Abstract
Morgellons disease is a rare disease with unknown etiology. Herein, we report the first case of Morgellons disease in Korea. A 30-year-old woman presented with a 2-month history of pruritic erythematous patches and erosions on the arms, hands, and chin. She insisted that she had fiber-like materials under her skin, which she had observed through a magnifying device. We performed skin biopsy, and observed a fiber extruding from the dermal side of the specimen. Histopathological examination showed only mild lymphocytic infiltration, and failed to reveal evidence of any microorganism. The polymerase chain reaction for Borrelia burgdorferi was negative in her serum.
Morgellons disease is a mysterious disease with unknown etiology. It is characterized by fibers appearing in slow- or non-healing skin lesions and even beneath unbroken skin, along with abnormal (crawling, stinging, or biting) sensations of skin. Extracutaneous manifestations (fatigue, joint pain, fibromyalgia, or sleep disorders) have been reported to co-exist1. It has been recognized as a delusional infestation2. However, recent studies are suggesting that it could be associated with an infectious organism: Borrelia burgdorferi34. There have been a number of reports and investigations about Morgellons disease in the US or Europe, but there are none so far in Asia.
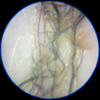
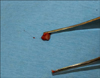
A 30-year-old woman presented with a 2-month history of pruritic cutaneous lesions on the hands and arms. She insisted that she had fiber-like materials under the skin, and could find fiber-like materials when she ripped the skin off. She also complained of a stinging sensation like having a splinter in the fingers. She brought some pictures of the fiber-like materials ‘in situ,’ taken by her using a magnifying device. Twisted black, brown, and red fibers were buried in the skin (Fig. 1). Upon dermatologic examination, multiple erythematous patches and erosions were observed on the arms, hands, and chin (Fig. 2). Dermoscopic examination revealed nonspecific signs. Regarding past medical history, she had been diagnosed with narcolepsy 12 years previously and had taken modafinil and venlafaxine. She wanted us to perform a histopathologic examination to make a proper diagnosis, which was performed on the intact forearm skin. In a gross examination of specimen, a fiber was observed extruding from the dermal side of the specimen (Fig. 3). The skin specimen and fiber was processed by the routine tissue preparation, content of which was not further investigated. Histopathological examination revealed mild superficial perivascular lymphocytic infiltration, but was otherwise normal (Fig. 4). Periodic Acid-Schiff, Grocott's Methenamine Silver, Warthin-Starry stain, and Wright-Giemsa stain were negative. Masson's trichrome stained only dermal collagen. Cytokeratin 5/6 was positive, cytokeratin 7 was positive in skin appendage, and cytokeratin 20 was negative. Tissue culture was negative for microorganisms. In laboratory tests, the white blood cell count was slightly elevated (12.36×103/µl). Thyroid function tests, immunoglobulins (IgG, IgA, IgM), and complements (C3, C4) were within normal limits. B. burgdoferi serology was negative. Considering that a supportive, non-confrontational, and multi-disciplinary approach5 or antipsychotic agents are essential for the treatment of this disease, she was advised to visit the department of psychiatry and to take medication. However, the patient refused follow-up.
Morgellons disease is a controversial subject. One study2 reported that its prevalence was 3.65 per 100,000, with Caucasian predominance. Its main symptom is development of fibers or materials from the skin, with or without cutaneous lesions and abnormal perceptions.
Many studies have classified it as delusions of parasitosis or delusional infestation6. One study5 disclosed that laboratory values associated with infection were normal in Morgellons disease patients, and that cutaneous biopsy specimens revealed only nonspecific findings. Another research2 from the Centers for Disease Control and Prevention reported that there was no common underlying medical condition or infectious organism in Morgellons disease cases, and that the fibers were composed mainly of cellulose. It was also reported that most of them were co-affected by other psychiatric disorders78. It has been reported that hypnotherapy9 or pimozide10 are effective treatments for improving the physical and psychological symptoms.
On the other hand, recent research has advocated that Morgellons disease is a real somatic disorder, related to Lyme disease. Middelveen et al.34 reported that this disorder was associated with spirochetal infection (B. burgdorferi). Culture, histology, immunohistochemistry, electron microscopy, and molecular testing verified that Morgellons disease could be associated with a systemic spirochetal infection3. Also, the filaments detected in the cases were found to have a collagen component, and contain melanin pigment. It was suggested that the presence of spirochetes activated keratinocytes and fibroblasts to express keratin and collagen, respectively11.
In this case, Morgellons disease was considered as a delusional infestation, not as a somatic disease. The histopathologic and immunohistochemistry analysis revealed nonspecific findings without infectious etiologies. The evidence of the black fiber observed in gross specimen was also absent, which was consistent to previous study5. It could be dissolved by the organic solvents used in the tissue preparation process. Serology failed to find any evidence of infection with B. burgdoferi. In addition, the patient in this case had been treated for narcolepsy.
Patients with Morgellons disease lack insight, and are reluctant to be referred to psychiatric physicians. This may impede proper management, and result in dermatologists being the only physicians managing them. Further investigation into Morgellons disease is still needed, and large population studies are required for establishing appropriate treatment methods. We report this case to highlight Morgellons disease for enhancing physicians' consciousness of this disease in Asia.
Figures and Tables
References
1. Savely VR, Leitao MM, Stricker RB. The mystery of Morgellons disease: infection or delusion? Am J Clin Dermatol. 2006; 7:1–5.
2. Pearson ML, Selby JV, Katz KA, Cantrell V, Braden CR, Parise ME, et al. Clinical, epidemiologic, histopathologic and molecular features of an unexplained dermopathy. PLoS One. 2012; 7:e29908.

3. Middelveen MJ, Bandoski C, Burke J, Sapi E, Filush KR, Wang Y, et al. Exploring the association between Morgellons disease and Lyme disease: identification of Borrelia burgdorferi in Morgellons disease patients. BMC Dermatol. 2015; 15:1.

4. Middelveen MJ, Burugu D, Poruri A, Burke J, Mayne PJ, Sapi E, et al. Association of spirochetal infection with Morgellons disease. F1000Re. 2013; 2:25.

5. Robles DT, Olson JM, Combs H, Romm S, Kirby P. Morgellons disease and delusions of parasitosis. Am J Clin Dermatol. 2011; 12:1–6.

6. Söderfeldt Y, Groß D. Information, consent and treatment of patients with Morgellons disease: an ethical perspective. Am J Clin Dermatol. 2014; 15:71–76.

7. Hylwa SA, Foster AA, Bury JE, Davis MD, Pittelkow MR, Bostwick JM. Delusional infestation is typically comorbid with other psychiatric diagnoses: review of 54 patients receiving psychiatric evaluation at Mayo Clinic. Psychosomatics. 2012; 53:258–265.

8. Foster AA, Hylwa SA, Bury JE, Davis MD, Pittelkow MR, Bostwick JM. Delusional infestation: clinical presentation in 147 patients seen at Mayo Clinic. J Am Acad Dermatol. 2012; 67:673.e1–673.e10.

9. Gartner AM, Dolan SL, Stanford MS, Elkins GR. Hypnosis in the treatment of Morgellons disease: a case study. Int J Clin Exp Hypn. 2011; 59:242–249.
10. Reid EE, Lio PA. Successful treatment of Morgellons disease with pimozide therapy. Arch Dermatol. 2010; 146:1191–1193.

11. Middelveen MJ, Mayne PJ, Kahn DG, Stricker RB. Characterization and evolution of dermal filaments from patients with Morgellons disease. Clin Cosmet Investig Dermatol. 2013; 6:1–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download