Dear Editor:
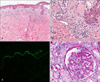
A 45-year-old woman presented with a 5-week history of vesicular eruption over her body. Four years prior, she was diagnosed with Hashimoto thyroiditis with anti-thyroglobulin antibody level, 339 U/ml (reference range, 0~100 U/ml) and anti-microsomal antibody level, 1,296 U/ml (reference range, 0~100 U/ml). She had been taking medication for 3 years, discontinuing it on her own. In addition, she had been taking telmisartan 80 mg/day, amlodipine 5 mg/day, and hydrochlorothiazide 12.5 mg/day for 4 months to control hypertension. Physical examination revealed multiple erythematous collarettes of blisters with intense pruritus on her whole body (Fig. 1). Skin biopsy with direct immunofluorescence (DIF) study was performed on her back. Hematoxylin-eosin staining revealed a subepidermal bulla with mixed inflammatory infiltration in the upper dermis (Fig. 2A, B). The DIF study revealed linear deposition of immunoglobulin (Ig) A along the dermoepidermal junction (Fig. 2C), resulting in the diagnosis of linear IgA dermatosis (LAD). Laboratory test results were otherwise normal except for the following: white blood cell count, 15,000/µl with 85.6% neutrophil concentration; hemoglobin level, 10.8 g/dl; blood urea nitrogen level, 30.6 mg/dl; creatinine level, 1.44 mg/dl; urinary protein level, 55.9 mg/dl; urinary creatinine level, 96.9 mg/dl; urinary protein-to-creatinine ratio, 0.58; and urinary red blood cell count, many per high power field. On referral to the department of nephrology for evaluation, she was diagnosed with IgA nephropathy by kidney biopsy (Fig. 2D). Moreover, further evalution revealed normocytic normochromic anemia with elevated serum ferritin level, implying anemia of chronic inflammation. During 12-month follow-up, the cutaneous lesions had been fairly well controlled with dapsone 50~100 mg/day, with or without colchicine 1.2 mg/day.
LAD is an acquired, autoimmune vesiculobullous dermatosis characterized by subepidermal blisters with deposition of linear homogeneous IgA at the basement membrane. Its pathogenesis is unclear, but associations with malignancies, drugs, and inflammatory diseases, notably ulcerative colitis, have been reported in adults1. Several cases of LAD with IgA nephropathy have been reported in children1, but a few in adults2.
Hashimoto thyroiditis is an autoimmune thyroiditis demonstrating high titers of thyroid antibodies. It is associated with other autoimmune diseases such as Addison disease, type 1 diabetes mellitus, vitiligo, rheumatoid arthritis, or systemic lupus erythematosus. To the best of our knowledge, only one case associated with LAD has been reported3. As they share the autoimmune pathogenesis, regulatory T cells might play a role in LAD and Hashimoto thyroiditis4.
IgA nephropathy is an immune complex-mediated glomerulonephritis characterized by diffuse mesangial IgA deposit, sometimes with IgM, IgG, complement 3, or Ig light chains. IgA in the mesangium is typically of the polymeric IgA1 subclass. Pena-Penabad et al.2 suggested a possible role of the IgA1 subclass in the shared pathogenesis between LAD and IgA nephropathy. Furthermore, in a genome-wide association study of IgA nephropathy, six new genome-wide significant associations were found, most of which were associated with the risk of inflammatory bowel disease5. These loci could be related to LAD, as the association between LAD and ulcerative colitis is well documented.
In conclusion, we report a rare case of concurrent LAD, Hashimoto thyroiditis, and IgA nephropathy.
Figures and Tables
Fig. 1
(A) A 45-year-old woman presented with multiple erythematous collarettes of blisters on her whole body, mainly on the trunk. Note the clustered bullae on the back. (B) New bullae are found adjacent to old bullae, forming a string of beads sign.

Fig. 2
(A, B) Subepidermal bulla with mixed inflammatory infiltration in the upper dermis (H&E, virtual slide view). (C) Linear deposition of immunoglobulin (Ig) A along the dermoepidermal junction (direct immunofluorescence [DIF], ×200). (D) Mild widening of the mesangial matrix with focal and segmental mesangial hypercellularity on renal biopsy (periodic acid-Schiff stain, virtual slide view). The renal DIF study result showed mild IgA, C3, and minimal IgM deposits at the mesangium (not shown).
References
1. Rositto AE, Cobeñas C, Drut R. Linear IgA disease of childhood developing IgA nephropathy. Pediatr Dermatol. 2008; 25:339–340.

2. Pena-Penabad C, Hernández-Vicente I, Hernández-Martín A, García-Silva J, Flores T, Armijo M. IgA mesangial nephropathy and autoimmune haemolytic anaemia associated with linear IgA bullous dermatosis. Br J Dermatol. 1995; 133:146–148.

3. Horiguchi Y, Ikoma A, Sakai R, Masatsugu A, Ohta M, Hashimoto T. Linear IgA dermatosis: report of an infantile case and analysis of 213 cases in Japan. J Dermatol. 2008; 35:737–743.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download