Abstract
Background
Herpes zoster (HZ) is caused by reactivation of latent varicella-zoster virus (VZV) infection. HZ-associated aseptic meningitis, a rare complication of HZ, can require hospitalization and a long treatment period.
Objective
A retrospective study was performed to identify potential factors associated with HZ-associated aseptic meningitis development.
Methods
We included all outpatients and patients admitted in the neurology and dermatology departments of a single tertiary center, who were diagnosed with HZ for two years. Among 818 patients, 578 patients were eligible for analysis.
Results
The demographics and potential risk factors were compared between the uncomplicated HZ group (n=554) and aseptic meningitis group (n=24). Among the potential factors, the dermatological distribution of skin rash and gender showed statistically significantly different between the two groups. Patients with craniocervical distribution of HZ accounted for 87.5% (n=21) of the aseptic meningitis group and 54.3% (n=301) of the uncomplicated HZ group (p=0.043). The aseptic meningitis group had more men (66.7%, n=16) than the uncomplicated HZ group (42.8%, n=237, p=0.033). Patients with craniocervical distribution had an odds ratio (OR) of 5.884 (p=0.001) for developing aseptic meningitis when compared with the other dermatome involvements. Additional logistic regression analysis resulted in a fading between gender difference (p=0.050) and craniocervical involvement having an OR of 5.667 for aseptic meningitis (p=0.006).
Herpes zoster (HZ) is a disease caused by reactivation of the latent varicella-zoster virus (VZV) that remains latent in the dorsal root and cranial nerve ganglia; this latency is known to be life-long12. Once reactivated, the virus spreads along the involved nerves and the corresponding cutaneous dermatome. The incidence of HZ has increased in the last two decades: 3.6 per 1,000 person-years in the United States, with an increase from 3.2 to 4.1 per 1,000 person-years from 1996 to 20013.
Numerous complications have been associated with HZ, including postherpetic neuralgia, meningitis, myelitis, encephalitis, and arteritis4. In a previous study of 859 patients with HZ, the postherpetic neuralgia occurred in 7.9% within 60 days of the onset of HZ; superinfection, 2.3%; ocular complications, 1.6%; motor neuropathy, 0.9%; meningitis, 0.5%; and HZ oticus, 0.2%5. Old age and comorbid conditions that may impair cell-mediated immunity including diabetes, cancer, connective tissue disease, chronic obstructive pulmonary disease, inflammatory bowel disease, human immunodeficiency virus infection, organ transplantation, and psoriasis have been reported to be associated with higher risk of complications in HZ patients5. HZ-associated aseptic meningitis is considered a rare complication of HZ, and it usually requires hospitalization and a long period of treatment.
Clinically, HZ-associated aseptic meningitis is relatively common in comparison to other complications involving the central nervous system. In HZ patients with headaches accompanied by nausea, vomiting, neck stiffness, fever or chills complicated meningitis should be suspected. It is thought that the involvement of cranial nerves may contribute to a higher risk of aseptic meningitis. In a previous report of patients with systemic cancer, cases of HZ-associated meningoencephalitis, although small in number, were all associated with trigeminal or disseminated zoster6. However, the clinical characteristics and potential risk factors that may predispose patients with HZ to complicated aseptic meningitis have been poorly studied. The aim of this study was to identify the possible risk factors and related clinical characteristics in patients with HZ for developing HZ-associated aseptic meningitis.
This retrospective study was based on a review of electronic medical records from patients diagnosed with HZ. This study was approved by the institutional review boards of Chonnam National University Hospital (IRB no. CNUH-2015-150).
We included all outpatients as well as all patients admitted in the neurology and dermatology departments of a single tertiary centre who were diagnosed with HZ in 2013 and 2014. A total of 818 patients were initially included. After the electronic medical records were thoroughly reviewed, 578 patients were eligible for analysis as the excluded 240 cases lacked a definite diagnosis or had insufficient medical records for analysis. Dermatologists examined skin lesions including Tzanck smears. Patients with symptoms of headache, fever or meningeal irritation signs were suspected to have meningitis and underwent spinal tapping for evaluation of the cerebrospinal fluid (CSF). Among the medical records, data pertaining to age, gender, involved dermatomes, and other medical conditions (hypertension, diabetes mellitus, pregnancy, concurrent malignancy, liver cirrhosis, chronic kidney disease, and immunosuppressant use) were used for evaluation and analysis.
HZ was diagnosed by dermatologists in patients with characteristic distribution and appearance of skin lesions accompanied by localized pain. Tzanck smear was utilized to support the diagnosis of HZ. HZ-associated aseptic meningitis was defined as follows: 1) signs and/or symptoms of meningeal irritation without brain parenchymal involvement in patients within 4 weeks of HZ diagnosis; 2) CSF leukocyte count over 5×106/L; 3) a negative CSF stain and culture for bacteria, tuberculosis, and fungus; and 4) no other explainable non-infectious aetiology.
Descriptive statistics were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Fisher's exact test and bimodal logistic regression were used in the analysis of the collected data. All tests performed were two-tailed and differences were considered significant at p<0.05.
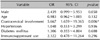
The demographics and potential risk factors were compared between the uncomplicated HZ group (n=554) and HZ-associated aseptic meningitis group (n=24) (Table 1). The mean age was 56.8 years in the uncomplicated group, and 51.1 years in the aseptic meningitis group. The aseptic meningitis group was 5.7 years younger; however, this difference was not significant (p=0.296). Age stratification showed that patients over the age of 60 years accounted for half of the uncomplicated HZ group and the aseptic meningitis group (49.9% and 50.0% respectively). Among the potential risk factors, the dermatological distribution of skin rash and gender were significantly different between the two groups. Patients with craniocervical distribution of HZ accounted for 87.5% (n=21) of the aseptic meningitis group and 54.3% (n=301) of the uncomplicated group (p=0.043). When a comparison was made between craniocervical distributions versus the rest, patients with craniocervical distribution had an odds ratio of 5.884 (95% confidence interval [CI], 1.735~19.953; p=0.001) for developing HZ-associated aseptic meningitis. The aseptic meningitis group had a higher proportion of men (66.7%, n=16) than the uncomplicated group (42.8%, n=237, p=0.033). The frequency of hypertension, diabetes mellitus, use of immunosuppressants, and concurrent malignancy or hematologic disorder was not significantly different between the two groups. The frequency of liver cirrhosis and chronic kidney disease was also insignificant (Table 1). The interval between onset of HZ and symptoms of meningitis was 5.3 days in average, ranging from 0 to 30 days. In 20 of the cases (83.3%), the meningitis symptoms manifested within 6 days from onset of HZ skin lesions.
To adjust for confounding effects, logistic regression analysis was performed. The gender difference between the two groups faded (95% CI, 0.999~5.953; p=0.050) and the craniocervical involvement had an odds ratio of 5.667 for the complication of aseptic meningitis (95% CI, 1.659~19.365; p=0.006) (Table 2). Among the craniocervical dermatomes, the V1 trigeminal dermatome was most frequently involved in the meningitis group (p=0.003) with 4-fold increased risk (OR, 4.4; 95% CI, 1.756~11.048; p=0.002) compared to the involvement of other dermatomes.
In this retrospective study of the potential risk factors for the development of aseptic meningitis in patients with HZ, patients with skin lesions on craniocervical distribution had higher odds for the development of HZ-associated aseptic meningitis. Among the trigeminal branches, the involvement of the ophthalmic branch (V1) was associated with higher risk of complicated meningitis. In a previous study by Galil et al.5, the involvement of the V1 dermatome increased the risk of developing any complication in HZ patients, which is more or less consistent with our finding. The association between skin lesions with craniocervical distribution and aseptic meningitis has been described in a previous report on systematic cancer patients, in which all patients with meningoencephalitis had trigeminal or disseminated zoster6. This relation can be explained by considering the anatomical distance between the brain meninges and the region of the involved dermatome. A closer anatomical distance may facilitate viral invasion to the brain meninges and cause clinical symptoms of meningitis. A previous case of a HIV-positive VZV meningoencephalitis patient showed histopathological evidence of necrotizing vasculitis predominant in the meninges in postmortem autopsy7. This finding indicates that vasculitis is a pathogenic mechanism in meningitis associated with VZV, and hematogenous invasion the virus may play a role in CNS VZV infections. Another previous study revealed CSF findings in 46 patients with HZ that 21 patients presented with leukocytosis and one-third had positive PCR results for VZV or anti-VZV IgG within the first week, after the onset of skin lesions8. These findings demonstrate that subclinical invasion of CSF by VZV seems common. Therefore, the increased risk with craniocervical involvement cannot solely be attributed to the anatomical proximity.
In a previous retrospective analysis of central nervous system VZV reactivation, 71% of aseptic meningitis cases were noted in male patients9. In regards to the study of HZ prevalence, a Swedish analysis revealed a female predominance10, and a systematic review of European data by Pinchinat et al.11 also reported higher incidence rates in female patients. In the current study, 56.2% of the total HZ cases were noted in women and although not statistically significant, male predominance in the aseptic meningitis group was observed. Female predominance is a trend for HZ, but the complication rate of HZ-associated aseptic meningitis is higher in male patients. This is presumed to be due to immunological and hormonal differences between genders. Further study is needed to clarify the relationship between gender and incidence of HZ-associated aseptic meningitis and the underlying mechanisms contributing to this difference.
HZ-associated aseptic meningitis accounted for 4.15% of the total HZ cases in our study, which is higher than the previous report: 0.5%5. This may be due to the increasing proportion of the elderly population, resulting in older HZ patients who bear higher risk of complications. In our study, however, the mean age was younger in the aseptic meningitis group (51.1 years vs. 56.8 years in the uncomplicated HZ group). The relatively small number of the meningitis patients (24 cases) compared with the other group (554 cases) may have contributed to the contradictory age difference between the two groups. A larger sample size may yield a contrasting result. Immunosuppression is associated with increased risk of not only HZ and its complications3121314. Our results did not show significant difference in immunocompromised hosts, which include patients with concurrent malignancy, hematologic disease, or chronic immunosuppressant use, between the uncomplicated HZ group and the Hz-associated aseptic meningitis group. These results may be indicating reduced incidence of HZ complications in immunocompromised population of our study, probably due to active diagnosis and early antiviral treatment at initial stage of HZ in these patients and increased prophylactic use of antiviral agents especially in patients undergoing hematopoietic cell transplantation15. Previous comorbidities or medical conditions (hypertension, diabetes mellitus, pregnancy, liver cirrhosis, and chronic kidney disease) were not significantly associated with HZ-associated aseptic meningitis in the current study. Although patients with chronic kidney disease have been reported to have a higher risk for HZ compared to the general population1617, the association between complicated aseptic meningitis and chronic kidney disease was not significant. Future study with a larger sample size may reveal significance of the previously mentioned comorbidities in relation to HZ-associated meningitis.
The strength of our study is that we enrolled a relatively large number of patients for analysis. However, there are also several limitations. First, given that this was a retrospective study, the associations observed cannot be considered as definitive evidence of a causal relationship. Further study with a prospective design is needed. Second, 240 patients were excluded from the analysis due to insufficient medical records or lack of proper diagnosis, which may have influenced analysis of the results. Third, the etiology of complicated aseptic meningitis cases was not confirmed by VZV PCR in the current study. Patients with aseptic meningitis caused by other viral agents may have been included in the analysis, as enterovirus is the most common causative pathogen and VZV accounts for only 8% of aseptic meningitis cases in adults18.
In HZ patients, a skin rash with craniocervical distribution is associated with a higher risk of HZ-associated aseptic meningitis. Closer observation is needed to detect signs and symptoms of meningitis in patients with HZ infection with this risk factor. Clinicians should take this information into account when treating patients with HZ.
Figures and Tables
Table 1
Demographics and clinical characteristics of patients with uncomplicated herpes zoster and herpes zoster-associated aseptic meningitis (n=578)

Values are presented as number only, number (%), or mean±standard deviation unless otherwise indicated. HZ: herpes zoster, OR: odds ratio, CI: confidence interval. *Indicates statistical significance, †p-values for the Fisher's exact test, ‡p-values for the Mann-Whitney U test, §Craniocervical involvement vs. others.
Table 2
Relative odds of herpes zoster-associated aseptic meningitis in patients with herpes zoster: logistic regression model
ACKNOWLEDGMENT
All persons who have made substantial contribution, but who are not eligible as authors are named in acknowledgment. This study was supported by a grant from the Brain Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT & Future Planning NRF-2014M3C7A1046041 (to B.K.) and a grant from Chonnam National University Hospital CRI 13902-22.4 (to B.K.).
References
1. Ku CC, Padilla JA, Grose C, Butcher EC, Arvin AM. Tropism of varicella-zoster virus for human tonsillar CD4(+) T lymphocytes that express activation, memory, and skin homing markers. J Virol. 2002; 76:11425–11433.

2. Chen JJ, Gershon AA, Li ZS, Lungu O, Gershon MD. Latent and lytic infection of isolated guinea pig enteric ganglia by varicella zoster virus. J Med Virol. 2003; 70:Suppl 1. S71–S78.

3. Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007; 82:1341–1349.

4. Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med. 2000; 342:635–645.

5. Galil K, Choo PW, Donahue JG, Platt R. The sequelae of herpes zoster. Arch Intern Med. 1997; 157:1209–1213.

6. Hughes BA, Kimmel DW, Aksamit AJ. Herpes zoster-associated meningoencephalitis in patients with systemic cancer. Mayo Clin Proc. 1993; 68:652–655.

7. Kleinschmidt-Demasters BK, Mahalingam R, Shimek C, Marcoux HL, Wellish M, Tyler KL, et al. Profound cerebrospinal fluid pleocytosis and Froin's syndrome secondary to widespread necrotizing vasculitis in an HIV-positive patient with varicella zoster virus encephalomyelitis. J Neurol Sci. 1998; 159:213–218.

8. Haanpää M, Dastidar P, Weinberg A, Levin M, Miettinen A, Lapinlampi A, et al. CSF and MRI findings in patients with acute herpes zoster. Neurology. 1998; 51:1405–1411.

9. Becerra JC, Sieber R, Martinetti G, Costa ST, Meylan P, Bernasconi E. Infection of the central nervous system caused by varicella zoster virus reactivation: a retrospective case series study. Int J Infect Dis. 2013; 17:e529–e534.

10. Studahl M, Petzold M, Cassel T. Disease burden of herpes zoster in Sweden--predominance in the elderly and in women-a register based study. BMC Infect Dis. 2013; 13:586.
11. Pinchinat S, Cebrián-Cuenca AM, Bricout H, Johnson RW. Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis. 2013; 13:170.

12. Antonelli MA, Moreland LW, Brick JE. Herpes zoster in patients with rheumatoid arthritis treated with weekly, low-dose methotrexate. Am J Med. 1991; 90:295–298.

13. Korelitz BI, Fuller SR, Warman JI, Goldberg MD. Shingles during the course of treatment with 6-mercaptopurine for inflammatory bowel disease. Am J Gastroenterol. 1999; 94:424–426.

14. Miller GG, Dummer JS. Herpes simplex and varicella zoster viruses: forgotten but not gone. Am J Transplant. 2007; 7:741–747.

15. Kim DH, Messner H, Minden M, Gupta V, Kuruvilla J, Wright J, et al. Factors influencing varicella zoster virus infection after allogeneic peripheral blood stem cell transplantation: low-dose acyclovir prophylaxis and pre-transplant diagnosis of lymphoproliferative disorders. Transpl Infect Dis. 2008; 10:90–98.

16. Kuo CC, Lee CT, Lee IM, Ho SC, Yang CY. Risk of herpes zoster in patients treated with long-term hemodialysis: a matched cohort study. Am J Kidney Dis. 2012; 59:428–433.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download