 1.92; 95% CI, 1.22~2.11; p=0.003), and body surface area more than 2% (OR, 2.20; 95% CI, 1.26~3.24; p<0.001).
Vitiligo is a disease that causes loss of skin pigmentation wherein epidermal melanocytes lose their function. The incidence of vitiligo worldwide is approximately 0.5% to 4%1.
Lesions at physical injury areas in normal/unaffected skin of patients with cutaneous diseases are referred to as Koebner phenomenon (KP)2. KP is the well-known phenomenon in dermatology3. However, its pathogenesis has not been elucidated to date2. KP is recognized in many diseases, such as vitiligo, lichen planus, psoriasis, and Darier's disease23. The prevalence of KP in vitiligo differs widely, and it is reported to occur in 21% to 62% of patients4.
Clear evidence regarding the pathophysiology and clinical consequences of KP in vitiligo is sparse. We aimed to study the prevalence of KP in our vitiligo patients. Moreover, we sought to observe different associations with this response and to find out whether KP is associated with disease severity, duration, type of vitiligo and other factors.
A cross-sectional observational study was conducted using vitiligo patients attending the Department of Dermatology at King Khalid University Hospital in Riyadh. In total, 381 patients with all types of vitiligo were enrolled; patients of various ages from both genders were enrolled from January 2010 to December 2015. Full history and physical examination were completed and documented. Vitiligo European Task Force (VETF) questionnaires5 were completed by the patients who attended the clinic. These questionnaires covered a broad range of demographic and clinical information, including gender, age, type of vitiligo (focal, segmental, mixed, acro facial, mucosal and vulgaris), site of onset of the disease (face, neck, upper limbs, lower limbs, chest and abdomen, back, lip tip, scalp, genitalia and fingers), KP, presence of halo naevi, leukotrichia, family history of vitiligo, and family history of premature hair graying.
There is no consensus or laboratory test to determine the clinical activity of vitiligo. According to the literature, vitiligo has been classified as being stable when further progression of lesions or development of new lesions has been absent for the past year3.
Multivariate analysis was performed to assess various associations, such as total body surface area (BSA), status of disease progression, family history of vitiligo, presence of halo nevus, leucotrichia and other diseases associated with KP. Official approval was obtained from King Khalid University Hospital's Ethical Committee (E-16-2189).
The data was entered and analyzed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). Median+inter-quartile range (IQR) is provided for quantitative variables. Frequencies and percentages were obtained for qualitative variables. The Mann Whitney U test was applied to compare median differences among groups. Data normality was assessed using the Shapiro Wilk test. The Pearson chi-square and Fisher's exact tests were applied to observe associations between qualitative variables. Binary logistic regression analyses was also performed to observe the odds ratios (ORs) in various study parameters. A p-value of <0.05 was considered statistically significant.
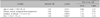
A total of 381 cases of vitiligo were included in this study. Descriptive statistics are provided in Table 1. The median age of cases was 24 years and ranged from 0.6 to 76 years. The median onset age was 13 years and ranged from 0.5 to 72 years. The majority of the cases were males (237, 62.2%) compared with females (144, 37.8%). The most common type of vitiligo was vitiligo vulgaris, which was present in 152 (39.9%) of cases. Segmental vitiligo (SV) was present only in 8 patients (2.1%). Face and lower limb served as the site of vitiligo onset in approximately 25% of cases each. A significant number of patients (178, 46.7%) had a family history of vitiligo. Approximately 227 (59.6%) of cases had an initial single lesion. KP (by history) was reported in 107 (28.1%) of cases.
Age (p=0.019), BSA% (p<0.001) and disease duration (p=0.011) were significantly increased in cases with KP compared with cases without KP. Leukotrichia was more frequently observed in patients without KP (p=0.044). Family history of vitiligo, halo nevi and family history of premature grey hair were not significantly associated (p>0.05). No significant association was seen between males 64 compared with females 43; p>0.05). Disease progression and KP were also significantly associated (p=0.013). Regarding the vitiligo type, the focal type (76 cases, 27.7%) was commonly observed in patients without KP (p=0.008), whereas mixed vitiligo (22 cases, 20.6%) was more frequently observed in cases with KP (p=0.010). The comparison of KP with clinical presentation is presented in Table 2.
Logistic regression analyses of KP (yes/no) for patient characteristics are presented in Table 3. Disease activity (progressive) (OR, 1.82; 95% confidence interval [95% CI], 1.17~2.92; p=0.041), disease duration longer than 5 years (OR, 1.92; 95% CI, 1.22~2.11; p=0.003) and BSA more than 2% (OR, 2.20; 95% CI, 1.26~3.24; p<0.001) were significantly associated with KP.
The KP is a renowned phenomenon in dermatology. This condition is defined as “the development of lesions at sites of distinctively traumatized uninvolved skin of patients with cutaneous diseases.”26 KP occurs in 21% to 62% of patients with vitiligo347. The clinical importance of KP is still not absolutely understood; however, a positive Koebner reaction could be a predictor of subsequent disease activity78. Only limited data have been published to support this hypothesis8.
To date, the exact etiopathogenesis of KP in vitiligo remains unknown; however, multiple mechanisms, including immunological, neural and vascular factors that ultimately lead to depigmentation, are suggested9.
The concept of KP as a sign of more active or extensive vitiligo or as a risk factor of a reduced therapeutic response remains vague. In this study, the clinical profile of vitiligo patients with KP was compared with patients without KP. To our understanding, this comparison has not been described in the Arab population to date. Several significant differences were observed between patients with or without signs of KP, thus potentially providing guidelines for answering patients' questions with regard to prognosis and treatment response.
In a previous study5, a history of KP was apparent in 30.4% of 217 patients of the VETF paper based on the question: ‘Is there any depigmentation on scars (Koebner phenomenon)?’5 Using the same question, our study revealed that KP was present in 107/381 (28.1%) of patients. In an Indian study10, patients with KP exhibited a notably older age of onset and a reduced duration of illness. Of 1,416 patients studied, 94 (6.6%) had KP. Of these, 80 (85.1%) had NSV, and 8 (8.5%) had SV. Thus, KP was observed in 7.1% of patients with NSV and 7.8% of patients with SV. Patients exhibiting KP had a drastically older age at onset of vitiligo (17.7±15.0 years vs. 14.47±14.11 years; p<0.01) and a reduced illness duration (6.49±7.45 years vs. 8.69±10.07 years; p=0.02) compared with those without KP. KP was significantly associated with the primary site of involvement, with legs being the most common site (28.9% of patients) followed by the face (20%) and hands (15.6%) (p<0.001, v2 test) possibly because these sites are more at risk of trauma. In contrast, patients with KP in our study had a longer duration of illness but an older age of onset.
Our results indicate that males more frequently exhibit KP 64/107 (59.8%) than females 43 (40.2%). However, no significant difference between gender and KP was noted (Table 2). In contrast, a study concluded that women are more prone to have KP (KP1 and KP2A) than men8. The same study suggested that the affected BSA was significantly increased in the presence of any KP subtype (p=0.038)8. Our results supported the previous findings that patients with KP also demonstrated an increased affected BSA (OR, 1.83; p=0.016); however, in contrast to our study, this study did not classify BSA as >2% and ≤2% (Table 3). Interestingly, leukotrichia was more frequently observed in our patients without KP manifestation (p=0.044), for which the pathological link should be explored in future studies.
Three different types of KP are reported. The patient's history [KP type 1 (KP1)], clinical examination [KP type 2A/B (KP2A: lesions on friction areas; KP2B: linear], artefactual lesions and experimental induction [KP type 3 (KP3)]). KP3 is mainly restricted to clinical trials, while KP1 and KP2A and B can be used in daily practice9. In this study, patients with positive history of KP were extracted from our vitiligo database.
Frequency of KP occurrence based on vitiligo clinical form was noted as 31% for vulgaris11 and 5.3% for segmental12 disease; no data are available regarding the association between KP and acrofacial vitiligo. Interestingly, another study13 revealed a parallel pattern of KP distribution among vitiligo vulgaris. This finding is in accordance with our results that indicate that KP is more prevalent in vitiligo vulgaris (p=0.033)
In our multivariate analyses, active progressive disease was positively associated with positive KP (OR, 1.8; p=0.02). Moreover, disease duration longer than 5 years was significantly more associated with positive KP (OR, 2.3; p<0.0001). These findings again are in accordance with the fact that KP is an indicator of active disease.
In the present study, the group manifesting KP had a significantly higher median age compared with those without KP which is not reported before. But here we did not find any association of KP with early age of onset. This is in contrast to previous reports which tend to occurred more in early age of onset of disease3. One possibility involves the genetic differences between the two populations. Other differences include the lack of association between the presence of KP and its diverse subtypes. Additionally, factors, such as atopy and autoimmune diseases, could be implicated. This difference might be attributed to the generally low frequency of disease associations in our study cohort, which in turn could be to a certain extent ascribed to the fact that the diagnosis of KP in our study was exclusively based on history.
The observed differences between vitiligo patients with KP and vitiligo patients without KP indicates possible underlying differences in disease activity status. Patients with KP more likely have active vitiligo and are more prone to develop further depigmentation despite treatment. These clinically based associations should be confirmed by larger epidemiological and pathological studies to better understand the etiopathogenesis of and therapeutic options for vitiligo.
In conclusion, this study reveals a direct relation between KP and other clinical signs of vitiligo, such as BSA, duration of disease, and disease activity, among others.
The scarcity of local literature regarding KP is an opportunity for prospective research with a proposed redefinition of KP in vitiligo as outlined via the consensus of the VETF group. Future studies involving larger numbers of patients will help to further explain the clinical characteristics of KP.
Figures and Tables
Table 1
Descriptive and clinical presentation of vitiligo patients (n=381)

Table 2
Clinical presentation of vitiligo associated with Koebner phenomenon (n=107)

Table 3
Mutivariate logistic regression for factors associated with Koebner phenomenon in vitiligo patients (n=107)
ACKNOWLEDGMENT
The project was financially supported by Vitiligo Research Chair, King Saud University, Vice Deanship of Research Chairs, Deanship of Scientific Research.
References
1. Gawkrodger DJ, Ormerod AD, Shaw L, Mauri-Sole I, Whitton ME, Watts MJ, et al. Vitiligo: concise evidence based guidelines on diagnosis and management. Postgrad Med J. 2010; 86:466–471.

2. Morais P, Oliveira M, Matos J. Striae: a potential precipitating factor for Koebner phenomenon in psoriasis? Dermatol Online J. 2013; 19:18186.

3. van Geel N, Speeckaert R, Taieb A, Picardo M, Böhm M, Gawkrodger DJ, et al. Koebner's phenomenon in vitiligo: European position paper. Pigment Cell Melanoma Res. 2011; 24:564–573.

4. Barona MI, Arrunátegui A, Falabella R, Alzate A. An epidemiologic case-control study in a population with vitiligo. J Am Acad Dermatol. 1995; 33:621–625.

5. Taïeb A, Picardo M. VETF Members. The definition and assessment of vitiligo: a consensus report of the vitiligo European task force. Pigment Cell Res. 2007; 20:27–35.

8. van Geel N, Speeckaert R, De Wolf J, Bracke S, Chevolet I, Brochez L, et al. Clinical significance of Koebner phenomenon in vitiligo. Br J Dermatol. 2012; 167:1017–1024.
9. van Geel N, Speeckaert R, Mollet I, De Schepper S, De Wolf J, Tjin EP, et al. In vivo vitiligo induction and therapy model: double-blind, randomized clinical trial. Pigment Cell Melanoma Res. 2012; 25:57–65.

10. Kanwar AJ, Mahajan R, Parsad D. Koebner phenomenon in vitiligo in an Indian population. Clin Exp Dermatol. 2013; 38:554–555.

11. Hann SK, Lee HJ. Segmental vitiligo: clinical findings in 208 patients. J Am Acad Dermatol. 1996; 35:671–674.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download